Abstract
Purpose
Fatal radiation pneumonitis is a rare event. In recent years, higher incidences of grade 5 pneumonitis have been reported. Based on 3 cases in our clinic, a literature review was performed to assess specific clinical features and risk factors for fatal pneumonitis.
Methods and Materials
Three patients with nonsmall cell lung cancer were treated with conventionally fractionated radiation therapy, 2 with volumetric modulated arc therapy and one with intensity modulated radiation therapy. All 3 patients had high volumes of 5 Gy in the total lung and contralateral lungs. Patients died of pneumonitis between 2 and 5 months after the end of radiation therapy. A literature review focused on grade 5 pneumonitis was performed for conventionally fractioned and stereotactic radiation therapy for lung cancer.
Results
Patients with grade 5 pneumonitis develop symptoms sooner than lower grade pneumonitis. Symptoms often do not respond to steroid treatment or return after steroid taper. Imaging features extend beyond the high dose area and involve the contralateral lung. Dosimetric risk factors include both low dose and high dose lung volumes. For patients undergoing stereotactic radiation therapy interstitial lung disease has been described as a risk factor.
Conclusions
Despite decades of investigating radiation pneumonitis, the question of the optimum dose distribution in the lung, a large dose to a small volume versus a small dose to a large volume, is still unresolved. When both low and high dose lung volume constraints are followed, the risk for grade 5 pneumonitis has been shown to be low even with intensity modulated radiation therapy and concurrent chemotherapy. In addition to dose factors, underlying clinical and radiographic parameters play an important role for the development of grade 5 pneumonitis.
Introduction
Radiation pneumonitis (RP) is the most clinically relevant toxicity of radiation therapy to the chest. It affects about 30% of patients with locally advanced lung cancer treated with conventionally fractionated radiation therapy1 and <10% of patients treated with stereotactic body radiation therapy (SBRT) for tumor manifestations in the lung.2 Various factors have been identified to influence the risk of RP. These include treatment-related parameters, such as mean lung dose and lung V20Gy, and combining radiation therapy with chemotherapy. Other factors are tumor size and location, and clinical features such as pulmonary function, smoking history, comorbidities and patient age.1, 2, 3 RP is not only limited to radiation therapy of lung cancer, but has also been observed after the treatment of other chest malignancies, such as breast cancer, esophagus cancer, lymphomas, and in pediatric patients.4, 5, 6, 7
Fatal RP, or grade 5 radiation pneumonitis (G5 RP) per Common Terminology Criteria for Adverse Events, is a tragic event that typically has a low occurrence of about 2% after conventionally fractionated radiation therapy1 and 1% after SBRT.8 Recent reports on rates of G5 RP that are higher than typically expected, even after radiation therapy to small lung volumes with SBRT, demand increased attention to potential risk factors and their combinations. An increased risk of G5 RP has been associated with several factors such as the introduction of advanced radiation treatment techniques, for example, the use of intensity modulated radiation therapy (IMRT) for pleuramesothelioma post extrapleural pneumonectomy9, 10, 11, 12 or lung cancer,13, 14 the presence of underlying lung conditions such as interstitial lung disease,15, 16, 17, 18, 19, 20, 21, 22, 23 and other predisposing conditions.21, 24, 25, 26, 27 We report 3 cases with G5 RP and review the literature to identify common determinants of G5 RP to help prevent fatal outcomes in the future.
Case Reports
Patient A
A 74-year-old white man received a diagnosis of stage IIIB (T4N2M0) squamous cell carcinoma of the lung. The large primary tumor was located in the right lower lobe with right hilar and lower paratracheal lymph node involvement. Medical history included chronic obstructive pulmonary disease, hypertension, coronary artery disease, hyperlipidemia, and hemochromatosis. He had an 80 pack-year smoking history, having quit 12 years before his lung cancer diagnosis. Pulmonary function tests revealed a forced expiratory volume in 1 second (FEV1) of 70% predicted and a diffusion capacity for carbon monoxide (DLCO) of 41% predicted. Karnofsky index (KI) was 80%. Treatment consisted of concurrent carboplatin plus paclitaxel chemotherapy and volumetric modulated arc therapy (VMAT) delivering 60 Gy in 30 fractions with daily cone beam computed tomography (CBCT) for image guidance. The internal gross tumor volume (iGTV) measured 1161 mL, the clinical target volume (CTV) 1468 mL, and the planning target volume (PTV) 2014 mL. The total lung volume CTV was 3731 mL. The dose-volume histogram (DVH) of his lungs (lungs-CTV) showed a volume receiving 5 Gy or higher (V5Gy) of 88% (contralateral lung V5Gy 89%), V10Gy of 70%, and V20Gy of 29%. Mean lung-CTV dose (MLD) was 18.6 Gy. Mean heart dose (MHD) was 22 Gy and heart V60Gy was 2%. Treatment was tolerated well without any ≥G2 toxicities.
On a routine follow-up visit 12 days after end of treatment (EOT), the patient reported cramping in the chest, shortness of breath, fatigue, and some dysphagia. At that time, symptoms were treated symptomatically. Twenty-six days after EOT, the patient presented for a follow-up appointment having symptoms of pleuritic chest pain, shortness of breath, orthopnea, and nonproductive cough; no fevers were reported, and SpO2 was 95%. Computed tomography chest imaging was only remarkable for a possible new metastatic focus in the right upper lobe. After a brief admission he was discharged on a prednisone taper for presumed radiation pneumonitis and pain medication with symptomatic improvement. Three weeks later, while still on steroids, he was readmitted with chest pain and acute hypoxic respiratory failure with SpO2 of 88% requiring treatment with a bilevel positive air pressure machine. His computed tomography imaging at readmission showed diffuse interval ground glass opacity changes and septal thickening, with some bilateral apical sparing and peripheral left lung sparing (Fig. 1). He was started on high-dose methylprednisolone and empirical antibiotics for a differential diagnosis inclusive of organizing pneumonia, opportunistic infection, and radiation pneumonitis. The infectious workup was mostly inconclusive and nonspecific, with the patient remaining afebrile during his hospitalization while having a mild neutrophil-predominant leukocytosis (13.6 on arrival) attributed to steroid therapy. He had negative blood cultures, a negative nasopharyngeal direct respiratory panel, and a negative Legionella urine antigen test. Fungitell was elevated, but Platelia testing was negative for invasive aspergillosis, and his induced sputum culture only showed mixed respiratory flora. Vancomycin was suspended after his negative cultures and he was started on a course of Bactrim to cover for possible Pneumocystis jiroveci pneumonia in addition to completing 7 days of Zosyn. Owing to worsening respiratory failure, the patient was treated in the intensive care unit (ICU). Unfortunately, he failed to improve and died on the thirteenth day of his readmission, 2 months after the end of radiation treatment.
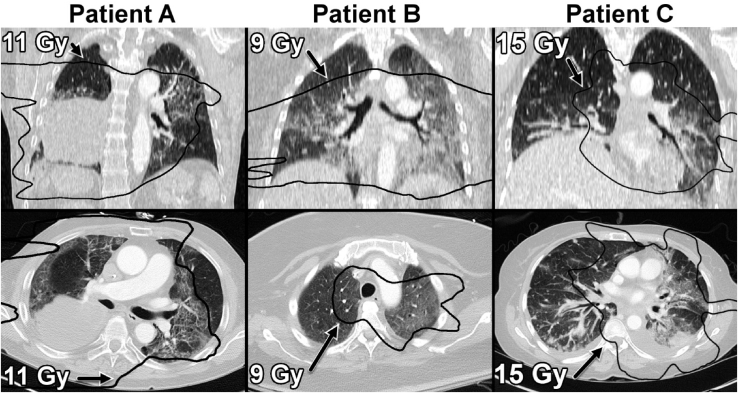
Figure 1.
Radiographic lung changes at the onset of pneumonitis symptoms. Computed tomographic images at the time of radiation pneumonitis diagnosis were deformably registered to the planning computed tomographies. Isodose lines approximating the interstitial lung changes were overlaid. For each patient, the isodose line that visually overlapped best with the observed lung changes is presented (patient A, 11 Gy; patient B, 9 Gy; patient C, 15 Gy). Shown are coronal (top) and axial (bottom) planes for each patient. In addition to the groundglass changes in patient A and B, patient C also had a pleural effusion and disease progression in both lungs with increasing lung metastases. Although low dose lines matched the lung changes well in patient A, the overlap area was less for patient B and particularly C indicating that dose levels vary between patients.
Patient B
A 72-year-old black woman was diagnosed with stage IIIA (T2N2M0) squamous cell carcinoma of the left lower lobe (LLL) with questionable involvement of a right hilar lymph node. Past medical history included diabetes mellitus type 2, hypertension, hyperlipidemia, osteoarthritis, obesity, and a cerebral meningioma that was resected 5 years earlier. She had a 30 pack-year smoking history and quit 9 years before her cancer diagnosis. Her KI was 80%, and pulmonary function tests showed a FEV1 of 130% predicted with DLCO of 68% predicted. Owing to presumed contralateral hilar involvement, the patient initially received weekly carboplatin and paclitaxel that was stopped prematurely after 3 cycles owing to severe peripheral neuropathy. Six months after chemotherapy she received a diagnosis of tumor progression in the LLL. She then underwent VMAT (60 Gy in 30 fractions, no concurrent systemic therapy) with daily CBCT for image guidance, which was tolerated well with only mild dysphagia. The volumes for iGTV, CTV, PTV, and lung-CTV were 85 mL, 191 mL, 363 mL, and 2741 mL, respectively. The lung DVH (lungs-CTV) showed a V5Gy of 92% (CL V5Gy 92%), V10Gy of 81%, and V20Gy of 32%. MLD was 20 Gy. MHD was 29.8 Gy and heart V60Gy 3%.
The patient presented approximately 2 months from the end of radiation treatment with diabetic ketoacidosis, seizure, and weakness. She was admitted for 8 days and was ultimately discharged to a skilled nursing facility on 3 L/min supplemental oxygen. Chest x-ray at 2 months posttreatment did not show significant changes except for tumor regression. She completed 7 days of antibiotics but was readmitted 4 days after hospital discharge with worsening hypoxia with SpO2 in the 60s, cough, and fever of 38.4°C. The patient was admitted to the ICU, and a new painful bone metastasis in the hip was diagnosed. Chest x-ray at admission showed worsening airspace disease. A chest CT 3 days later, or 2 months and 10 days from EOT, showed signs of new airspace disease with wide spread groundglass and reticular opacities with nodularity in the upper lobes and the LLL (Fig. 1). She was placed on intravenous methylprednisolone, bronchodilators (ipratropium and albuterol), and restarted broad-spectrum antibiotics, having a working diagnosis of acute on chronic hypoxic respiratory failure due to radiation pneumonitis and pneumonia. She had a negative direct respiratory pathogen panel, a negative Legionella urine antigen test, and negative blood cultures. She improved while completing a week of Vancomycin and Zosyn and was transferred out of the ICU, but decompensated shortly thereafter. Antibiotics were restarted with a new chest x-ray showing interval changes again concerning for a new or worsening pneumonia, but she remained afebrile and repeat blood cultures were negative. A new chest CT 1 week later revealed worsening ground glass and consolidative opacities in addition to her shrunken lung mass. The patient failed to significantly improve during hospitalization and died 1 month after readmission, or 15 weeks from EOT.
Patient C
A 52-year-old African woman received a diagnosis stage IV (T4N2M1) adenocarcinoma of the LLL with involvement of the pleura, pericardium, mediastinal, and subcarinal lymph nodes, and presumed small pulmonary metastases. She had no history of tobacco use and no significant past medical history with a KI of 100%. Tumor pathology was negative for epithelial growth factor receptor and anaplastic lymphoma kinase with 70% programmed death-ligand 1 positivity. She underwent initial immunotherapy with pembrolizumab for 4 cycles but had disease progression. She was subsequently switched to carboplatin and paclitaxel for 4 cycles and received maintenance pemetrexed. She then developed a lytic lesion in the T12 vertebra and underwent SBRT. Two months later, owing to primary tumor progression without evidence of progressive disease elsewhere and the patient's desire for aggressive treatment, IMRT (60 Gy in 30 fractions, no concurrent systemic therapy) to the LLL primary lesion and involved lymph nodes was performed using 6 fields with daily CBCT for image guidance. The volumes of iGTV, CTV, PTV, and lungs-CTV were 108 mL, 190 mL, 391 mL, and 2642 mL, respectively. Lung DVH (lungs-CTV) showed a V5Gy of 90% (CL V5Gy 88%), V10Gy of 67%, and V20Gy of 34%. MLD was 17.8 Gy. MHD was 18.8 Gy and heart V60Gy was 5%.
One month after lung IMRT the patient was found to have a single brain metastasis in her right temporal lobe for which she had a craniotomy and mass resection followed by WBRT to 30 Gy. She was then started on Taxotere chemotherapy. Nine weeks later, or 14 weeks after her lung IMRT, she was admitted with dry cough, pain in the lower chest, shortness of breath with SpO2 of 96%, tachycardia, and hypotension. She was neutropenic and developed fevers of 38.6°C. She also was found to have a pulmonary embolism associated with right lower extremity deep vein thrombosis and was started on anticoagulation, with antibiotics for suspected pneumonia. During her admission, her respiratory status worsened and she was transferred to the ICU. CT chest imaging showed diffuse ground glass opacities in the LLL and lingual and small bilateral pleural effusions. She was started on methylprednisolone for suspected RP and subsequently improved. A chest CT obtained 5 days after starting steroid treatment showed significant reduction of ground glass changes consistent with her clinical improvement. After briefly being discharged, she returned to the hospital 2 days later with increased difficulty breathing, cough, and a low fever. She had a chest tube placed for an enlarged left-sided pleural effusion and started broad-spectrum antibiotics. In addition to her effusions, imaging showed basilar consolidative airspace disease on the right and diffusely scattered ground glass opacities, as well as progression of pulmonary metastases. The patient failed to respond to intensive care treatment and ultimately died 5 months from the end of her lung radiation therapy. The ultimate cause of death in this patient was not identified with certainty. Although other conditions, such as status post pembrolizumab application, pneumonia, pleural effusion, disease progression, and pulmonary embolism, might have also played a role, RP was thought to be the likely major cause of the patient's symptoms.
Discussion and Literature Review
Symptomatic RP has been reported to occur in 17% to 30% of lung cancer patients treated with conventionally fractionated radiation therapy1, 27, 28 and 9% to 30% with SBRT.2, 29, 30 RP occurs also in patients undergoing radiation therapy to the chest for other diagnosis than lung cancer. For a more focused literature review, and because RP is most frequently observed in lung cancer patients, the present study was limited to lung cancer.
Although most patients having pneumonitis can be managed with established therapeutic interventions, including slowly tapered steroids, antibiotics, and respiratory support, G4 and G5 RP still occur in 1% to 4% of patients who undergo conventionally fractionated or hypofractionated radiation therapy.1, 20, 27, 28 Unexpectedly high rates of G5 RP were reported from several large centers after treating patients postoperatively with IMRT after extrapleural pneumonectomy for pleuramesothelioma.9, 10, 11, 12 Various dose factors ranging from V5Gy to V20Gy and MLD were found to be correlated with the increased risk. More recently, higher rates of G5 RP of up to 20% were reported in several series for patients with unresected locally advanced and early stage NSCLC.13, 14, 18, 19, 20, 22, 31 Observation of G5 RP in our own patients and review of recent reports prompted us to report particularly on fatal pneumonitis with the goal of identifying G5 RP-specific clinical and therapeutic risk factors. A large spectrum of factors has been associated with RP, including smoking status, smoking history, lung function, type and timing of systemic therapy, and patient performance among others.1, 2, 3 These factors will be discussed here only because they have been reported to affect G5 RP in lung cancer patients. Table 11,7,13,14,18,27,28,32, 33, 34, 35 (conventional fractionation) and Table 215,16,19,20,22,23,31,36,37,38 (SBRT) describe more recent studies that have reported on a minimum of 2 G5 RP patients with some description of G5 RP-related risk factors in lung cancer patients.
Table 1.
Conventionally fractionated radiation therapy for lung cancer
| Author | Grade 5 RP incidence | Average time to symptom onset for G5 RP | Survival from symptom onset | Treatment modality | Dosimetric factors lung Vx (%), MLD (Gy) | Statistical and other findings |
|---|---|---|---|---|---|---|
| Graham et al27 | 4/99 (4%) | 8/8 ≥G3 RP deceased 8 mo from EOT | 3D-CRT ± chemo | All G5 RP V20≥35% | V20 related to ≥G2 RP on MVA (P = .001) | |
| Jiang et al28 | 2/165 (1%) | 4.5 mo (3-6 mo) from start of RT | IMRT ± chemo | Study constraints MLD ≤22 Gy, V5 <65%, V20<40% (V20<35% with chemo) |
||
| Khalil et al13 | 2/12 (17%) in group I 2/50 (4%) in group III |
1.4-2.5 mo from start of RT | 3.3 mo from start of RT | IMRT | Group I V20<40% Group II V20<40% MLD ≤20 Gy Group III V5≤60%, V20<40% MLD ≤20 Gy |
No decrease in G3 or G4 RP in group III, but less G5 RP (P = .05) Heart V50 > in G5 RP (25.7% vs 14.7%) G5 RP in older patients with comorbidities |
| Lee et al18 | 5/60 (8%) | Median 33 d (6-160) from EOT for all RP patients 0-1.5 mo from EOT in all G5 RP |
Median 1.5 mo (1-3) from EOT | 3D-CRT ± chemo | G5 patients | ILD on pre-RT chest CT associated with RP (P = .009) MLD, V10, V20, V30, V40, and NTCP sig. associated with RP No difference between dosimetric factors of G5 RP vs <G5 RP |
| V20: 29.47-57.67 | ||||||
| V30: 24.82-42.56 | ||||||
| MLD: 15.22-26.73 | ||||||
| Nakamura et al32 | 5/102 (5%) | RT ± chemo | RP incidence less in superior lobe primary (P = .01) No difference in RP incidence ± chemo |
|||
| Palma et al1 | 16/836 (2%) | Concurrent 3D-CRT or IMRT + chemo | Lower lobe tumor, greater V20, and daily dose > 2 Gy predictive of G5 RP | |||
| Song et al14 | 4/37 | Median 11 days (0-24 d) from EOT | Helical tomotherapy ± chemo | G5 patients V20: 20%-29% MLD: 14-18 Gy |
Univariate analysis: Poor performance, V5, CL V5, and CL V10 significantly associated with G5 RP Multivariate analysis: CL V5 associated with G5 RP (P = .029); CL V5>80% had 20-fold risk increase of G5 (P = .018) |
|
| Tsujino et al33 | 2/71 (3%) | Concurrent 3D-CRT + chemo | G5 RP mean V20: 34.5 (± 3.5%) |
V20 significantly associated with ≥G2 RP ≥G2 RP at 6 mo 14% for V20≤25%, and 63% for V20≥26% |
||
| Wang et al34 | 27/463 (6%) | 53 d ± 26 d for out of field RP | All: 58 d (6-683) 13 pat with out-of-field RP: 33 d (6-68) |
RT ± chemo | Shorter survival for out-of-field RP (P < .001) and serum albumin < 35 g/dL (P = .042) | |
| Yamaguchi et al7 lung and esophageal cancer | 3/62 (5%) | Median 3.3 mo (1.8-4.8) from start of RT | 3D-CRT | G5 Pat (no data 3rd G5 Pat) V5: 36.5, 56.7 V10: 24.8, 43.9 V20: 5.3, 22.6 MLD: 5.2, 10.8 CL MLD: 5.2, 11.9 |
Subclinical ILD tended to be significant for G5 RP (P = .0785), extensive ILD in 2/3 G5 | |
| Zhuang et al35 | 3/24 (12.5%) | 1 pat during RT, 1 pat 2 d from EOT, 1 pat 21 d from EOT | Median 3 weeks (1, 3, 6 weeks) | IMRT + concurrent erlotinib | Normal V5-V30, MLD |
Abbreviations: 3DCRT = 3-dimensional conformal radiation therapy; CL = contralateral lung; CT = computed tomography; D = days; EOT = end of treatment; Gx = grade of radiation pneumonitis; ILD = interstitial lung disease; MLD = mean lung dose; IMRT = intensity modulated radiation therapy; mo = months; MVA = multivariate analysis; Pat = patient(s); NTCP = normal tissue complication probability; RP = radiation pneumonitis; RT = radiation therapy; sig. = significantly; Vx = lung volume receiving ≥x Gy radiation dose.
Table 2.
Stereotactic radiation therapy for lung cancer
| Author | Grade 5 RP incidence | Average time to symptom onset for G5 RP | Survival from symptom onset | Dosimetric factors Vx (%), MLD (Gy) |
Statistical and other findings |
|---|---|---|---|---|---|
| Aibe et al31 | 2/30 (13%) | 2.5 mo (2, 3) from EOT | 3 mo (2, 4) | G5 RP Pat (mean ≤G2 RP) V5: 43.6, 25.5 (20.5) V20: 13.9, 5.3 (4.8) MLD: 8.7, 4.8 (4.0) |
G5 RP vs ≤G2 RP GTV: P = .025 PTV: P = .096 V5: P = .067 |
| Bahig et al15 | 3/150 (2%) 3/5 (60%) with ILD |
Median 3.2 mo from EOT | G5 patients V5: 48, 33, 21 V20: 21, 15, 6 MLD: 11, 8, 5 |
||
| Bahig et al16 | 5/504 (1%) overall 5/24 (21%) with ILD |
2.1 mo (1.3-3.2) for ≥G3 RP | ≥G3 RP vs no RP V5 28% vs 18% (P = .05) MLD 7 vs 4 (P = .03) |
All G5 RP with ILD UVA: lower FEV1 (P = .04 on MVA), FVC, DLCO, V5, MLD, emphysema, O2 dependence, ILD associated with ≥G3 RP |
|
| Hof et al36 | 4/53 (8%) | ≥G3 RP significantly correlated with CL V5 (P = .001), TL V5 (P = .008), and CL MLD (P = .011) 4/7 ILD with G5 toxicity 2/4 G5 RP with ILD |
|||
| Onishi et al19 | 23/1789 (1%) | Median 75 d (14-204) | Median 53 d (4-802) | 14/19 G5 RP cases with ILD 3/4 of immediately progressive G5 RP cases without ILD |
|
| Onishi et al20 | 7% (N = 242 with ILD) | V20≥10% significant for G5 RP | |||
| Tekatli et al22 | 6/63 (10%) possible or likely | Median 9.5 mo (3.3-42.8) from start of RT | 4/8 patients with ILD developed G5 RP | ||
| Yamashita et al37 | 7/117 (6%) | Median 3 mo (1-6) from EOT | G5 RP mean | KL-6, SP-D, and interstitial pneumonitis (IP) on pre RT CT significantly correlated with ≥G4 RP No significant dose/volume differences for ≥ G4 RP vs <G4 RP |
|
| V20: 6.9 | |||||
| V40: 2.3 | |||||
| MLD: 5.6 | |||||
| Yamashita et al38 | 3/25 (12%) | 4.7 mo (3-6) from EOT | 1 mo after symptoms onset | Increased RP with higher conformity index No correlation between RP and MLD, field size, PTV, or V5-V50 |
|
| Yoshitake et al23 | 3/260 (1%) overall 3/18 (17%) with ILD 0/242 (0%) without ILD |
Median 4.3 mo (2.7-8.5) from EOT | ILD was only factor significantly associated with RP on MVA KL-6 > 600 U/mL and lung V5 >18% in RP G5 |
Abbreviations: CL = contralateral lung, CT = computed tomography, DLCO = diffusion capacity for carbon monoxide, EOT = end of treatment, FEV1 = forced expiratory volume in 1 second, FVC = forced vital capacity, Gx = grade of radiation pneumonitis, KL-6 = Krebs von den Lungen-6, ILD = interstitial lung disease, MLD = mean lung dose, MVA = multivariate analysis, RP = radiation pneumonitis, RT = radiation therapy, TL = total lung, SP-D = Surfactant protein D, UVA = univariate analysis, Vx = lung volume receiving ≥x Gy radiation dose.
Clinical symptoms, time to onset, and duration
Clinical symptoms of RP have not been described systematically in great detail. The predominant symptom at the time of clinical manifestation of RP is dyspnea with nonproductive cough. Fever has been reported to occur in about 30% of patients at the time of initial diagnosis of G5 RP.37, 39 Sekine et al39 reported on the clinical symptoms of pneumonitis in 385 lung cancer patients treated to 50 to 70 Gy. Patients with fatal pneumonitis (3.6%) showed higher rates of dyspnea and fever initially and during the clinical course of pneumonitis compared with patients with lower grade pneumonitis. Although there might be an initial response to steroid treatment, patients with G5 RP often do not respond to steroids at all or fail to have further therapeutic response at the time of symptom recurrence.34, 38 All of our patients developed dyspnea and 2 of them also had localized chest pain, perhaps related to pleuritic involvement at the time of onset of RP symptoms. Patient C had low-grade fevers and neutropenia; no evidence of infection was found. The actual cause of the fever remained unclear.
RP typically results in initial clinical symptoms after a latency period of 6 weeks to 6 months after the end of radiation therapy. Several authors reported early clinical manifestation of RP for patients with high-grade pneumonitis12, 32, 40 and patients with higher radiation dose to the lung.33 Literature review indicates that particularly patients with G5 RP treated for locally advanced disease experienced pneumonitis symptoms earlier than patients with lower grade pneumonitis.13, 18, 34 In some reports, patients started to develop RP symptoms during radiation therapy18 or within the first month after treatment.14, 35 Sekine et al39 reported that radiographic signs of RP appeared at a significantly shorter median interval after radiation therapy of only 2.4 weeks in patients with G5 RP compared with 9.9 weeks in patients not requiring steroids. Khalil et al13 who reported a 9% rate of G5 RP found a shorter time to onset of RP symptoms in G5 patients (1.4-2.5 months) compared with other ≥G3 RP (within first 6 months) after the start of radiation therapy. These authors also reported a significantly shorter survival for G5 RP patients compared with patients with G2 and G3 RP (median 3.3 months vs 16.3 months). After tomotherapy with or without chemotherapy, Song et al14 reported G5 RP in 4 of 37 patients (11%). Time to G5 RP was 11 days (range 0-24) from end of therapy compared with 32 days (range 0-215) for patients with lower grade RP. Lee et al18 reported G5 RP in 5 of 60 patients. Patients developed symptoms during treatment and up to 6 weeks post RT, and all died between 1 and 3 months. Zhuang et al35 reported on 3 of 24 patients treated with IMRT and erlotinib developing G5 RP during and up to 3 weeks after RT. Patients died one to 6 weeks after the onset of symptoms. Early symptom onset was also observed in our patients where the first signs of RP were seen between 1 and 3 months, and survival post radiation therapy was 2 to 5 months.
The time course of G5 RP in SBRT seems to be more delayed, with onset reported after a median of 75 days (range, 14-204 days) from the start of radiation therapy and a median survival of 53 days (4-802) in a large series of 1789 patients with 1% G5 RP.24 Tekatli et al22 reported G5 RP in 6 of 63 patients treated with SBRT for >5 cm tumors. Patients survived 4.8 to 42.8 months from treatment start.
Imaging findings
Typical radiographic changes after radiation therapy display diffuse or patchy ground glass opacities or consolidation. Although radiographic changes of pneumonitis are often confined to the treatment fields, cases of G5 RP after tomotherapy, IMRT, SBRT, and 3-dimensional conformal radiation therapy (3DCRT) typically display more diffuse interstitial and infiltrative changes that cover large areas of both lungs.7, 9, 14, 31, 41 Patients with lung changes extending beyond the radiation fields seem to have a worse prognosis. Wang et al34 reported on 31 patients with ≥G3 RP. Thirteen patients developed out-of-field pneumonitis, had a latent period of 53 ± 26 days and died after median 33 days without response to steroids, except for transient improvement in 2 patients. Comparably, 18 patients developed in-field pneumonitis, exhibiting a latent period of 70 ± 32 days with median survival of 160 days. Similar to the associated clinical symptoms, radiographic changes associated with RP appear sooner in patients with G5 RP than in lower grade pneumonitis. Sekine et al39 reported a median duration from the end of radiation therapy to the onset of radiographic change of 9.9 weeks (–2.9 to 45.1) for patients who did not need steroids, compared with 6.7 weeks (0-24.5) for patients with higher grade pneumonitis, and 2.4 weeks (0.4-10.1) for G5 RP. In this report, 79% of patients with G5 RP developed the first radiographic changes before 6 weeks and none after 12 weeks compared with 27% and 35% in patients not requiring steroids and 41% and 14% in patients requiring steroids, but without fatal outcome. Typically in G5 RP, once initial radiographic signs become manifest, radiographic changes quickly spread to involve large areas of the lung. Three out of 5 patients with G5 RP reported by Lee et al18 developed focal consolidation in the radiation fields during treatment or within 1 month after EOT that progressed to involve the whole lung; the other 2 patients presented with bilateral lung infiltration 4 to 6 weeks after RT with rapid progression. The extent of radiographic changes in our described patients is shown in Figure 1. Symptoms preceded radiographic changes by days and weeks; only when symptoms became severe did airspace disease become visible on imaging. As demonstrated in Figure 1, in 2 of our patients the low dose lung volumes were found to overlap with the observed extent of the lung changes. With ongoing consolidation resulting in lung deformation in patient C, no clear overlap pattern between dose and lung changes could be identified.
Radiation dose factors and treatment technique
Radiation dose to the lung has frequently been investigated as a predictor of RP. Mean lung dose, relative percentages of the whole lung volume receiving defined doses, particularly V20Gy, and normal tissue complication probability values have classically been associated with the RP risk.3 They have been used in routine clinical treatment, ongoing clinical trial protocols, and treatment guidelines. The identified threshold doses depend on a large variety of factors such as the use of heterogeneity correction, the method used to calculate lung volumes, for example, whole lung minus GTV, CTV or PTV, and whether chemotherapy is delivered together with radiation therapy among others.3 In a metaanalysis by Palma et al,1 including 836 patients treated with 3DCRT or IMRT, G5 RP was observed in 16 cases (1.9%). V20Gy was associated with an increased risk of G5 RP (odds ratio 1.09 for every 1% increase). In addition, ≥2 Gy dose per fraction was also identified with a higher G5RP risk. The risk for G5 RP was 7% for a fraction size >2 Gy versus 1.5% for ≤2 Gy. Graham et al27 reported G5 RP in 4 of 99 patients after 3DCRT, with all 4 patients having a V20Gy ≥35%. Similarly, Tsujino et al,33 who reported 2 cases of G5 RP after 3DCRT found that the patients with G5 RP had a mean V20Gy of 34.5% ± 3.5%. In the report by Lee et al,18 patients with G5 RP did not have higher lung doses than patients with lower grade RP; however, doses were rather high overall with MLD between 15.2 Gy and 26.7 Gy, V20Gy of 29.5% to 57.7%, and V30Gy of 24.8% to 42.6%.
More recently, with the increasing use of tomotherapy, IMRT, and VMAT, treatments resulting in larger low-dose lung volumes, lung V5Gy and V10Gy, and low dose contralateral lung volumes have been identified as factors contributing to the RP risk.7, 13, 14 For tomotherapy some authors recommend to specifically include low V5Gy and V10 Gy limits for the total and contralateral lung. For example, Song et al14 using tomotherapy recommended a contralateral lung V5Gy < 60% in addition to conventional dose parameters. In their report, a contralateral lung V5Gy > 80% was associated with a 20-fold increase of treatment-related death. One of the most remarkable reports by Khalil et al13 showed an increase of G5 RP after the introduction of IMRT and a reduction of the G5 RP risk when using a low dose constraint, V5Gy ≤ 60%. Two of our patients received VMAT and one received fixed-field IMRT, resulting in large V5Gy volumes of the total and contralateral lung while meeting conventional dose thresholds. In our patients, no V5Gy constraints were used for plan optimization.
For SBRT, several authors reported an increased high-grade pneumonitis risk with higher lung dose, whereas others did not find a lung dose-RP correlation. Higher V5Gy, V10Gy, V20Gy, and MLD have been associated with high-grade pneumonitis risk after SBRT by several authors.2, 7, 15, 16, 23, 29 Using VMAT, Hof et al36 identified total lung V5Gy, contralateral lung V5Gy, and contralateral MLD as factors associated with high-grade RP in ≥5 cm tumors. Onishi et al20 reported that G5 RP was significantly higher for V20Gy ≥ 10%.
In addition to treatment technique, dose distributions are affected by tumor size and field length. It is not surprising that larger tumors and tumors in the lower lobes that often include mediastinal lymph nodes have been associated with a higher RP risk.1, 2, 31, 32 With long superior-inferior volumes, large parts of the lungs are traversed by the radiation beams. Total lung volumes, lung volumes spared from radiation or PTV or lung volume ratios might therefore play a role for predicting RP risk. Lung-CTV volumes are typically used to create mean lung dose and relative VxGy volumes. Absolute lung or lung-CTV volumes are not commonly used to assess the risk for pulmonary toxicity. Lung-CTV volumes and PTV or lung volume ratios were reported in RTOG 0617.42 When comparing our data with RTOG 0617 data, our patients had on average lower lung-CTV volumes potentially indicating a higher RP risk. However, in RTOG 0617 IMRT patients had less pneumonitis than 3DCRT patients despite statistically larger PTV volumes, lower lung-CTV volumes, and larger PTV or lung volume ratios. The importance of lung-CTV volumes is therefore not clear and needs to be investigated further. Radiation therapy for locally advanced tumors in the lower lobes can also result in a higher heart dose, which was found to be associated with G5 RP,13 whereas tumor location does not appear to affect heart dose for SBRT treatments of early stage disease.43
With the increasing use of image guidance, imaging dose needs to be considered as well. All of our patients underwent daily CBCT imaging. Assuming a daily CBCT imaging dose of 3 cGy, an additional dose of about 1 Gy to a large lung volume needs to be added to the dose delivered through the therapy beams. This equates to about 20% of the 5 Gy dose volume that has been found to be relevant for RP in several studies. For assessment of the correct dose-RP relationship, verification imaging doses should therefore be considered.
Interstitial lung disease
Interstitial lung disease (ILD), also called interstitial pneumonia, interstitial pneumonitis, or usual interstitial pneumonia, has been identified by several recent reports as a significant risk factor for high-grade and G5 RP after SBRT.15, 16, 19, 20, 22, 23, 36, 37, 44 G5 RP was reported in 7% to 21% of patients with ILD.16, 19, 20 Yoshitake et al23 found a 17% incidence of G5 RP in patients with ILD compared with 0% in patients without ILD. In a recent review by Chen et al,17 the increased risk for toxicity in patients with ILD was confirmed and dose recommendations were given to avoid mortality in this population. The authors suggested the constraints of V20Gy ≤6.5% and MLD ≤4.5 Gy. ILD was also identified as a significant risk factor for G5 RP in several studies reporting outcomes after conventionally fractionated radiation therapy.7, 8, 18, 41 None of our patients showed pretreatment ILD.
Conclusions
Patients with G5 RP develop pneumonitis symptoms earlier than patients with lower grade pneumonitis and have severe symptoms that often do not respond to steroid treatment. Imaging shows associated changes in large lung volumes including the contralateral lung and areas outside of the high-dose radiation fields. Both low and higher dose lung volumes seem to be relevant for plan optimization with advanced treatment techniques for early stage and locally advanced lung cancers. From our own observation and literature review, low dose constraints, such as V5Gy ≤ 60%, should therefore be included in treatment protocols and therapeutic guidelines for locally advanced lung cancer, in addition to established lung dose constraints such as V20Gy and mean lung dose, particularly when using IMRT and even more so for VMAT. In RTOG 0617, lung V5Gy was significantly higher in the IMRT arm, but lung V5Gy was not associated with ≥ G3 RP in this study. The reason for this might be that more than half of the patients received 3D CRT with a median V5Gy of 54.8% and an interquartile range of 43.3 to 65.9%, compared with 61.6% and an interquartile range of 52.1% to 70.4% for IMRT. In addition, V5Gy doses delivered in RTOG 0617 were likely lower than described in the present study where VMAT was used in 2 of our patients and a highly modulated IMRT plan in patient C.42
Despite decades of investigating pneumonitis, the question of the optimum dose distribution in the lung, a large dose to a small volume versus a small dose to a large volume, is still unresolved. When both low and high dose lung volume constraints are followed, the risk for G5 RP has been shown to be low even with IMRT and concurrent chemotherapy.28 In addition to dose factors, underlying clinical and radiographic parameters play an important role for the G5 RP risk as demonstrated with the presence of ILD, particularly for patients treated with SBRT. Radiomics of the lung may therefore improve upon the predictive strength of traditional clinical and DVH parameters and should be investigated further.45
Footnotes
Sources of support: This work had no specific funding.
Disclosures: None
References
- 1.Palma D.A., Senan S., Tsujino K. Predicting radiation pneumonitis after chemoradiation therapy for lung cancer: An international individual patient data meta-analysis. Int J Radiat Oncol Biol Phys. 2013;85:444–450. doi: 10.1016/j.ijrobp.2012.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao J., Yorke E.D., Li L. Simple factors associated with radiation-induced lung toxicity after stereotactic body radiation therapy of the thorax: A pooled analysis of 88 studies. Int J Radiat Oncol Biol Phys. 2016;95:1357–1366. doi: 10.1016/j.ijrobp.2016.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marks L.B., Bentzen S.M., Deasy J.O. Radiation dose-volume effects in the lung. Int J Radiat Oncol Biol Phys. 2010;76:S70–S76. doi: 10.1016/j.ijrobp.2009.06.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis G.D., Agrusa J.E., Teh B.S. Radiation pneumonitis in pediatric Hodgkin lymphoma patients receiving radiation therapy to the chest. Pract Radiat Oncol. 2018;8:e364–e368. doi: 10.1016/j.prro.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 5.Pinnix C.C., Huo J., Milgrom S.A. Using benchmarked lung radiation dose constraints to predict pneumonitis risk: Developing a nomogram for patients with mediastinal lymphoma. Adv Radiat Oncol. 2018;3:372–381. doi: 10.1016/j.adro.2018.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whelan T.J., Olivotto I.A., Parulekar W.R. Regional nodal irradiation in early-stage breast cancer. N Engl J Med. 2015;373:307–316. doi: 10.1056/NEJMoa1415340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamaguchi S., Ohguri T., Matsuki Y. Radiotherapy for thoracic tumors: Association between subclinical interstitial lung disease and fatal radiation pneumonitis. Int J Clin Oncol. 2015;20:45–52. doi: 10.1007/s10147-014-0679-1. [DOI] [PubMed] [Google Scholar]
- 8.Niska J.R., Schild S.E., Rule W.G., Daniels T.B., Jett J.R. Fatal radiation pneumonitis in patients with subclinical interstitial lung disease. Clin Lung Cancer. 2018;19:e417–e420. doi: 10.1016/j.cllc.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 9.Allen A.M., Czerminska M., Jänne P.A. Fatal pneumonitis associated with intensity-modulated radiation therapy for mesothelioma. Int J Radiat Oncol Biol Phys. 2006;65:640–645. doi: 10.1016/j.ijrobp.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 10.Kristensen C.A., Nottrup T.J., Berthelsen A.K. Pulmonary toxicity following IMRT after extrapleural pneumonectomy for malignant pleural mesothelioma. Radiother Oncol. 2009;92:96–99. doi: 10.1016/j.radonc.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 11.Miles E.F., Larrier N.A., Kelsey C.R. Intensity-modulated radiotherapy for resected mesothelioma. The Duke experience. Int J Radiat Oncol Biol Phys. 2008;71:1143–1150. doi: 10.1016/j.ijrobp.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Rice D.C., Smythe W.R., Liao Z. Dose dependent pulmonary toxicity after postoperative intensity-modulated radiotherapy for malignant pleural mesothelioma. Int J Radiat Oncol Biol Phys. 2007;69:350–357. doi: 10.1016/j.ijrobp.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 13.Khalil A.A., Hoffmann L., Moeller D.S., Farr K.P., Knap M.M. New dose constraint reduces radiation-induced fatal pneumonitis in locally advanced non-small cell lung cancer patients treated with intensity-modulated radiotherapy. Acta Oncol. 2015;54:1343–1349. doi: 10.3109/0284186X.2015.1061216. [DOI] [PubMed] [Google Scholar]
- 14.Song C.H., Pyo H., Moon S.H., Kim T.H., Kim D.W., Cho K.H. Treatment-related pneumonitis and acute esophagitis in non-small-cell lung cancer patients treated with chemotherapy and helical tomotherapy. Int J Radiat Oncol Biol Phys. 2010;78:651–658. doi: 10.1016/j.ijrobp.2009.08.068. [DOI] [PubMed] [Google Scholar]
- 15.Bahig H., Filion E., Vu T. Excellent cancer outcomes following patient-adapted robotic lung SBRT but a case for caution in idiopathic pulmonary fibrosis. Technol Cancer Res Treat. 2015;14:667–676. doi: 10.7785/tcrt.2012.500445. [DOI] [PubMed] [Google Scholar]
- 16.Bahig H., Filion E., Vu T. Severe radiation pneumonitis after lung stereotactic ablative radiation therapy in patients with interstitial lung disease. Pract Radiat Oncol. 2016;6:367–374. doi: 10.1016/j.prro.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Chen H., Senan S., Nossent E.J. Treatment-related toxicity in patients with early-stage non-small cell lung cancer and coexisting interstitial lung disease: A systematic review. Int J Radiat Oncol Biol Phys. 2017;98:622–631. doi: 10.1016/j.ijrobp.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Lee Y.H., Kim Y.S., Lee S.N. Interstitial lung change in pre-radiation therapy computed tomography is a risk factor for severe radiation pneumonitis. Cancer Res Treat. 2015;47:676–686. doi: 10.4143/crt.2014.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Onishi H., Marino K., Yamashita H. Case series of 23 patients who developed fatal radiation pneumonitis after stereotactic body radiotherapy for lung cancer. Technol Cancer Res Treat. 2018;17:1–6. doi: 10.1177/1533033818801323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Onishi H., Yamashita H., Shioyama Y. Stereotactic body radiation therapy for patients with pulmonary interstitial change: High incidence of fatal radiation pneumonitis in a retrospective multi-institutional study. Cancers (Basel) 2018;10:257. doi: 10.3390/cancers10080257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Osborn V.W., Leaf A., Lee A. Bilateral diffuse grade 5 radiation pneumonitis after intensity modulated radiation therapy for localized lung cancer. World J Clin Oncol. 2017;8:285–288. doi: 10.5306/wjco.v8.i3.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tekatli H., Van 't hof S., Nossent E.J. Use of stereotactic ablative radiotherapy (SABR) in non-small cell lung cancer measuring more than 5 cm. J Thorac Oncol. 2017;12:974–982. doi: 10.1016/j.jtho.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 23.Yoshitake T., Shioyama Y., Asai K. Impact of interstitial changes on radiation pneumonitis after stereotactic body radiation therapy for lung cancer. Anticancer Res. 2015;35:4909–4913. [PubMed] [Google Scholar]
- 24.Hsieh C.H., Chang H.T., Lin S.C. Toxic risk of stereotactic body radiotherapy and concurrent helical tomotherapy followed by erlotinib for non-small-cell lung cancer treatment—case report. BMC Cancer. 2010;10:696. doi: 10.1186/1471-2407-10-696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu Y., Li J., Su X. Fatal pneumonitis associated with postoperative intensity-modulated radiotherapy in lung cancer: Case report and review. Oncol Lett. 2013;5:714–716. doi: 10.3892/ol.2012.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Westhoff P.G., De Ruysscher D.K., Schramel F.M. Fatal bilateral pneumonitis after locoregional thoracic chemoradiation in a transplanted patient under immunosuppressive therapy. Anticancer Res. 2014;34:7315–7317. [PubMed] [Google Scholar]
- 27.Graham M.V., Purdy J.A., Emami B. Clinical dose-volume histogram analysis for pneumonitis after 3D treatment for non-small cell lung cancer (NSCLC) Int J Radiat Oncol Biol Phys. 1999;45:323–329. doi: 10.1016/s0360-3016(99)00183-2. [DOI] [PubMed] [Google Scholar]
- 28.Jiang Z.Q., Yang K., Komaki R. Long-term clinical outcome of intensity-modulated radiotherapy for inoperable non-small cell lung cancer: The MD Anderson experience. Int J Radiat Oncol Biol Phys. 2012;83:332–339. doi: 10.1016/j.ijrobp.2011.06.1963. [DOI] [PubMed] [Google Scholar]
- 29.Harder E.M., Park H.S., Chen Z., Decker R.H. Pulmonary dose-volume predictors of radiation pneumonitis following stereotactic body radiation therapy. Pract Radiat Oncol. 2016;6:e353–e359. doi: 10.1016/j.prro.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 30.Yamashita H., Takahashi W., Haga A., Nakagawa K. Radiation pneumonitis after stereotactic radiation therapy for lung cancer. World J Radiol. 2014;6:708–715. doi: 10.4329/wjr.v6.i9.708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aibe N., Yamazaki H., Nakamura S. Outcome and toxicity of stereotactic body radiotherapy with helical tomotherapy for inoperable lung tumor: Analysis of Grade 5 radiation pneumonitis. J Radiat Res. 2014;55:575–582. doi: 10.1093/jrr/rrt146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nakamura T., Fuwa N., Kodaira T. Clinical outcome of stage III non-small-cell lung cancer patients after definitive radiotherapy. Lung. 2008;186:91–96. doi: 10.1007/s00408-007-9063-5. [DOI] [PubMed] [Google Scholar]
- 33.Tsujino K., Hirota S., Endo M. Predictive value of dose-volume histogram parameters for predicting radiation pneumonitis after concurrent chemoradiation for lung cancer. Int J Radiat Oncol Biol Phys. 2003;55:110–115. doi: 10.1016/s0360-3016(02)03807-5. [DOI] [PubMed] [Google Scholar]
- 34.Wang J.Y., Chen K.Y., Wang J.T. Outcome and prognostic factors for patients with non-small-cell lung cancer and severe radiation pneumonitis. Int J Radiat Oncol Biol Phys. 2002;54:735–741. doi: 10.1016/s0360-3016(02)02994-2. [DOI] [PubMed] [Google Scholar]
- 35.Zhuang H., Yuan Z., Chang J.Y. Radiation pneumonitis in patients with non-small-cell lung cancer treated with erlotinib concurrent with thoracic radiotherapy. J Thorac Oncol. 2014;9:882–885. doi: 10.1097/JTO.0000000000000126. [DOI] [PubMed] [Google Scholar]
- 36.Hof S.V., Delaney A.R., Tekatli H. Knowledge-based planning for identifying high-risk stereotactic ablative radiation therapy treatment plans for lung tumors larger than 5 cm. Int J Radiat Oncol Biol Phys. 2019;103:259–267. doi: 10.1016/j.ijrobp.2018.08.013. [DOI] [PubMed] [Google Scholar]
- 37.Yamashita H., Kobayashi-Shibata S., Terahara A. Prescreening based on the presence of CT-scan abnormalities and biomarkers (KL-6 and SP-D) may reduce severe radiation pneumonitis after stereotactic radiotherapy. Radiat Oncol. 2010;5:32. doi: 10.1186/1748-717X-5-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yamashita H., Nakagawa K., Nakamura N. Exceptionally high incidence of symptomatic grade 2-5 radiation pneumonitis after stereotactic radiation therapy for lung tumors. Radiat Oncol. 2007;2:21. doi: 10.1186/1748-717X-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sekine I., Sumi M., Ito Y. Retrospective analysis of steroid therapy for radiation-induced lung injury in lung cancer patients. Radiother Oncol. 2006;80:93–97. doi: 10.1016/j.radonc.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 40.Appelt A.L., Vogelius I.R., Farr K.P., Khalil A.A., Bentzen S.M. Towards individualized dose constraints: Adjusting the QUANTEC radiation pneumonitis model for clinical risk factors. Acta Oncol. 2014;53:605–612. doi: 10.3109/0284186X.2013.820341. [DOI] [PubMed] [Google Scholar]
- 41.Yamaguchi S., Ohguri T., Ide S. Stereotactic body radiotherapy for lung tumors in patients with subclinical interstitial lung disease: The potential risk of extensive radiation pneumonitis. Lung Cancer. 2013;82:260–265. doi: 10.1016/j.lungcan.2013.08.024. [DOI] [PubMed] [Google Scholar]
- 42.Chun S.G., Hu C., Choy H. Impact of intensity-modulated radiation therapy technique for locally advanced non–small-cell lung cancer: A secondary analysis of the NRG Oncology RTOG 0617 randomized clinical trial. J Clin Oncol. 2017;35:56–62. doi: 10.1200/JCO.2016.69.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reshko L.B., Kalman N.S., Hugo G.D., Weiss E. Cardiac radiation dose distribution, cardiac events and mortality in early stage lung cancer treated with stereotactic radiation therapy (SBRT) J Thorac Dis. 2018;10:2346–2356. doi: 10.21037/jtd.2018.04.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ueki N., Matsuo Y., Togashi Y. Impact of pretreatment interstitial lung disease on radiation pneumonitis and survival after stereotactic body radiation therapy for lung cancer. J Thorac Oncol. 2015;10:116–125. doi: 10.1097/JTO.0000000000000359. [DOI] [PubMed] [Google Scholar]
- 45.Krafft S.P., Rao A., Stingo F. The utility of quantitative CT radiomics features for improved prediction of radiation pneumonitis. Med Phys. 2018;45:5317–5324. doi: 10.1002/mp.13150. [DOI] [PubMed] [Google Scholar]