This cross-sectional study assesses the quantity and quality of sleep and the factors associated with sleep disturbances in hospitalized patients in the Netherlands.
Key Points
Questions
What is the quantity and quality of sleep in hospitalized patients compared with their habitual sleep at home and what are the main factors that disturb sleep during hospitalization?
Findings
This cross-sectional study of 2005 patients in the Netherlands found that sleep duration and sleep quality were significantly affected in hospitalized patients compared with patients’ habitual sleep at home. Many potentially modifiable hospital- and patient-related factors were associated with sleep disturbances in the hospital.
Meaning
Quality and quantity of sleep in hospitalized patients may be suboptimal and negatively associated with many hospital-related factors; interventions to target sleep-disturbing factors in hospitals may improve healing.
Abstract
Importance
Although inadequate sleep has a proven negative association with health care outcomes, to date, no large-scale studies have examined sleep in general hospital wards.
Objectives
To assess the subjective quantity and quality of sleep and to identify the hospital-related factors associated with sleep disturbances in hospitalized patients.
Design
For this nationwide, single-day, multicenter, cross-sectional, observational study, which took place on February 22, 2017, all hospitals in the Netherlands were encouraged by word of mouth and conventional and social media to participate in this study. A total of 39 hospitals participated. Included patients were at least 18 years of age, were able to give informed consent, and had spent at least 1 night in a regular-care hospital ward.
Exposures
Hospitalization in a regular-care ward.
Main Outcomes and Measures
Quantity and quality of last night's sleep in the hospital compared with habitual sleep at home the month before hospitalization. The Consensus Sleep Diary and the Dutch-Flemish Patient-Reported Outcomes Measurement Information System (PROMIS) Sleep Disturbance item bank were used. Complementary questions assessed sleep-disturbing factors.
Results
A total of 2005 patients were included (median age, 68 years; interquartile range, 57-77 years; 994 of 1935 [51.4%] were male [70 patients did not identify their sex]). Compared with habitual sleep at home, the total sleep time in the hospital was 83 minutes (95% CI, 75-92 minutes; P < .001) shorter. The mean number of nocturnal awakenings was 2.0 (95% CI, 1.9-2.1) times at home vs 3.3 (95% CI, 3.2-3.5) times during hospitalization (P < .001). Patients woke up 44 minutes (95% CI, 44-45 minutes; P < .001) earlier than their habitual wake-up time at home. A total of 1344 patients (70.4%) reported having been awakened by external causes, which in 718 (35.8%) concerned hospital staff. All aspects of sleep quality measured using PROMIS questions were rated worse during hospitalization than at home. The most reported sleep-disturbing factors were noise of other patients, medical devices, pain, and toilet visits.
Conclusions and Relevance
This study demonstrated that the duration and quality of sleep in hospitalized patients were significantly affected and revealed many potentially modifiable hospital-related factors negatively associated with sleep. Raising awareness about the importance of adequate sleep in the vulnerable hospital population and introducing interventions to target sleep-disturbing factors may improve healing.
Introduction
Inadequate sleep has a negative association with general health and well-being.1,2,3,4 Small studies5,6,7,8,9 in selected patient populations suggest that sleep in hospitals is suboptimal. However, information about the quantity and quality of sleep in patients in general hospital wards is lacking. A good night's sleep improves cognitive and emotional functioning,10 which is important during an often emotionally challenging stay in the hospital. Sleep is essential for adequate immune, metabolic, and endocrine functioning1,11,12,13 and may have an association with healing and survival.14 Studies15,16 suggest that sleep deprivation is a possible key risk factor for development of delirium.
Patient-related factors, such as pain, and hospital-related factors, such as noises from alarms or sleep interruptions attributable to medical procedures, may contribute to disturbance of sleep.17,18,19,20 However, to date, no large-scale, multicenter studies have been performed to investigate how these factors are associated with sleep disturbance in hospitals. Identifying relevant and potentially modifiable hospital-related factors associated with sleep disturbances can be the key to introducing remedial measures. The primary aims of this nationwide, single-day study in the Netherlands were to assess the quantity and quality of sleep and to identify the hospital-related factors associated with sleep disturbances in hospitalized patients.
Methods
Study Design and Participants
This was a nationwide, single-day, multicenter, cross-sectional, observational study using the flash mob research (FMR) method, which allows the investigation of clinically relevant questions on a large scale in a short time.21 Flash mob research is based on the concept of flash mobs: “a sudden and planned gathering of many people at a particular place that has been arranged earlier.”22 With the use of multiple hospitals, it is possible to obtain sufficient data with FMR in a short time. After preparing the study, the coordinators (H.M.W., E.S.v.d.E., J.A., F.H.B., E.J.W.v.S., and P.W.B.N.) invited acute care internists from hospitals throughout the Netherlands to participate in the study using word of mouth and conventional and social media. Hospitals were also recruited through the professional network of the members of the “Onderzoeks Consortium Acute Geneeskunde” Acute Medicine Research Consortium.23 All participating hospitals received approval from their local ethics committees to obtain verbal informed consent with annotation in the patient record. Patient records were anonymized before the coordinators received them.
The coordinating center, the VU University Medical Center in Amsterdam, the Netherlands, provided a standardized protocol, instructions on procedures, case report forms, and questionnaires. The study was performed on February 22, 2017, between 8 am and 5 pm. To stimulate participation by health care workers and patients, conventional and social media provided some information before the study. However, to minimize observer and participant bias, release of the exact study date was embargoed until 6 am February 22, 2017.
All patients at least 18 years of age, with any disease condition, able to give informed consent, and who spent at least the night before the data collection in a regular-care ward were eligible for enrollment. Patients from intensive care, coronary care, and stroke units were excluded.
Questionnaire
A Consensus Sleep Diary (CSD) was used to asses subjective sleep quantity.24 In addition, after reaching consensus among the coordinating members, we selected 5 of 8 items from the Dutch-Flemish Patient-Reported Outcomes Measurement Information System (PROMIS), version 1.0, sleep disturbance item bank (Short Form 8a) and a sixth item from the complete PROMIS sleep disturbance item bank, which we believed were best suitable to measure sleep disturbance in hospitalized patients.25,26 To measure the differences in sleep experiences in the hospital vs home, each item was asked twice: once with reference to the previous night at the hospital and once with reference to habitual sleep at home during the month before hospitalization. These items were complemented by questions about hospital-related, personal, and environmental factors that could have influenced sleep, including use of sleep medication (eAppendix in the Supplement).
Sleep Quantity
The CSD items assessed subjective estimates of the clock times of lights out (ie, closing the eyes to fall asleep) and final awakening, sleep-onset latency (ie, time taken to fall asleep), the number of awakenings, and the total duration of wake after sleep onset (ie, time spent awake after going to sleep). The information provided was used to calculate total sleep time (ie, actual time spent asleep) and sleep efficiency (ie, the proportion of sleep relative to the time between lights out and final awakening).
Sleep Disturbance
The included 5-point Likert-type PROMIS items assessed 2 positive (satisfying and refreshing) and 3 negative (restless, difficulty falling asleep, and feeling lousy when waking up) evaluations of sleep. Each item provided a statement and asked how well it suited the patient, from not at all to very much. A sixth item on general sleep quality was answered as very poor to very good. The items that assessed positive evaluations were recoded in such a way that a higher score indicated more sleep disturbance. Because the time frame was adjusted for the design of this study, we did not calculate PROMIS T scores but only used raw summary scores (range, 0-24) that described overall sleep disturbance.
Disturbing Factors
The CSD items were complemented by questions on whether sleep was associated with a list of disease-related, hospital-related, personal, or environmental sleep-disturbing factors. An additional text field allowed patients to fill out other factors.
Statistical Analysis
Intrinsic to the FMR approach, no fixed sample size was set a priori. However, to obtain reliable and generalizable results and based on what was found feasible in a previous study,21 we aimed to include at least 1000 patients.
Categorical variables are summarized by percentages. Continuous variables are summarized by means and 95% CIs or medians and interquartile ranges (IQRs). Mean sleep quality and quantity were compared between hospital and home using mixed linear models with the patients’ difference scores (hospital relative to home) as the dependent variable, with an intercept-only model for the fixed part and a random effect of hospital. Means were concluded to differ between hospital and home when the fixed intercept differed significantly from 0. To check whether differences in mean sleep quality and quantity between hospital and home varied across groups of patients, we added a fixed effect for the grouping variable to the mixed model. Transformations of the dependent variables were considered in case residuals and were not normally distributed. To assess the robustness of the conclusions based on mixed-model analysis to deviations from normality, additional sensitivity analyses were performed in which we compared the individual differences between groups using nonparametric tests (Mann-Whitney test and Kruskal-Wallis analysis of variance). The nonparametric tests ignored the clustering of patients within hospitals, but this clustering was found to be ignorable because the variance component for the random effect of hospital in the mixed models was often estimated to be 0. Normality of dependent variables and residuals from the mixed models was checked using normal probability plots. Analyses were performed with SPSS for Windows, version 21 (SPSS Inc). P < .05 was considered to be statistically significant.
Results
An estimated potential population of approximately 2500 patients was eligible for inclusion; however, some patients could not be included because they were too sick or could not grant consent because of cognitive disturbances (on clinical grounds). The questionnaire was completed by 2005 patients in 39 of 93 Dutch hospitals (median age, 68 years; IQR, 57-77 years; 994 of 1935 [51.4%] were male [70 patients did not identify their sex]). Nonsurgical specialties were best represented (1536 [81.0%]) (Table 1). A total of 335 patients (16.7%) had been taking sleep medication at home (of which 189 [56.4%] were taking benzodiazepines) and 539 (26.9%) the previous night (of which 264 [49.0%] were taking benzodiazepines) (eTable 1 in the Supplement).
Table 1. Characteristics of 2005 Patients.
| Characteristic | Findinga |
|---|---|
| Sex (n = 1935) | |
| Male | 994 (51.4) |
| Female | 941 (48.6) |
| Age, y (n = 1975) | |
| Median (IQR) | 68 (57-77) |
| ≤35 | 117 (5.9) |
| 36-50 | 216 (10.9) |
| 51-65 | 525 (26.6) |
| 66-80 | 765 (38.7) |
| ≥81 | 352 (17.8) |
| Length of stay (n = 1773) | |
| Median (IQR) | 4 (2-8) |
| 1 Night | 359 (20.2) |
| >1 Nights | 1414 (79.8) |
| No. of patients in room (n = 1975) | |
| Median (IQR) | 2 (1-4) |
| 1 | 504 (25.5) |
| 2 | 514 (26.0) |
| 3 | 163 (8.3) |
| 4 | 774 (39.2) |
| ≥5 | 35 (1.8) |
| Ward type (n = 1945) | |
| Acute admission unit | 269 (13.8) |
| Regular ward | 1676 (86.2) |
| Specialty (n = 1897) | |
| Surgical specialtiesb | 361 (19.0) |
| Nonsurgical specialtiesc | 1536 (81.0) |
| Surgery (n = 1981) | |
| Yes | 451 (22.8) |
| No | 1530 (77.2) |
Abbreviation: IQR, interquartile range.
Data are presented as number (percentage) of patients unless otherwise indicated. All 2005 patients answered the questions concerning demographics and sleep-disturbing factors. In 30 cases, the necessary demographic information could not be extracted mainly because we could not read the handwriting (n = 1975). Because some patients did not fill in 1 or 2 questions, we decided not to exclude them for every question but only for the ones they did not respond to.
Surgical specialties included cardiothoracic surgery, vascular surgery, plastic surgery, neurosurgery, ophthalmic surgery, general surgery, orthopedics, urology, gynecology, traumatology, anesthesiology, and ear, nose, and throat.
Nonsurgical specialties included cardiology, geriatrics, dermatology, gastroenterology, hematology, internal medicine, nephrology, neurology, oncology, psychiatry, pulmonology, and rheumatology.
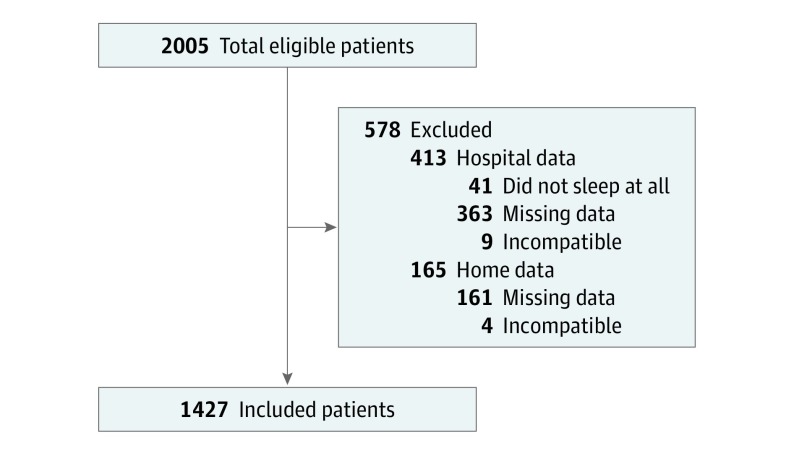
The 1427 patients (71.2%) who provided complete (home and at hospital) answers to all CSD questions were included in the sleep quantity analysis (Figure). The 578 excluded patients (28.8%) did not differ from the included patients with respect to baseline characteristics (eTable 2 in the Supplement).
Figure. Inclusion Quantitative Sleep Measurements.
Raw summary difference scores for the PROMIS questions could be calculated in 1885 patients (94.0%) because of few missing answers in some patients. However, because many patients only forgot to fill out 1 of the 12 questions, we also chose to calculate the difference for each question separately (Table 2).
Table 2. Subjective Sleep Disturbance Scores (PROMIS)a.
| Item | Median (IQR) | Mean Difference (95% CI) |
|---|---|---|
| My sleep quality was | ||
| Home (n = 1958) | 3 (2-3) | 0.58 (0.52 to 0.64) |
| Hospital (n = 1966) | 2 (1-3) | |
| I was satisfied with my sleep | ||
| Home (n = 1960) | 3 (2-3) | 0.60 (0.53 to 0.67) |
| Hospital (n = 1961) | 2 (1-3) | |
| My sleep was refreshing | ||
| Home (n = 1961) | 3 (2-3) | 0.63 (0.56 to 0.70) |
| Hospital (n = 1969) | 2 (1-3) | |
| My sleep was restless | ||
| Home (n = 1951) | 1 (0-2) | −0.45 (−0.52 to −0.38) |
| Hospital (n = 1952) | 1 (0-3) | |
| I had difficulty falling asleep | ||
| Home (n = 1957) | 0 (0-1) | −0.51 (−0.59 to −0.44) |
| Hospital (n = 1958) | 1 (0-3) | |
| I felt lousy when I woke up | ||
| Home (n = 1952) | 0 (0-1) | −0.24 (−0.30 to −0.18) |
| Hospital (n = 1956) | 0 (0-1) | |
| Raw summary score | ||
| Home (n = 1914) | 5 (3-9) | −3.0 (−3.4 to −2.7) |
| Hospital (n = 1921) | 9 (5-14) |
Abbreviations: IQR, interquartile range; PROMIS, Patient-Reported Outcomes Measurement Information System.
Every question was answered using a 5-point scale, scored as follows: 0, very poor/not at all; 1, poor/a little bit; 2, fair/somewhat; 3, good/quite a bit; and 4, very good/very much. A raw summary PROMIS sleep disturbance score was calculated after reverse coding the second and third items. A higher raw summary score indicates more subjective sleep disturbance (range, 0-24). Differences indicate hospital minus home scores. P < .001 for all comparisons.
Sleep Quantity
Table 3 summarizes the CSD measures of subjective sleep quantity. Mean total sleep time was 83 minutes (95% CI, 75-92 minutes) shorter during hospitalization (6 hours 4 minutes; 95% CI, 5 hours 56 minutes to 6 hours 11 minutes) than at home (7 hours 27 minutes; 95% CI, 7 hours 21 minutes to 7 hours 33 minutes) (P < .001). The difference resulted primarily from earlier final awakening in the hospital of a mean of 44 minutes (95% CI, 44-45 minutes). There was a higher number of awakenings in the hospital 3.3 times (95% CI, 3.2-3.5 times) than at home (2.0 times; 95% CI, 1.9-2.1 times) (P < .001). Sleep efficiency was lower in the hospital (76%; 95% CI, 75%-77%) than at home (88%; 95% CI, 88%-89%) (difference, 12%; 95% CI, 14%-11%; P < .001).
Table 3. Subjective Sleep Quantity and Timing Measures (Consensus Sleep Diary)a.
| Measure | Home | Hospital | Difference (95% CI), min | P Value |
|---|---|---|---|---|
| Lights out time | 23:05 (23:01 to 23:08) | 22:57 (22:52 to 23:01) | −8 (−9 to −8) | .002 |
| Sleep onset | 23:29 (23:25 to 23:33) | 23:41 (23:35 to 23:46) | 12 (12 to 12) | <.001 |
| Sleep-onset latency, mean (95% CI), min | 23 (21 to 25) | 44 (40 to 47) | 21 (21 to 21) | <.001 |
| Wake after sleep onset, mean (95% CI), min | 32 (29 to 34) | 61 (57 to 65) | 29 (29 to 29) | <.001 |
| Final wake time | 07:28 (07:24 to 07:32) | 06:44 (06:40 to 06:48) | −44 (−45 to −44) | <.001 |
| Sleep window | 08:23 (08:18 to 08:28) | 07:47 (07:42 to 07:52) | −36 (−36 to −36) | <.001 |
| Total sleep time | 07:27 (07:21 to 07:33) | 06:04 (05:56 to 06:11) | −83 (−92 to −75) | <.001 |
| Sleep efficiency, % (95% CI) | 88 (88 to 89) | 76 (75 to 77) | −12 (−14 to −11) | <.001 |
Home and hospital data are presented as mean clock time in hours:minutes (95% CI) unless otherwise indicated. Differences indicate hospital minus home scores. The summary measures are based on the 1427 patients who provided compatible answers to all Consensus Sleep Diary questions.
Sleep Disturbance
Table 2 summarizes the PROMIS items of subjective sleep disturbance. For all 6 questions (eTable 3 and eFigure 1 in the Supplement), there was a significantly worse rating in the hospital (median, 9; IQR, 5-14) vs at home (median, 5; IQR, 3-9) (P < .001). Raw summary scores and differences in scores were not significantly associated with sex (male: mean, 9.5; 95% CI, 9.1-9.9; female: mean, 10.0; 95% CI, 9.6-10.4; P = .06), length of stay (1 day; mean, 10.5; 95% CI, 9.8-11.1; 2 days: mean, 9.6; 95% CI, 8.9-10.2; 3 days: mean, 9.7; 95% CI, 8.7-10.8; ≥4 days: mean, 9.7; 95% CI, 9.3-10.0; P = .14), or number of patients sleeping in the same room (single room: mean, 9.7; 95% CI, 9.2-10.3; double room: mean, 9.3; 95% CI, 8.8-9.9; triple room: mean, 10.0; 95% CI, 9.1-10.9; quadruple room: mean, 10.0; 95% CI, 9.6-10.5; 5-person room: mean, 10.4; 95% CI, 6.3-14.5; 6-person room: mean, 9.1; 95% CI, 6.7-11.5; >6-person room: mean, 12.0; 95% CI, 0.4-23.5; P = .54). More sleep disturbance was experienced by patients admitted to a surgical unit (score, 10.5; 95% CI, 9.9-11.2) than patients in nonsurgical units (score, 9.6; 95% CI, 9.3-9.9) (P = .02), whereas there was no difference in sleep disturbance between these groups at home. Older patients experienced less sleep disturbance during hospitalization than younger patients. Sleep disturbance at home did not differ across age groups (>36 years old: mean, 6.9; 95% CI, 6.0-7.8; 36-50 years old: mean, 7.0; 95% CI, 6.3-7.7; 51-65 years old: mean, 6.7; 95% CI, 6.3-7.2; 66-80 years old: mean, 6.5; 95% CI, 6.2-7.0; >80 years old: mean, 6.6; 95% CI, 6.0-7.1; P = .84) (eTable 4 and eFigure 2 in the Supplement).
Disturbing Factors
Sleep was negatively associated with at least 1 hospital-related factor in 1276 patients (64.6%). Noise of other patients was the most common disturbing factor, interfering with sleep onset in 473 patients (23.6%). A total of 1696 patients (84.6%) reported at least 1 nocturnal awakening, and 65.8% of all reasons given were hospital related, including noise of other patients (453 [22.6%]) and being awakened by hospital staff (403 [20.1%]). Toilet visits were responsible for nocturnal awakenings in 434 patients (21.6%). Only 566 patients (28.2%) reported to have awakened spontaneously in the morning. Of patients who had not awakened spontaneously, hospital-related reasons were held responsible in 73.7% of the cases. In 718 patients (35.8%), it concerned awakenings by a member of the hospital staff (Table 4 and eTable 5 and eFigure 3 in the Supplement).
Table 4. Sleep-Disturbing Factors.
| Sleep Variablea | No. (%) With ≥1 Reason | Sleep-Disturbing Factors, No. (%)a | Top 3 Sleep-Disturbing Factorsb | |
|---|---|---|---|---|
| Hospital Related | Patient Related | |||
| Sleep-onset latency (n = 1976) | 1276 (64.5) | 4144/6334 (65.4) | 2190/6334 (34.6) | Noise of other patients (23.6%), pain (19.9%), and noise of hospital equipment (19.4%) |
| Nocturnal awakenings (n = 2004) | 1696 (84.6) | 3978/6042 (65.8) | 2064/6042 (34.2) | Other reason (36.4%), noise of other patients (22.6%), and awakened by hospital staff (20.1%) |
| Final awakening (n = 1910) | 1344 (70.4) | 3234/4389 (73.7) | 1155/4389 (26.3) | Awakened by hospital staff (35.8%), other reason (11.6%), and noise of other patients (10.9%) |
Hospital-related reasons include awakened by hospital staff, noise of other patients, noise of hospital staff, noise of medical instruments, uncomfortable bed or pillow, lights, transfer to new room, and other hospital-related answers to the open-ended question. Patient-related reasons include pain, anxiety, worrying about illness, dyspnea, alarm clock, and other patient-related answers to the open-ended question.
Percentages are the proportion of all patients (N = 2005) who experienced the sleep-disturbing factor. In the other factors category, 434 (59.5%) of nocturnal awakenings and 120 (51.4%) of final awakenings were caused by toilet visits; this was not an option included in the survey.
Discussion
To our knowledge, this nationwide, single-day, multicenter, cross-sectional, observational, FMR study is the first large-scale study to examine the prevalence, severity, and factors negatively associated with sleep quantity and sleep quality in hospitalized patients. We found that hospitalized patients slept shorter times with more interruptions, woke up earlier, and experienced poorer sleep quality than at home. In two-thirds of cases, disturbances involved hospital-related factors, of which many seem modifiable.
In line with other studies,9,17,20,27,28 we identified noises and awakenings by medical staff as the most important hospital-related sleep-disturbing factors. Although not included in the list of potential sleep disruptors, an important disturbing factor frequently mentioned by the patients was waking up for toilet visits. Continuous intravenous drips at night and extra diuretics may have contributed to an increased frequency of toilet visits in the hospital. Most of the sleep-disturbing factors found in our study seem easy to address by incorporating simple changes in nightly hospital routines. A recent pilot study29 demonstrated an increase in total sleep time and subjective sleep quality after offering sleep hygiene education to nurses, introducing interventions to minimize light and noise disturbances, and reducing care-related disruptions and overnight fluids.
There was no significant difference in the association with sleep quantity and quality in patients sleeping in a single room compared with patients sleeping in a room with other patients. A probable explanation is that in most Dutch hospitals, the sickest patients are prioritized for sleeping in a single room because of scarcity and need for more care-related disruptions. Most of our population (57%) was older than 65 years and experienced fewer sleep disturbances in the hospital possibly because they are used to more disrupted sleep at home. In addition, sleep disturbance at home did not differ across age groups, possibly because the younger patients were also likely to have a high burden of comorbidity affecting their sleep at home and in the hospital.
We used national newspapers and social media to promote the study, aiming to raise awareness about the existence of sleep disturbances in hospitals and stimulate future research. Future investigation on sleep optimization should focus on interventions such as dimmed lights in corridors and patient rooms, silent footwear, remote alarms in staff rooms and in the pockets of the nurses, and distribution of flight packages at admission that contain earplugs and eye masks. The possibility of introducing remote measurement of vital signs and nocturnal checkups via webcams should also be explored. In addition, changing the timing and minimizing nursing activities early in the morning; avoiding unnecessary standard procedures, such as routine vital signs measurements, continuous intravenous drips at night, and diuretics in the afternoon, could potentially improve sleep. However, to our knowledge, most of these interventions have never been tested in general wards; therefore, prospective interventional studies are needed.
Strengths and Limitations
The main strength of the present study is that by using the FMR design we included a large heterogeneous sample of patients within 1 day. The hospitals were in different regions of the Netherlands and included academic, nonacademic teaching, and nonteaching hospitals in urban and rural areas. Therefore, it was likely that we had a representative sample of the Dutch hospitals.
The study also had some limitations. For the subjective sleep quantity outcomes, almost one-third of the patients had to be excluded because of missing or incompatible data. There were no differences in the demographic characteristics of included and excluded patients; thus, we assumed that the included population was representative of the total study population. In addition, 41 patients reporting “not to have slept at all” the last night in the hospital were excluded because of missing exact time data. This exclusion may have led to an overestimation of sleep duration during hospitalization.
Furthermore, some admitted patients were not eligible for inclusion because of delirium or cognitive problems. Other patients were asleep when the questionnaires were distributed, possibly because they did not sleep enough at night. Some were too ill or exhausted, which may also have led to a conservative estimate of sleep problems during hospitalization.
A downside of using habitual sleep at home during the month before admission is the lack of information about the condition that the patients were in during that period. Habitual sleep patterns may have deviated from usual sleep patterns at home because of illnesses before admission. In addition, recall bias may have led to more positive estimates of in-home sleep and inflated the differences between in-home and in-hospital sleep ratings, which could have led to underestimation of sleep quantity and quality difference at home vs hospital.
Conclusions
This large-scale, multicenter study is the first, to our knowledge, to demonstrate compromised sleep quantity and quality in hospitalized patients and identified many potentially preventable hospital-related factors. Increasing awareness among health care workers of the importance of adequate sleep and introducing interventions that target sleep-disturbing factors in hospitals may lead to better sleep and better health outcomes.
eAppendix. Original Questionnaire
eTable 1. Overview of Use Sleep Medication
eTable 2. Characteristics of Patients Included and Excluded in Analysis on Subjective Sleep Quantity
eTable 3. Distribution of Answers to PROMIS Sleep Quality Items
eTable 4. Differences in Raw Summary Sleep Disturbance Scores Between Groups
eTable 5. Listing of All Disturbing Factors
eFigure 1. Distribution of Raw Summary Sleep Disturbance Scores in the Hospital and at Home
eFigure 2. Raw Summary Sleep Disturbance Scores in the Hospital and at Home in Different Age Groups
eFigure 3. Overview of Disturbing Factors (Before, During, After Sleep Onset)
References
- 1.Gamaldo CE, Shaikh AK, McArthur JC. The sleep-immunity relationship. Neurol Clin. 2012;30(4):1313-1343. [DOI] [PubMed] [Google Scholar]
- 2.Alvarez GG, Ayas NT. The impact of daily sleep duration on health: a review of the literature. Prog Cardiovasc Nurs. 2004;19(2):56-59. [DOI] [PubMed] [Google Scholar]
- 3.Gottlieb DJ, Punjabi NM, Newman AB, et al. . Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863-867. [DOI] [PubMed] [Google Scholar]
- 4.Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, van den Berg JF, Verschuren WM. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN study. Sleep. 2011;34(11):1487-1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manian FA, Manian CJ. Sleep quality in adult hospitalized patients with infection: an observational study. Am J Med Sci. 2015;349(1):56-60. [DOI] [PubMed] [Google Scholar]
- 6.Boonstra L, Harden K, Jarvis S, et al. . Sleep disturbance in hospitalized recipients of stem cell transplantation. Clin J Oncol Nurs. 2011;15(3):271-276. [DOI] [PubMed] [Google Scholar]
- 7.Enomoto M, Tsutsui T, Higashino S, et al. . Sleep-related problems and use of hypnotics in inpatients of acute hospital wards. Gen Hosp Psychiatry. 2010;32(3):276-283. [DOI] [PubMed] [Google Scholar]
- 8.De Rui M, Middleton B, Sticca A, et al. . Sleep and circadian rhythms in hospitalized patients with decompensated cirrhosis: effect of light therapy. Neurochem Res. 2015;40(2):284-292. [DOI] [PubMed] [Google Scholar]
- 9.Yilmaz M, Sayin Y, Gurler H. Sleep quality of hospitalized patients in surgical units. Nurs Forum. 2012;47(3):183-192. [DOI] [PubMed] [Google Scholar]
- 10.Lieberman HR, Bathalon GP, Falco CM, Kramer FM, Morgan CA III, Niro P. Severe decrements in cognition function and mood induced by sleep loss, heat, dehydration, and undernutrition during simulated combat. Biol Psychiatry. 2005;57(4):422-429. [DOI] [PubMed] [Google Scholar]
- 11.Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, Verschuren WM. Sufficient sleep duration contributes to lower cardiovascular disease risk in addition to four traditional lifestyle factors: the MORGEN study. Eur J Prev Cardiol. 2014;21(11):1367-1375. [DOI] [PubMed] [Google Scholar]
- 12.Spiegel K, Leproult R, van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435-1439. [DOI] [PubMed] [Google Scholar]
- 13.Stang A, Moebus S, Möhlenkamp S, Erbel R, Jöckel KH; Heinz Nixdorf Recall Study Investigative Group . Gender-specific associations of short sleep duration with prevalent hypertension. Hypertension. 2008;51(3):e15-e16. [DOI] [PubMed] [Google Scholar]
- 14.Martin JL, Fiorentino L, Jouldjian S, Mitchell M, Josephson KR, Alessi CA. Poor self-reported sleep quality predicts mortality within one year of inpatient post-acute rehabilitation among older adults. Sleep. 2011;34(12):1715-1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watson PL, Ceriana P, Fanfulla F. Delirium: is sleep important? Best Pract Res Clin Anaesthesiol. 2012;26(3):355-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weinhouse GL, Schwab RJ, Watson PL, et al. . Bench-to-bedside review: delirium in ICU patients: importance of sleep deprivation. Crit Care. 2009;13(6):234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pilkington S. Causes and consequences of sleep deprivation in hospitalised patients. Nurs Stand. 2013;27(49):35-42. [DOI] [PubMed] [Google Scholar]
- 18.Dogan O, Ertekin S, Dogan S. Sleep quality in hospitalized patients. J Clin Nurs. 2005;14(1):107-113. [DOI] [PubMed] [Google Scholar]
- 19.Young JS, Bourgeois JA, Hilty DM, Hardin KA. Sleep in hospitalized medical patients, part 1: factors affecting sleep. J Hosp Med. 2008;3(6):473-482. [DOI] [PubMed] [Google Scholar]
- 20.Ghanbari Jolfaei A, Makvandi A, Pazouki A. Quality of sleep for hospitalized patients in Rasoul-Akram hospital. Med J Islam Repub Iran. 2014;28:73. [PMC free article] [PubMed] [Google Scholar]
- 21.Alsma J, van Saase JLCM, Nanayakkara PWB, et al. ; FAMOUS Study Group . The power of flash mob research: conducting a nationwide observational clinical study on capillary refill time in a single day. Chest. 2017;151(5):1106-1113. [DOI] [PubMed] [Google Scholar]
- 22.Cambridge Online Dictionary www.dictionary.cambridge.org. Accessed May 11, 2018.
- 23.Alam N, Oskam E, Stassen PM, et al. . Prehospital antibiotics in the ambulance for sepsis: a multicentre, open label, randomised trial. Lancet Respir Med. 2018;6(1):40-50. [DOI] [PubMed] [Google Scholar]
- 24.Carney CE, Buysse DJ, Ancoli-Israel S, et al. . The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35(2):287-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buysse DJ, Yu L, Moul DE, et al. . Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010;33(6):781-792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Terwee CB, Roorda LD, de Vet HC, et al. . Dutch-Flemish translation of 17 item banks from the patient-reported outcomes measurement information system (PROMIS). Qual Life Res. 2014;23(6):1733-1741. [DOI] [PubMed] [Google Scholar]
- 27.Bano M, Chiaromanni F, Corrias M, et al. . The influence of environmental factors on sleep quality in hospitalized medical patients. Front Neurol. 2014;5:267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lei Z, Qiongjing Y, Qiuli W, Sabrina K, Xiaojing L, Changli W. Sleep quality and sleep disturbing factors of inpatients in a Chinese general hospital. J Clin Nurs. 2009;18(17):2521-2529. [DOI] [PubMed] [Google Scholar]
- 29.Gathecha E, Rios R, Buenaver LF, Landis R, Howell E, Wright S. Pilot study aiming to support sleep quality and duration during hospitalizations. J Hosp Med. 2016;11(7):467-472. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Original Questionnaire
eTable 1. Overview of Use Sleep Medication
eTable 2. Characteristics of Patients Included and Excluded in Analysis on Subjective Sleep Quantity
eTable 3. Distribution of Answers to PROMIS Sleep Quality Items
eTable 4. Differences in Raw Summary Sleep Disturbance Scores Between Groups
eTable 5. Listing of All Disturbing Factors
eFigure 1. Distribution of Raw Summary Sleep Disturbance Scores in the Hospital and at Home
eFigure 2. Raw Summary Sleep Disturbance Scores in the Hospital and at Home in Different Age Groups
eFigure 3. Overview of Disturbing Factors (Before, During, After Sleep Onset)