Abstract
Background
Hamstring tears are well recognised in the sporting population. Little is known about these injuries in the general population.
Purpose
Evaluating the rates, patterns and risk factors of non-sporting hamstring tears, compared to sporting related hamstring tears.
Data Sources
MEDLINE, EMBASE, CINAHL, and the Cochrane Central Register of Controlled Trials (1989–2015).
Study Selection
Studies reporting patients with a grade 2 or 3 hamstring muscle tear, identified clinically, confirmed by MRI imaging or direct visualisation during surgical exploration.
Data Synthesis
144 sets of linked data were extracted for analysis. Most injuries were in males (81.3%), where mean age at injury was lower (30.2, 95% CI 29.1–31.3) than in females (35.4, 95% CI 32.4–38.4) p = 0.06. Key differences were found in the proportion of non-sporting injuries in patients under and over the age 40 (p = 0.001). The proportion of non-sporting injuries was significantly higher in females compared to males (25.9% female non-sporting injuries, versus 8.5% male; p = 0.02). Avulsions were more frequently reported in non-sporting activities (70.5%). The proportion of such injuries was notably higher in females, though this failed to meet significance (p = 0.124). Grouped by age category a bimodal distribution was noted, with the proportion of avulsions greater in younger (age <15) and older patients (age > 40) (p = 0.008). 86.8% of patients returned to pre-injury activity levels with a similar frequency across all study variables; age, activity (sporting vs non-sporting) and injury type (avulsion vs tear).
Conclusion
This review highlights a proportion of adults suffering grade 2 or 3 hamstring injuries from activities other than the classic sports trauma. The majority of these non-sporting injuries were avulsion injuries that clustered in older female and skeletally immature patients suggesting a potential link to bone mineral density.
Introduction
Hamstring tears are commonly reported in professional sports players.[1–3] In contrast, the prevalence of hamstring tears in recreational-sporting and non-sporting situations is poorly defined. This lack of data is especially true for older individuals, who are known amongst clinicians to present to general practice and orthopaedic clinics with hamstring tears, yet their prevalence is unknown. Patients suffering a hamstring tear due to sport are mainly in the second and third decade of life.[4, 5] In contrast, the age range of patients with non-sporting or recreational injuries is much greater with hamstring tears reported in patients aged 60 years and over.[1, 6, 7]
A muscle strain is an anatomical and functional disruption of the muscle-tendon unit.[8] Severity of injury is based on the extent of tissue damage, inflammatory response and loss of function. The most common classification system defines a grade 1 injury as no appreciable tissue disruption, mild pain and swelling and no or minimal loss of function, Grade 2 injuries as an identifiable partial disruption of the tissue with moderate pain and swelling thereby leading to loss of function, and grade 3 as complete disruption or tear of the musculotendonous unit with severe pain and swelling and lack of function.[9]
Reports describing hamstring injury diagnosis and management highlight considerable time differences from injury to presentation from several hours to many years.[1, 10] Typical findings on examination include localised tenderness, swelling and a palpable defect. This marked heterogeneity in presenting signs and symptoms along with the sometimes insidious development may lead to delayed presentation and late diagnosis. Diagnosis is aided by imaging, either by plain X-ray to detect bony avulsion fractures or with MRI and ultrasound, which can detail the extent of the injury.[11–14]
Despite their high prevalence, there is a remarkable lack of consensus on hamstring injury management. Recent systematic reviews by Ropiak et al and Ahmad et al suggest that Grade 1 and Grade 2 injuries are typically treated non-operatively.[11, 15] This may encompass rest, ice, compression and progressive mobilization as well as the use of analgesia and non-steroidal anti-inflammatories. The outcome of these partial tears is considered to be varied and unpredictable. Grade 3 injuries and those presenting following failed conservative treatment are often repaired surgically. Good functional outcomes have been reported with operative repair.[1, 16, 17] Correct identification and treatment of suspected hamstring injuries is therefore of high importance.
The aim of this study was to determine the incidence of the injury in both professional and recreational sports people as well as in the remainder of the population, who do not play sport. In particular, our aim was to identify any differences in the type of injury between these groups.
Methods
Literature search method
Four major databases were systematically searched in January and February 2015: MEDLINE, EMBASE, CINAHL and the COCHRANE LIBRARY. The complete electronic search history is detailled in S1 Table. Additionally, reference lists of eligible publications for further articles were manually scanned. The search was time limited from January 1989 to January 2015. Two reviewers (BK and SBP) independently read title and abstract of publications identified by the searches potentially meeting the eligibility criteria. Both reviewers read those publications considered relevant in full text to verify they met the eligibility criteria. A third reviewer (DFH) was consulted where initial agreement was not reached.
Study eligibility criteria
We focused our review on grade 2 and 3 hamstring injuries. To be included, the details of the hamstring injury (distal versus proximal, muscles involved, injury type) had to be stated and confirmed by either imaging (CT, MRI) or by visualisation through surgical exploration, or both. Hamstring avulsion fractures were included, and treatment modality recorded (surgery or conservative management). We required patient age and injury mechanism to be stated. The publication language was English. All data was reviewed including retrospective and case study literature so long as the previous criteria was met.
The search resulted in a total of 6237 papers: 849 from MEDLINE (via Ovid 23/01/15), 4842 from EMBASE (via Ovid 1/02/15), 4 from the COCHRANE LIBRARY (1/02/15) and 542 from CINAHL (via EbcsoHost 1/02/15). Following exclusions, 53 papers met the inclusion criteria leading to a final data set of 144 hamstring injuries. The study selection process is shown in Fig 1. The majority of studies included were individual case reports (44) with a smaller number of retrospective case series (2) and a single prospective case series (Table 1).
Fig 1. Study Selection Process.
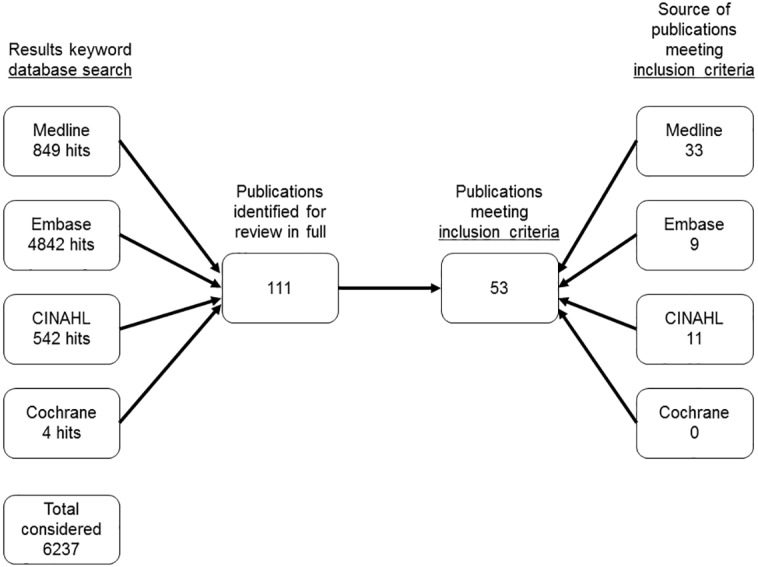
Table 1. Publications summary chart.
| Authors | Year | Study design | Number of subjects | non-sporting injury | Subject age (years) |
|---|---|---|---|---|---|
| Adejuwon A, et al.[18] | 2009 | Case series | 2 | 0 | 19, 25 |
| Alioto RJ, et al.[19] | 1997 | Case report | 1 | 0 | 25 |
| Akova B, et al.[20] | 2002 | Case report | 1 | 0 | 17 |
| Al-Humadi M, et al.[21] | 2009 | Case report | 1 | 1 | 30 |
| Askling C, et al.[22] | 2000 | Case series | 2 | 0 | 20, 22 |
| Bansal R, et al.[23] | 2005 | Case report | 1 | 0 | 19 |
| Biedert RM [24] | 2015 | Case Series | 3 | 0 | 13, 14, 15 |
| Boŝnjak R.[25] | 2009 | Case report | 1 | 0 | 48 |
| Bruckner PU, et al.[26] | 2005 | Case series | 8 | 1* | 23–60 (44*) |
| Carmody C, et al.[27] | 1995 | Case report | 1 | 0 | 44 |
| Clark B, et al.[28] | 2011 | Case report | 1 | 0 | 26 |
| Cross MJ, et al.[29] | 1998 | Retrospective review | 9 | 1 | 54 |
| Cooper D, et al.[5] | 2010 | Case series | 17 | 0 | 22–39 |
| Cotofana S, et al.[30] | 2012 | Case report | 1 | 1 | 49 |
| Croisier JL, et al.[31] | 2005 | Case reports | 2 | 0 | 33, 47 |
| David A, et al.[32] | 1994 | Case report | 1 | 0 | 41 |
| Floor S, et al.[33] | 2012 | Case reports | 2 | 0 | 44,45 |
| Fortems Y, et al.[34] | 1995 | Case reports | 2 | 1* | 44 (42*) |
| Gidwani S, et al.[35] | 2007 | Retrospective review | 11 | 0 | 9–51 |
| Grieve R, et al.[36] | 2006 | Case report | 1 | 0 | 26 |
| Hernesman SC, et al.[6] | 2003 | Case report | 1 | 0 | 68 |
| Johnson AE, et al.[37] | 2003 | Case report | 1 | 1 | 36 |
| Khoshnoodi P, et al. [38] | 2014 | Case report | 1 | 0 | 26 |
| Kirkland A, et al.[39] | 2008 | Case report | 1 | 0 | 24 |
| Konan S, et al.[4] | 2010 | Prospective review | 10 | 0 | 24–38 |
| Kurosawa H, et al.[40] | 1996 | Case reports | 2 | 0 | 25, 28 |
| Kusma M, et al.[41] | 2007 | Case report | 1 | 0 | 43 |
| Kwak HY, et al.[42] | 2011 | Case reports | 2 | 0 | 16, 24 |
| Kwong Y, et al.[43] | 2006 | Case report | 1 | 1 | 62 |
| LaBan MM, et al. [7] | 2007 | Case report | 1 | 1 | 64 |
| Lempainen L, et al.[10] | 2007 | Case series | 18 | 0 | 18–40 |
| Lin YT, et al. [44] | 2008 | Case report | 1 | 0 | 21 |
| Lindner D, et al. [45] | 2014 | Case report | 1 | 0 | 16 |
| Mallo G, et al.[46] | 2009 | Case report | 1 | 0 | 29 |
| Marx RG, et al.[47] | 2009 | Case reports | 2 | 1* | 30, 30* |
| Mascarenhas R, et al.[48] | 2009 | Case report | 1 | 1 | 22 |
| McGoldrick F, et al.[49] | 1990 | Case report | 1 | 0 | 36 |
| Mica L, et al.[50] | 2009 | Retrospective review | 6 | 6* | (48–73)* |
| Murray PJ, et al.[51] | 2009 | Case report | 1 | 0 | 56 |
| Oseto MC, et al.[52] | 2004 | Case report | 1 | 0 | 39 |
| Pan KL, et al. [53] | 2000 | Case report | 1 | 1 | 33 |
| Schache AG, et al.[54] | 2008 | Case report | 1 | 1 | 20 |
| Scilia A, et al.[55] | 2011 | Case report | 1 | 0 | 55 |
| Sebastianelli WJ, et al.[56] | 1990 | Case report | 1 | 0 | 21 |
| Servant CTJ, et al. [57] | 1998 | Case report | 1 | 0 | 16 |
| Shyamalan G, et al.[58] | 2010 | Case series | 8 | 2* | 11–34 (22*,41*) |
| Sikka RS, et al. [59] | 2013 | Case series | 3 | 0 | 12, 16, 16 |
| Sonnery-Cottet B, et al.[60] | 2012 | Case report | 1 | 0 | 24 |
| Stradley SL, et al.[61] | 2008 | Case report | 1 | 0 | 43 |
| Takami H, et al. [62] | 2000 | Case report | 1 | 0 | 27 |
| Thomson NOB, et al. [63] | 1999 | Case report | 1 | 0 | 39 |
| Valente M, et al. [64] | 2013 | Case report | 1 | 0 | 24 |
| Watura C, et al.[65] | 2011 | Case report | 1 | 0 | 42 |
*highlight the age of the non-sporting cases in that report.
Statistical analysis
Data from eligible studies and subjects was collated and analysed using SPSS version 19. Data was reported by mean with 95% confidence intervals as a measure of dispersion. Pearson’s Chi Square, Fisher’s Exact Tests and the Student’s t-test were used to determine association between variables.
Results
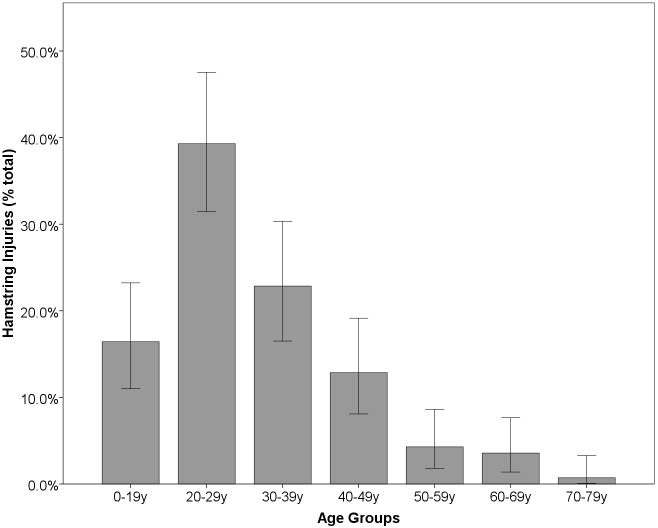
The mean age of patients across the study population was 31.1 (95% CI 30.1–32.3). Patient age ranged from 9 to 73 years. The majority (72.2%) of hamstring injuries reported were observed in patients in their 20s and 30s (Fig 2). Most injuries were reported in males (81.3%). Mean age at injury in males was lower (30.2, 95% CI 29.1–31.324) than in females (35.4, 95% CI 32.4–38.4) with this difference approaching significance (Students t-test, p = 0.06).
Fig 2. Distribution of reported injuries by age group.
Injurious activity
88.2% of hamstring injuries were described as being sustained during sporting activities (50% of these were in professional or competitive athletes). The most common sporting activities were ball sports (44.4%), running (24.3%), skiing/water skiing (13.2%) and contact sports/martial arts(6.3%). The remaining 11.8% of hamstring injuries were sustained during 'non-sporting' activities; these ranged from a single high impact trauma, road traffic accident, (0.7%) to low impact falls slips and trips (11.1%).
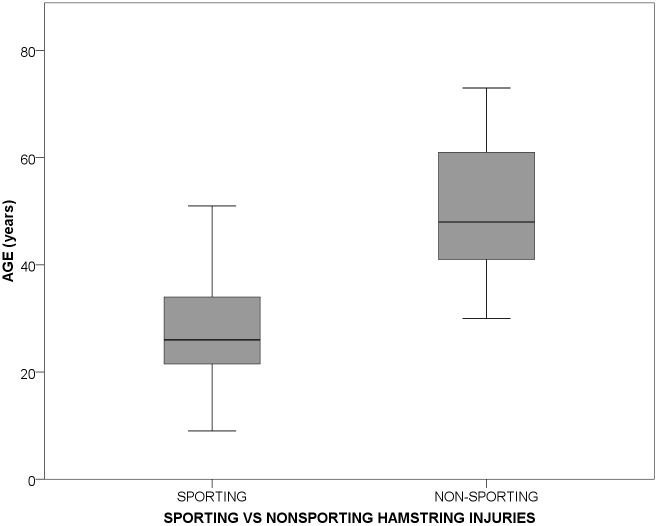
The mean age of patients with a hamstring injury as a result of playing sport was 28.7 (95% CI 27.7–29.7), compared to a mean age of 49.5 (95% CI 43.0–56.1) in patients with a non-sporting hamstring injury. This difference was statistically significant (p<0.001, Students t-test, Fig 3).
Fig 3. Distribution of injuries comparing sports versus non-sports aetiologies and age.
Gender was related to both activity of injury and injury type. The proportion of non-sporting injuries was significantly higher in females compared to males (25.9% of female injuries were non-sporting, compared to 8.5% of male injuries; p = 0.02).
Injury type
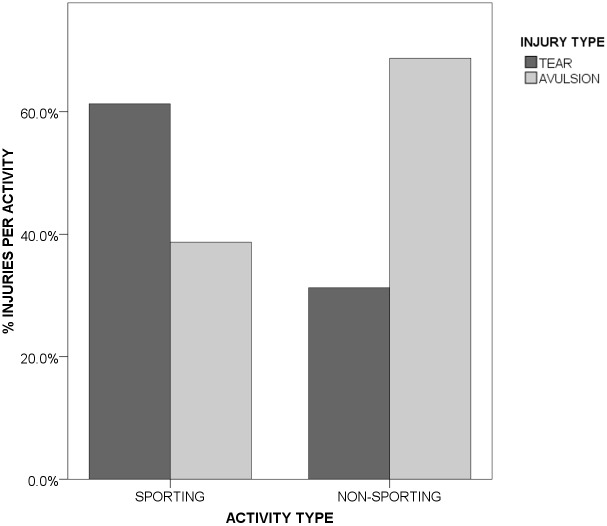
Tears (of muscle or tendon) were the most common injury report (57.6%) the remaining 42.4% being avulsions (of tendon origin/insertion to bone). Avulsion injuries were significantly more common in patients injured during non-sporting activities (70.5%) compared to sports related injuries (38.6%, Fig 4)(p = 0.012, Pearson’s Chi-square test).
Fig 4. Distribution of injury type by sports participation.
The proportion of avulsion injuries was notably higher in females (55.6% of injuries in females were avulsions, compared to 39.3% of injuries in males) compared to males, though this failed to meet significance (p = 0.124, Pearson’s Chi-square test). The mean age was similar across tear and avulsion injury groups (tear30.1y 95% CI 28.1–32.1; avulsion 32.0y 95% CI 29.9–34.1). However, when grouped by age category, the distribution of avulsion injuries was apparently bimodal, being significantly higher in patients below the age of 15 and in patients above the age of 40, compared to those between ages 15 and 39 years (Pearson Chi-Square, p = 0.008).
Outcomes
Reporting on return to activity was not available for four patients; these patients were excluded from analysis assessing return to pre-injury activity level (the remaining 140 patients were included). 86.8% of patients were described as returning to pre-injury activity levels. There was no difference in age between those who did (30.8yrs, 95%CI 29.6–32.0) and those who did not (30.1yrs, 95%CI 27.5–32.7) return to pre-injury function (Student's t-test, p = 0.798).
Discussion
Hamstring tears typically occur during rapid acceleration/deceleration involving sudden forced hip flexion concomitant with knee extension, and are well documented to occur as a result of sporting activities. [1, 16] Many studies have assessed the incidence, risk factors and severity of hamstring injuries in professional athletes, perhaps in whom there is a strong economic interest in defining the injury and expediting player return. [66, 67] Our review takes a different approach, assessing all reported hamstring injuries with defined mode of injury including those caused by non-sporting activities. By doing so the patient cohort extends across a much large range.
The principle findings of this systematic review of linked data was a population of individuals injuring their hamstrings in non-sporting situations. These ‘non-sporting injuries’ were more likely in females, in an older demographic and tended to be avulsions of the hamstring origins/insertions to the bone as opposed to tears of the muscle belly
As is typically reported, most hamstring injuries were due to sporting activities, however we highlight a proportion of injuries caused by simple low impact falls and slips; This has not been well described previously. We identified one report looking at non-athletes that described six patients where flexion of the hip with hyperextension of the knee during everyday activities such as missing a step during walking or gardening led to complete hamstring avulsions. [50]
The mean age of people sustaining a non-sporting injury was significantly greater than the age of those suffering sporting injuries. This is in keeping with the current literature, however, the heavily skewed demographic split towards females and the proportion of muscle injury/ avulsion injuries differing between sporting and non-sporting groups are new findings. It is of interest that the avulsions cluster in younger and older individuals, which is consistent witha possible association with skeletal maturity and bone mineral density (BMD). This association between BMD and avulsion/mid substance tendon tear has been previously recognized in different injury sites, namely the calcaneus/Achilles tendon and tibial tubercle/patella tendon; Wren et al demonstrated in a cadaver model that tendo-achilles avulsion injuries were related to reduced calcaneal bone density [68], a finding confirmed in osteoporotic bone and diabetic patients. [69–71] These are most commonly reported in the older patient and are typically the result of minor trauma such as accidental trips causing falls.[72] Similarly, the site where the extensor mechanism of the knee fails varies with age [73], with avulsions occurring at the tibial tubercle/inferior pole of the patella in immature patients and at the superior pole of the patella in older adults.
We suggest that the relatively small number of hamstring injuries reported in non-sporting situations may be a feature of selection bias and an under-representation of the true picture across the general population, as has been observed in other conditions [74]. This is compounded by problems with mis-diagnosis and coding. Hamstring injuries most commonly present with buttock pain, however the differential diagnosis of buttock pain is extensive and includes pathologies in the back, hip and groin. Referred pain from the lumbo-sacral spine may present as ill-defined posterior thigh or buttock pain and is a common presentation in general practice.[11, 75, 76] and may be confused with hamstring tears. In contrast, athletic and surgical cohorts are relatively well coded, in contrast coding of hamstring injuries in general practice is not well defined, again suggesting that hamstring tears in the community may be comparatively under-reported. In the sports medicine literature it is suggested that failing to diagnose a hamstring tear may lead to mismanagement, which may have a detrimental impact on outcome. Although surgical repair of chronic tears can be successful, the procedure is more complex, potentially requiring neurolysis of the sciatic nerve and the outcome is less predictable; consequently early repair is generally recommended [16, 77]. This though is in relation to athletes. The available literature does not confirm whether this same principle applies to the wider population.
Strengths and Weaknesses
The main limitation of this analysis of linked data was the inability to proceed to formal meta-analysis. This was due to the overall poor quality of study variable definition in the individual reports.
However, despite this limitation, it has identified a population of hamstring tears due to non-sporting injuries, particularly in females, which should be considered in the differential diagnosis of hip pain following a low energy fall. Further research is needed in this group to ascertain the most appropriate intervention and management especially in those where there is an avulsion fracture.
Conclusion
This review highlights a largely unrecognised population of adults suffering hamstring injuries from low-impact activities. These tend to be avulsion injuries that cluster in the older female and skeletally immature patients suggesting a potential link to bone mineral density.
Supporting Information
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We would like to thank Mrs Sheila Fisken, liaison librarian at the University of Edinburgh Medical School, for her invaluable knowledge and contribution to the design of the literature searches of this review.
Data Availability
All relevant data are within the data and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1.Wood DG, Packham I, Trikha SP, Linklater J. Avulsion of the Proximal Hamstring Origin. J Bone Joint Surg Am 2008;90(11):2365–74. 10.2106/JBJS.G.00685 [DOI] [PubMed] [Google Scholar]
- 2.Lempainen L, Sarimo J, Heikkilä J, Mattila K, Orava S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med 2006;40(8):688–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Askling C, Lund H, Saartok T, Thorstensson A. Self-reported hamstring injuries in student dancers. Scand J Med Sci Sports 2002;12(4):230–235. [DOI] [PubMed] [Google Scholar]
- 4.Konan S, Haddad F. Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop 2010;34(1):119–23. 10.1007/s00264-009-0739-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper DE, Conway JE. Distal semitendinosus ruptures in elite-level athletes: low success rates of nonoperative treatment. Am J Sports Med 2010;38(6):1174–8. 10.1177/0363546509361016 [DOI] [PubMed] [Google Scholar]
- 6.Hernesman SC, Hoch AZ, Vetter CS, Young CC. Foot drop in a marathon runner from chronic complete hamstring tear. Clin J Sport Me. 2003;13(6):365–8. [DOI] [PubMed] [Google Scholar]
- 7.LaBan MM, McNeary L. An avulsion of the semitendinosus and biceps femoris conjoined tendons. Am J Phys Med Rehabil 2008;87(2):168 10.1097/PHM.0b013e318161982d [DOI] [PubMed] [Google Scholar]
- 8.Garrett WE Jr. Muscle Strain Injuries. Am J Sports Med 1996;24(6):S2–8. [PubMed] [Google Scholar]
- 9.O’Donoghue DH. Introduction: treatment of injuries to athletes: 1962. Clin Orthop Relat Res 2002;402:3–8. [DOI] [PubMed] [Google Scholar]
- 10.Lempainen L, Sarimo J, Mattila K, Heikkilä, Orava S, Puddu G. Distal tears of the hamstring muscles: review of the literature and our results of the surgical treatment. Br J Sports Med 2007;41(2):80–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ropiak CR, Bosco JA. Hamstring injuries. Bull NYU Hosp Jt Dis 2012;70(1):41–8. [PubMed] [Google Scholar]
- 12.Colosimo AJ, Wyatt HM, Frank KA, Mangine RE. Hamstring avulsion injuries. Oper Tech Sports Med 2005;13(1):80–8. [Google Scholar]
- 13.Koulouris G, Connell D. Hamstring muscle complex: an imaging review. Radiographics 2005;25(3):571–586. [DOI] [PubMed] [Google Scholar]
- 14.Kerkhoffs GM, van Es N, Wieldraaijer T, Sierevelt IN, Ekstarnd J, van Dijk CN. Diagnosis and prognosis of acute hamstring injuries in athletes. Knee Surg Sports Traumatol Arthrosc 2013;21(2):500–9. 10.1007/s00167-012-2055-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmad CS, Redler LH, Ciccotti MG, Maffulli N, Longo UG, Bradley J. Evaluation and management of hamstring injuries. Am J Sports Med 2013;41(12):2933–47. 10.1177/0363546513487063 [DOI] [PubMed] [Google Scholar]
- 16.Folsom GJ, Larson CM. Surgical treatment of acute versus chronic complete proximal hamstring ruptures: results of a new allograft techniques for chronic reconstructions. Am J Sports Med 2008;36(1):104–9. [DOI] [PubMed] [Google Scholar]
- 17.Cohen S, Rangavajjula A, Vyas D, Bradley JP. Functional results and outcomes after repair of proximal hamstring avulsions. Am J Sports Med. 2012. 40(9):2092–8. 10.1177/0363546512456012 [DOI] [PubMed] [Google Scholar]
- 18.Adejuwon A, McCourt P, Hamilton B, Haddad F. Distal semitendinosus tendon rupture: Is there any benefit of surgical intervention? Clin J Sport Med 2009;19(6):502–4. 10.1097/JSM.0b013e3181bd09c7 [DOI] [PubMed] [Google Scholar]
- 19.Alioto RJ, Browne JE, Barnthouse CD, Scott AR. Complete rupture of the semimembranous complex in a professional athlete. Clin Orthop Relat Res 1997;336:162–5. [DOI] [PubMed] [Google Scholar]
- 20.Akova B, Okay E. Avulsion of the ischial tuberosity in a young soccer player: six years follow-up. J Sports Sci Med 2002;1(1):27–30. [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Humadi H, Fulkerson EW, Egol KA. Semimembranosus tendon mediated avulsion fracture of the posteromedial tibial plateau. J Trauma 2009;66(1):E1–E3. 10.1097/01.ta.0000242218.33654.2c [DOI] [PubMed] [Google Scholar]
- 22.Askling C, Tengvar M, Saartok T, Thorstensson A. Sports related hamstring strains –two cases with different etiologies and injury sites. Scand J Med Sci Sports 2000;10(5):304–7. [DOI] [PubMed] [Google Scholar]
- 23.Bansal R, Taylor C, Pimpalnerkar AL. Snapping knee: an unusual biceps femoris tendon injury. Knee 2005;12(6):4 58–60. [DOI] [PubMed] [Google Scholar]
- 24.Biedert RM. Surgical management of traumatic avulsion of the ischial tuberosity in young athletes. Clin J Sport Med 2015;25(1):6772. [DOI] [PubMed] [Google Scholar]
- 25.Bošnak R, Mofardin S, Derham C. Delayed sciatic neuropathy after distal semimembranosus muscle rupture associated with tethering of the sciatic nerve by rare distal muscular branch. Injury 2009;40(2):226–9. 10.1016/j.injury.2008.09.024 [DOI] [PubMed] [Google Scholar]
- 26.Bruckner PU, Imhoff AB. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports Traumatol Arthroscop 2005;13(5):411–8. [DOI] [PubMed] [Google Scholar]
- 27.Carmody C, Prietto C. Entrapment of the sciatic nerve as a late sequela of injury to the hamstring muscles: a case report. J Bone Joint Surg Am. 1995;77(7):1100–2. [DOI] [PubMed] [Google Scholar]
- 28.Clark BB, Jaffe D, Henn RF 3rd, Lovering RM. Evaluation and imaging of an untreated grade III hamstring tear: a case report. Clin Orthop Rel Res 2011;469(11):3248–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cross MJ, Vandersluis R, Wood D, Banff M. Surgical repair of chronic complete tendon rupture in the adult patient. Am J Sports Med 1998;26(6):785–8. [DOI] [PubMed] [Google Scholar]
- 30.Cotofana S, Tillman B, Pufe T, Lehrer S, Watz D, Zangl M, et al. Mechanisms of proximal hamstring rupture in a non-athlete healthy middle-aged female. Ann Anat 2012;194(5):489–493. 10.1016/j.aanat.2012.02.016 [DOI] [PubMed] [Google Scholar]
- 31.Croisier JL, Bartsch V, Burnel M, Zeevaert B. Isokinetic assessment of complete proximal hamstring tendon rupture: case reports. Isokinet Exerc Sci 2005;13(1):14–15. [Google Scholar]
- 32.David A, Buchholz J, Muhr G. Tear of the bipceps femoris tendon. Arch Orthop Trauma Surg 1994;113(6):351–2. [DOI] [PubMed] [Google Scholar]
- 33.Floor S, van der Veen AH, Devilee RJ. Two patients with a complete proximal rupture of the hamstring. Arch Orthop Trauma Surg 2010;130(4):523–6 10.1007/s00402-009-0950-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fortems Y, Victor J, Dauwe D, Faubry G. Isolated complete rupture of biceps femoris tendon. Injury 1995;26(4):275–6. [DOI] [PubMed] [Google Scholar]
- 35.Gidwani S, Bircher MD. Avulsion injuries of the hamstring origin –a series of 12 patients and management algorithm. Ann R Coll Surg Engl 2007;89(4):394–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grieve R. Proximal hamstring rupture, restoration of function without surgical intervention: a case study on myofascial trigger point pressure release. J Bodyw Mov Ther 2006;10(2):99–104. [Google Scholar]
- 37.Johnson AE, Granville RR, DeBerardino TM. Avulsion of the common hamstring tendon in an active duty airman. Mil Med 2003;168(1):40–2. [PubMed] [Google Scholar]
- 38.Khoshnoodi P, Tehranzadeh AD, Dunn JM, Tehranzadeh J. Semimembranosus tendon avulsion fracture of the posteromedial tibial plateau associated with posterior cruciate ligament tear and capsular rupture. Skelt Radiol. 2014;43:239–42. [DOI] [PubMed] [Google Scholar]
- 39.Kirkland A, Garrison C, Singleton S, Rodrigo J, Boettner F, Stuckey S. Surgical and therapeutic management of a complete proximal hamstring avulsion after failed conservative approach. J Orthop Sports Phys Ther 2008;38(12):754–60. 10.2519/jospt.2008.2845 [DOI] [PubMed] [Google Scholar]
- 40.Kurosawa H, Nakasita K, Nakasita H, Sasaki S, Takeda S. Complete avulsion of the hamstring tendons from the ischial tuberosity. A report of two cases sustained in judo. Br J Sports Med 1996;30:72(1)–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kusma M, Seil R, Kohn D. Isolated avulsion of the biceps femoris insertion-injury patterns and treatment options: a case report and literature review. Arch Orthop Trauma Surg 2007;127(9):777–80. [DOI] [PubMed] [Google Scholar]
- 42.Kwak HY, Bae SW, Choi YS, Jang MS. Early surgical repair of acute complete rupture of the proximal hamstring tendons. Clin Orthop Surg 2011;3(3):249–5. 10.4055/cios.2011.3.3.249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kwong Y, Patel J, Ramanathan EB. Spontaneous complete hamstring avulsion causing posterior thigh compartment syndrome. Br J Sports Med 2006;40(8):723–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lin Y-T, Chiu Y-N, Lin H-W, Wang T-G. Sonographic diagnosis of nontraumatic musculotendinous rupture of hamstring. J Med Ultrasound 2008;16(3):233–6. [Google Scholar]
- 45.Lindner D, Trenga AP, Stake CE, Jackson TJ, El Bitar YF, Domb BG. Endoscopic repair of a chronic incomplete proximal hamstring avulsion in a cheerleader. Clin J Sport Med. 2014;24(1):83–6. 10.1097/JSM.0b013e31829611b1 [DOI] [PubMed] [Google Scholar]
- 46.Mallo GC, Stanat SJC, Al-Humadi M, Divaris N. Posterior thigh compartment syndrome as a result of a basketball injury. Orthopedics 2009;32(12):923 10.3928/01477447-20091020-19 [DOI] [PubMed] [Google Scholar]
- 47.Marx RG, Fives G, Chu SK, Daluiski A, Wolfe SM. Allograft reconstruction for symptomatic chronic complete proximal hamstring tendon avulsion. Knee Surg Sports Traumatol Arthrosc 2009;17(1):19–23. 10.1007/s00167-008-0588-9 [DOI] [PubMed] [Google Scholar]
- 48.Mascarenhas R, Mcrae S, MacDonald PB. Semitendinosus allograft reconstruction of chronic biceps femoris rupture at the knee. J Knee Surg 2009;22(4):381–4. [DOI] [PubMed] [Google Scholar]
- 49.McGoldrick F, Colville J. Spontaneous rupture of the biceps femoris. Arch Orthop Trauma Surg 1990;109(4):234 [DOI] [PubMed] [Google Scholar]
- 50.Mica L, Schwaller A, Stoupis C, Penka I, Vomela J, Vollenweider A. Avulsion of the hamstring muscle group: A follow-up of 6 adult non-athletes with early operative treatment: a brief report. World J Surg 2009;33(8):1605–10. 10.1007/s00268-009-0099-y [DOI] [PubMed] [Google Scholar]
- 51.Murray PJ, Lowe WR. Achilles allograft reconstruction of a chronic complete proximal hamstring rupture. Knee Surg Sports Traumatol Arthrosc 2009;17(11):1360–3. 10.1007/s00167-008-0670-3 [DOI] [PubMed] [Google Scholar]
- 52.Oseto MC, Edwards JZ, Acus RW. Posterior thigh compartment syndrome associated with hamstring avulsion and chronic anticoagulation therapy. Orthopedics 2004;27(2):229–30. [DOI] [PubMed] [Google Scholar]
- 53.Pan KL, Ting F. Delayed repair of rupture of the biceps femoris tendon –a case report. Med J Malaysia 2000;55(3):368–70. [PubMed] [Google Scholar]
- 54.Schache AG, Koulouris G, Kofoed W, Morris HG, Pandy MG. Rupture of the conjoint tendon at the proximal musculotendinous junction of the biceps femoris long head: a case report. Knee Surg Sports Traumatol Arthrosc 2008;16(8):797–802. 10.1007/s00167-008-0517-y [DOI] [PubMed] [Google Scholar]
- 55.Scillia A, Choo A, Milman E, McInerney V, Festa A. Snapping of the proximal hamstring origin: a rare cause of coxa saltans: a case report. J Bone Joint Surg Am 2011;93(21):e125(1–3). [DOI] [PubMed] [Google Scholar]
- 56.Sebastianelli WJ, Hanks GA, Kalenak A. Isolated avulsion of the biceps femoris insertion: a case report. Clin Orthop Relat Res 1990;259:200–3. [PubMed] [Google Scholar]
- 57.Servant CTJ, Jones CB. Displaced avulsion of the ischial apophysis: a hamstring injury requiring internal fixation. Br J Sports Med 1998;32:255–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shyamalan G, Bircher M. Chronic complete proximal hamstring injury: The double-window approach for bony avulsions. Injury 2010;41(8):823–6. 10.1016/j.injury.2010.03.022 [DOI] [PubMed] [Google Scholar]
- 59.Sonnery-Cottet B, Archbold P, Thaunat M, Fayard J-M, Canuto SMG, Cucurrulo T. Proximal hamstring avulsion in a professional soccer player. Orthop Traumatol Surg Res 2012;98:928–31. 10.1016/j.otsr.2012.05.007 [DOI] [PubMed] [Google Scholar]
- 60.Sikka RS, Fetzer GB, Fischer DA. Ischial apophyseal avulsions: Proximal hamstring repair with bony fragment excision. J Pediatr Orthop. 2013;33(8):e72–4. 10.1097/BPO.0000000000000076 [DOI] [PubMed] [Google Scholar]
- 61.Stradley SL, Backs RA, Grosel J, Kaeding CC. Hamstring avulsion repair without using a flexing splint. JAAPA 2008;21(1):33–7. [DOI] [PubMed] [Google Scholar]
- 62.Takami H, Takahashi S, Ando M. Late sciatic nerve palsy following avulsion of the biceps femoris muscle from the ischial tuberosity. Arch Orthop Trauma Surg 2000;120:352–4. [DOI] [PubMed] [Google Scholar]
- 63.Thomson NOB, Jensen TT. Late repair of rupture of the hamstring tendons from the ischial tuberosity –a case report. Acta Orthop Scand 1999;70(1):89–91. [DOI] [PubMed] [Google Scholar]
- 64.Valente M, Mancuso F, Alecci V. Isolated rupture of biceps femoris tendon. Musculoskelet Surg. 2013;97:263–6. 10.1007/s12306-011-0171-2 [DOI] [PubMed] [Google Scholar]
- 65.Watura C, Harries W. Biceps femoris tendon injuries sustained while playing hockey. BMJ Case Rep 2011. Available: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3062872/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Woods C, Hawkins RD, Maltby S, Hulse M, Thomas A, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football-analysis of hamstring injuries. Br J Sports Med 2004;38(1):36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gabbe BJ, Finch CF, Bennell KL, Wajswelner H. Risk factors for hamstring injuries in community level Australian football. Br J Sports Med 2005;39:106–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wren TA, Yerby SA, Geaupré GS, Carter DR. Influence of bone mineral density, age and strain rate on the failure of human Achilles tendons. Clin Biomech (Bristol, Avon) 2001;16(6):529–3. [DOI] [PubMed] [Google Scholar]
- 69.Kathol MH, el-Khoury GY, Moore TE, Marsh JL. Calcaneal insufficiency fractures in patients with diabetes mellitus. Radiology 1991;180(3):725–9. [DOI] [PubMed] [Google Scholar]
- 70.Hedlund LJ, Maki DD, Griffiths HJ. Calcaneal fractures in the diabetic patients. J Diabetes Complications 1998;12(2):81–7. [DOI] [PubMed] [Google Scholar]
- 71.Squires B, Allen PE, Livingston J, Atkins RM. Fractures of the tuberosity of the calcaneous. J Bone Joint Surg [B] 2001;83-B:55–61. [DOI] [PubMed] [Google Scholar]
- 72.Lee S-M, Huh S-W, Chung J-W, Kim DW, Kim YJ, Rhee SK. Avulsion fractures of the calcaneal tuberosity: classification and its characteristics. Clin Orthop Surg 2012;4(2):134–8. 10.4055/cios.2012.4.2.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Peat G, Birrell F, Cumming J, Doherty M, Simpson H, Conaghan PG;Arthritis Research UK Clinical Studies Group for Osteoarthritis and Crystal Diseases. Under-representation of the elderly in osteoarthritis clinical trials. Rheumatology (Oxford) 2011;50(7):1184–6. [DOI] [PubMed] [Google Scholar]
- 74.Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am 1981;63(6):932–7. [PubMed] [Google Scholar]
- 75.Kujala UM, Orava S, Järvinen M. Hamstring injuries. Current trends in treatment and prevention. Sports Med 1997;23(6):397–404. [DOI] [PubMed] [Google Scholar]
- 76.Frank RM, Slabaugh MA, Grumet RC, Virkus WW, Bush-Joseph CA, Nho SJ. Posterior hip pain in the athletic population: Differential diagnosis and treatment options. Sports Health 2010;2(3):237–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med 2008;36(6):1110–5. 10.1177/0363546508314427 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the data and its Supporting Information files.