Abstract
Background. Drug overdose is an important, yet an inadequately understood, public health problem. Global attention to unintentional drug overdose has been limited by comparison with the scope of the problem. There has been a substantial increase in drug overdose incidence and prevalence in several countries worldwide over the past decade, contributing to both increased costs and mortality.
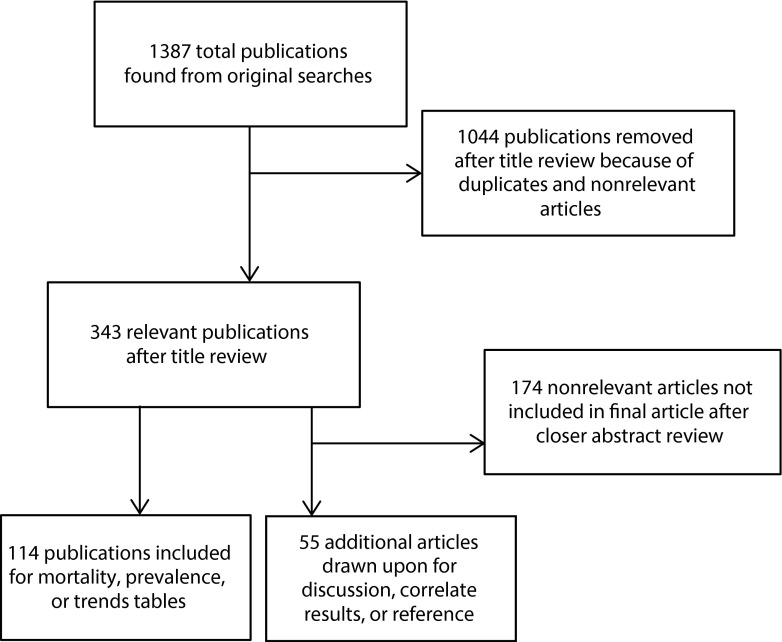
Objectives. The aim of this study was to systematically synthesize the peer-reviewed literature to document the global epidemiological profile of unintentional drug overdoses and the prevalence, time trends, mortality rates, and correlates of drug overdoses. We searched different combinations of Medical Subject Headings (MeSH) terms in PubMed for articles published from 1980 until July 2013, and we organized these results in tabular spreadsheets and compared them. We restricted the search to English-language articles that deal with unintentional overdose, focusing on 1 or more of the following key constructs: prevalence, time trends, mortality rates, and correlates. The term “overdose” as a MeSH major topic yielded 1076 publications. In addition, we searched the following combinations of nonmajor MeSH terms: “street drugs” and “overdose” yielded 180, “death” and “overdose” yielded 114, and “poisoning” and “drug users” yielded 17. There was some overlap among the searches. Based on the search and inclusion and exclusion criteria, we selected a total of 169 relevant articles for this article based on a close review of abstracts.
Results. We found wide variability in lifetime prevalence of experiencing a nonfatal overdose or witnessing an overdose, and in mortality rates attributable to overdose. Lifetime prevalence of witnessed overdose among drug users (n = 17 samples) ranged from 50% to 96%, with a mean of 73.3%, a median of 70%, and a standard deviation of 14.1%. Lifetime prevalence of drug users personally experiencing a nonfatal overdose (n = 27 samples), ranged from 16.6% to 68.0% with a mean of 45.4%, a median of 47%, and a standard deviation of 14.4%. Population-based crude overdose mortality rates (n = 28 samples) ranged from 0.04 to 46.6 per 100 000 person-years. This range is likely attributable to the diversity in regions, time periods, and samples. Most studies on longitudinal trends of overdose death rates or overdose-related hospitalization rates showed increases in overdose death rates and in overdose-related hospitalization rates across time, which have led to peaks in these rates at the present time. An overall trend of increasing deaths from prescription opioid use and decreasing deaths from illicit drug use in the past several years has been noted across most of the literature. With the increase in prescription opioid overdose deaths, drug overdose is not just an urban problem: rural areas have seen an important increase in overdose deaths. Lastly, cocaine, prescription opioids, and heroin are the drugs most commonly associated with unintentional drug overdoses worldwide and the demographic and psychiatric correlates associated with unintentional drug overdoses are similar globally.
Conclusions. There is a need to invest in research to understand the distinct determinants of prescription drug overdose worldwide. Several other countries need to collect in a systematic and continuous fashion such data on sales of prescription opioids and other prescription drugs, nonmedical use of prescription drugs, and hospitalization secondary to overdoses on prescription drugs. The sparse evidence on the environmental determinants of overdose suggests a need for research that will inform the types of environmental interventions we can use to prevent drug overdose. Methodological issues for future studies include enhancing data collection methods on unintentional fatal and nonfatal overdoses, and collecting more detailed information on drug use history, source of drug use (for prescription drugs), and demographic and psychiatric history characteristics of the individual who overdosed.
PLAIN-LANGUAGE Summary: Drug overdose is an important, yet inadequately understood, public health problem. The aim of this study was to systematically summarize the peer-reviewed literature to document the global epidemiological profile of unintentional drug overdoses, and the prevalence, time trends, mortality rates, and correlates of drug overdoses from 1980 until 2013. We found wide variability in prevalence mortality rates attributable to overdose. Most studies on longitudinal trends of overdose deaths or overdose-related hospitalizations showed increases across time. An overall trend of increasing deaths from prescription opioid use and decreasing deaths from illicit drug use in the past several years has been noted across most of the literature. With the increase in prescription opioid overdose deaths, drug overdose is not just an urban problem: rural areas have seen an important increase in overdose deaths. Lastly, cocaine, prescription opioids, and heroin are the drugs most commonly associated with unintentional drug overdoses worldwide and the demographic and psychiatric correlates associated with unintentional drug overdoses are similar globally. Future studies need to collect more detailed information on drug use history, source of drug use (for prescription drugs), and demographic and psychiatric history characteristics of the individual who overdosed.
Worldwide attention to unintentional drug overdose has been limited by comparison with the scope of the problem.1 There has been a substantial increase in drug overdose mortality in several countries worldwide over the past decade. The mortality rate from drug overdoses tripled in the United States between 1990 and 2006.2 In the United States, unintentional overdose deaths among adults aged 25 to 64 years exceeded motor vehicle crash deaths and suicides as a leading cause of injury death from 2008 onward.3 Likewise, unintentional overdose deaths outnumbered motor vehicle crash deaths in Australia in 2011.4 In Europe, rates have been stable since 2005, but most European countries also have high overdose rates. For example, overdose rates of more than 20 deaths per million are found in 14 of 30 European countries, and rates of more than 40 deaths per million in 7 countries.5
Until recently, drug overdoses were seen as a substance abuse or law enforcement issue and not as a public health problem.1 However, partly because of the increasing involvement of legal prescription drugs such as prescription opioids in drug overdoses, public health professionals have become more interested in the topic and in diminishing the societal burden posed by unintentional overdoses.1
Although drug overdose deaths attract much public attention,1,6–8 there are substantial consequences of nonfatal overdose, including cardiac and muscular problems, cognitive impairment, renal failure, hearing loss, and injuries sustained during overdose.9,10 Health care costs associated with overdose treatment are also substantial. From 1999 to 2008, hospitalization rates for overdoses in the United States increased by 55%, costing about $737 million in 2008.11 There are little data available on drug overdose hospitalization costs in countries other than the United States.
Drug overdose can be defined as happening when
someone . . . collapses, has blue skin, has convulsions, has difficulty breathing, loses consciousness, cannot be woken up, has a heart attack or dies while using drugs.12(p704)
This definition has been used widely across the literature.13–16 Unintentional drug overdoses are unique among causes of morbidity and mortality in 2 respects. First, unintentional overdose deaths are rarely instantaneous and drug users rarely overdose alone. As such, for the most part, overdose deaths are avoidable deaths. For example, those who witness an overdose episode can call for help and apply first aid measures.16 Opioid overdoses are preventable through the administration of naloxone, which can reverse the effect of opioids and can revive the individual.16–18 Second, drug overdoses are inevitably and inextricably linked to the surrounding environment, particularly in the centrality of drug availability as a necessary (but insufficient) determinant of overdose.19–23 Considering these observations that overdose is preventable and linked to surrounding environment, drug overdoses should be of concern to public health, both from the point of view of understanding their determinants and from the point of view of encouraging interventions to mitigate their consequences.
A systematic review of the drug overdose literature can help clarify what we know about unintentional drug overdoses and areas in which we have gaps in scholarship. Although reviews have been written about overdoses caused by particular types of drugs (e.g., prescription opioids, heroin, methadone),24–27 in certain places (e.g., Utah),28 on suicidal versus accidental overdose,29 or on overdoses among recently released prisoners,30 we are not aware of any global review of unintentional drug overdoses with the goal of synthesizing the prevalence, time trends, mortality rates, and correlates of drug overdose worldwide.
METHODS
The potential scope of literature that may be considered of interest to the topic is vast. We conducted a systematic review of publications available in the US National Library of Medicine’s PubMed electronic database31 in July 2013 by using different combinations of Medical Subject Headings (MeSH) search terms. We restricted the search to English-language articles published between 1980 and July 2013 that deal with unintentional overdose, focusing on 1 or more of the following key constructs: prevalence, time trends, mortality rates, and correlates. The term “overdose” as a MeSH Major Topic yielded 1076 publications. In addition, we searched the following combinations of nonmajor MeSH terms: “street drugs” and “overdose” yielded 180, “death” and “overdose” yielded 114, and “poisoning” and “drug users” yielded 17. There was some overlap among the searches. We did not use “unintentional” as a search term so as not to leave out studies that dealt with both intentional and accidental overdoses. There were no limitations in this original search on type of sample, or location or geography, but we excluded studies dealing with children, because, although this group is important, we aimed to focus only on studies that reported on unintentional drug overdoses among adults. We included commentaries because of their potential to shed light on potential interventions or trends. In addition, we reviewed reference lists of chosen articles to select additional studies or commentaries.
With these search and inclusion and exclusion criteria, we selected a total of 169 relevant articles for this study through a close review of abstracts (Figure 1). We were interested in articles that reported
population-based prevalence measures (46 articles; reported in Table 1),
studies that reported percentage of changes over time in trends of overdose (34 articles; Table 2),
mortality rates (53 articles; Table 3), and
correlates of overdose (summarized in the Results section, but not included in tables because of the lack of common quantitative measures to record these topics).
FIGURE 1—
Flowchart of selection of peer-reviewed articles to document the worldwide epidemiological profile of unintentional drug overdoses.
TABLE 1—
Studies Reporting the Prevalence of Unintentional Drug Overdose Worldwide, 1980–2013
| Reference | Type of Druga | Location and Time Period | Sample or Source | Type of Prevalence | Time Point | Prevalence, % |
| Coffin et al.15 | All substances | New York, NY, 2001–2004 | Street-recruited habitual drug usersb (n = 772) | Witnessed, both fatal and nonfatal | Lifetime | 68.5 |
| Experienced (nonfatal) | Lifetime | 16.6 | ||||
| Galea et al.32 | All substances | New York, NY, 2004–2005 | Overdose prevention and reversal program through a syringe exchange program—pilot study (n = 25) | Experienced (nonfatal) | Lifetime | 68.0 |
| Witnessed, both fatal and nonfatal | 83.0 | |||||
| Past 3 mo (of follow-up) | 50.0 | |||||
| Tobin et al.33 | All substances | Baltimore, MD, 2002–2003 | Self-Help in Eliminating Life-Threatening Diseases HIV-prevention studyc | Witnessed, both fatal and nonfatal | Lifetime | 70.0 |
| Werb et al.34 | All substances | Vancouver, BC, 2005–2006 | At-Risk Youth Study (n = 478) | Experienced (nonfatal) | Past 6 mo | 11.0 |
| Britton et al.35 | All substances (treatment sample) | 11 mid- to large urban areas in the United States | Drug Abuse Treatment Outcomes Studyd | Experienced (nonfatal) | Past year (after treatment) | 3.1 |
| Tracy et al.16; Bohnert et al.17 | Heroin, crack, and cocaine | Central Harlem and South Bronx, NY, 2001–2004 | Targeted street outreach of drug users aged ≥ 18 y (n = 1184) | Witnessed, both fatal and nonfatal | Lifetime | 67.3 |
| Witnessed, both fatal and nonfatal | Past 6 mo | 35.2 | ||||
| Among those who had ever witnessed (n = 672) | Experienced (nonfatal) | Lifetime | 45.0 | |||
| Bohnert et al.14 | Heroin, crack, and cocaine | Central Harlem and South Bronx, NY, 2001–2004 | Analytic sample = 1093 | Experienced (nonfatal) | Lifetime | 37.5 |
| Galea et al.36 | Heroin, crack, and cocaine | Central Harlem and South Bronx, NY, 2001–2004 | Among 928 persons who used cocaine during the past year | Experienced (nonfatal) | Past year | 17.0 |
| Heroin, crack, and cocaine | Among 1059 persons who used heroin during the past year | 16.8 | ||||
| Lagu et al.37 | Heroin and cocaine | Providence, RI, 2002–2004 | 329 study participantse | Witnessed, both fatal and nonfatal | Lifetime | 64.6 |
| Experienced (nonfatal) | 34.6 | |||||
| Brådvik et al.38 | Heroin | Malmö, Sweden, 2003 | 149 regular heroin users | Experienced (nonfatal) | Lifetime | 65.8 |
| Baca and Grant39 | Heroin | Albuquerque, NM, 2002 | Recruited from a syringe-exchange program: aged ≥ 18 y, used heroin in past 3 mo (n = 101) | Witnessed, both fatal and nonfatal | Lifetime | 94.1 |
| Experienced (nonfatal) | Lifetime | 64.4 | ||||
| Cullen et al.40 | Heroin | Dublin, Ireland, 1998–1999 | Questionnaire-based interview of drug users attending an inner city general practice (n = 24) | Witnessed, both fatal and nonfatal | Lifetime | 96.0 |
| Questionnaire-based interview | Witnessed fatal | 17.0 | ||||
| Questionnaire-based interview | Experienced (nonfatal) | 42.0 | ||||
| Darke et al.41 | Heroin | Sydney, Australia, 2001–2002 | ATOS cohort of 615 heroin usersf | Experienced (nonfatal) | Lifetime | 54.0 |
| Darke et al.42 | Heroin | Southwestern Sydney, Australia, 1995–1996 | 112 heroin users recruited through needle and syringe exchanges; had used heroin in preceding 24 hr | Experienced (nonfatal) | Lifetime | 53.0 |
| Past year | 16.4 | |||||
| Kerr et al.43; Kerr et al.44 | Heroin | Melbourne, Australia, 2007 | 99 injecting heroin users were recruited and interviewed at needle and syringe programs | Witnessed, both fatal and nonfatal | Lifetime | 84.0 |
| Experienced (nonfatal) | Lifetime | 61.0 | ||||
| Darke et al.9 | Heroin | New South Wales, Australia, 2001–2005 | Cohort study of 387 heroin users: ATOS | Experienced (nonfatal) | Lifetime (at baseline) | 55.0 |
| Past year (at baseline) | 26.6 | |||||
| Past 3 y (of follow-up) | 18.6 | |||||
| Darke et al.45 | Heroin | Sydney, Australia, 1994 | 329 heroin users | Witnessed, both fatal and nonfatal | Lifetime | 86.0 |
| Darke et al.46 | Heroin | Sydney, Australia, 1994 | 329 heroin users | Experienced (nonfatal) | Lifetime | 68.0 |
| Past year | 29.0 | |||||
| Gossop et al.47 | Heroin | South London, UK, 1992–1994 | Drug Transitions Project: 438 heroin users were contacted and interviewed by privileged-access interviewers | Experienced (nonfatal) | Lifetime | 23.0 |
| Past year | 9.4 | |||||
| Seal et al.48 | Heroin or “speedballs” (a cocaine and heroin mixture) | San Francisco, CA, 1998–1999 | 1427 heroin injectors were recruited from 6 inner-city neighborhoods (part of UHS) | Experienced (nonfatal) | Lifetime | 48.0 |
| Past year | 13.0 | |||||
| Taylor et al.49 | Injected heroin only | Glasgow, Scotland, 1993–1994 | 1018 recruited IDUs | Experienced (nonfatal) | Past year | 22.0 |
| Injected heroin + other drugs | 32.0 | |||||
| Methadone | 29.0 | |||||
| Buprenorphine | 26.0 | |||||
| Temazepam | 31.0 | |||||
| Cocaine | 37.0 | |||||
| Ecstasy | 38.0 | |||||
| Bluthenthal et al.50 | Injection drugs | San Francisco, CA, 1997 | UHS: 1114 street-recruited, active IDUs in 6 San Francisco Bay Area communities | Experienced (nonfatal) | Lifetime | 42.0 |
| UHS: 1114 street-recruited, active IDUs in 6 San Francisco Bay Area communities | Experienced (nonfatal) | Past year | 12.3 | |||
| Seal et al.51 | Injection drugs | San Francisco, CA, 2001 | UHS (n = 487): recruited from street settings in San Francisco and screened for enrollmentg | Experienced (nonfatal) | Past 6 mo (baseline) | 17.0 |
| San Francisco, CA, 2002 | Past 6 mo (follow-up) | 12.0 | ||||
| Jenkins et al.52 | Injection drugs (primarily heroin) | Seattle, WA, 2009 | Seattle and King Countyh (n = 447 clients) | Experienced (nonfatal) | Past year | 16.0 |
| Sherman et al.53 | Injection drugs | Baltimore, MD, 1999–2002 | Risk Evaluation and Assessment of Community Health IIIi (n = 309) | Witnessed, both fatal and nonfatal | Lifetime | 57.0 |
| Experienced (nonfatal) | 29.0 | |||||
| Pollini et al.54 | Injection drugs | Baltimore, MD, 2003–2004 | Cross-sectional survey administered to 924 IDUs in ongoing cohort study | Witnessed, both fatal and nonfatal | Lifetime | 69.7 |
| Wagner et al.55 | Injection drugs | Los Angeles, CA, 2006 | HRCj (n = 66) | Experienced (nonfatal) | Past 3 mo (at baseline) | 15.2 |
| Witnessed, both fatal and nonfatal | 48.5 | |||||
| Evans et al.56 | Injection drugs | San Francisco, CA, 1997 | UFO (“U Find Out”) Studyk (n = 644) | Experienced (nonfatal) | Lifetime | 39.1 |
| Experienced (nonfatal) | Past 3 mo (at baseline) | 11.9 | ||||
| Seal et al.57 | Injection drugs | San Francisco, CA, 1999–2000 | UHSl (n = 82) | Witnessed, both fatal and nonfatal | Lifetime | 89.0 |
| Davidson et al.58 | Injection drugs | San Francisco, CA, 1997–2000 | IDUs aged < 30 ym (n = 973) | Witnessed, both fatal and nonfatal | Lifetime | 73.0 |
| Past year | 50.0 | |||||
| Experienced (nonfatal) | Lifetime | 47.0 | ||||
| Past year | 26.8 | |||||
| Ochoa et al.13 | Injection drugs | San Francisco, CA, 1996 | Drug users aged 14–29 yn | Experienced (nonfatal) | Lifetime | 48.0 |
| Sergeev et al.59 | Injection drugs | Russian Federation, 2001 | Harm Reduction Training Projecto (n = 763) | Witnessed, both fatal and nonfatal | Lifetime | 81.0 |
| Witnessed fatal | 15.0 | |||||
| Experienced (nonfatal) | 59.0 | |||||
| Powis et al.60 | Injection drugs | London, UK, 1994–1995 | 312 current IDUsp | Witnessed, both fatal and nonfatal | Lifetime | 54.0 |
| Experienced (nonfatal) | 38.0 | |||||
| Fairbairn et al.19 | Injection drugs | Vancouver, BC, 2003–2005 | Vancouver Injection Drug Users Study (n = 551) | Experienced (nonfatal) | Past 6 mo (follow-up) | 6.7 |
| Kerr et al.61 | Injection drugs | Vancouver, BC, 1996–2004 | Vancouver Injection Drug Users Studyq (n = 1587) | Experienced (nonfatal) | Lifetime (at baseline) | 47.0 |
| Past 6 mo (follow-up) | 32.7 | |||||
| Bennett and Higgins62 | Injection drugs | Dorset, UK, 1995–1996 | Drug users who had injected in the 2 mo before interview (n = 212); multisource sampling | Experienced (nonfatal) | Past year | 30.0 |
| Witnessed, both fatal and nonfatal | 58.0 | |||||
| Bergenstorm et al.63 | Opioids | Bac Ninh and Tu Son, Vietnam, 2003 | 299 out-of-treatment male opioid IDUs aged 18–45 y; community-based cross-sectional survey | Experienced (nonfatal) | Lifetime | 43.5 |
| Past year | 36.1 | |||||
| Havens et al.64 | Prescription opioids, cocaine, heroin, and methamphetamine | Rural Appalachian Kentucky, year undisclosed | Social Networks Among Appalachian People Studyr (n = 400) | Witnessed, both fatal and nonfatal | Lifetime | 58.2 |
| Experienced (nonfatal) | 28.0 | |||||
| Fischer et al.65; Fischer et al.66 | Illicit opioids | Vancouver, BC, Edmonton, AB, Toronto, ON, Montréal, QC, and Québec, QC, 2002 | The Interdisciplinary Health Research Team on Illicit Opiate Addiction Research, Treatment, and Policys (n = 651) | Experienced (nonfatal) | Past 6 mo | 17.2 |
| Tobin et al.67 | Cocaine and opioids | Baltimore, MD, 2000 | 729 opioid and cocaine users completed a cross-sectional survey | Experienced (nonfatal) | Lifetime | 35.0 |
| Past year | 4.0 | |||||
| Man et al.68 | Opioids (methadone + diazepam) | Southern England, and Glasgow and Edinburgh, Scotland, 1999–2000 | Opioid users interviewed in 4 drug misuse treatment services (n = 135) | Experienced (nonfatal) | Lifetime | 56.0 |
| Silva et al.69 | Prescription opioids and tranquilizers | New York, NY, and Los Angeles, CA, 2009–2011 | 596 participants aged 16–25 yt | Experienced (nonfatal) | Lifetime | 23.6 |
| Kinner et al.70 | Illicit drugs | Vancouver, BC, 1996–2010 | Prospective cohort of 2515 community-recruited illicit drug users | Experienced (nonfatal) | Past 6 mo | 33.0 |
Note. ATOS = Australian Treatment Outcome Study; HRC = Homeless Health Care Los Angeles Center for Harm Reduction; IDUs = injection drug users; UHS = Urban Health Study.
All substances = opioid and nonopioid substances, both pharmaceutical and illicit, including alcohol.
Participants were users who had been injecting for at least 1 year, had injected heroin within the past 2 months, and were aged ≥ 18 years.
Snapshot of fourth wave (n = 568); recruited through street-based outreach, advertisements, and word of mouth; inclusion criteria were aged ≥ 18 years, having daily contact with drug users, and willingness to conduct HIV prevention outreach.
A longitudinal naturalistic multisite study; participants included 2966 patients with ≥ 1 substance abuse disorders.
Participants were recruited for a health service research study on drug users if they (1) were aged 18–70 years; (2) had injected heroin or cocaine during the preceding 30 days, or noninjection heroin or cocaine use at least weekly for the past 6 months; (3) had < 30 of the last 90 days spent in institutional settings including prisons and residential drug treatments or hospitalization; (4) spoke English; (5) denied intent to harm self or others; and (6) had absence of psychosis.
The cohort consisted of entrants to treatment of heroin dependence in opioid maintenance, detoxification, and residential rehabilitation; in addition, a group of heroin users not currently in treatment were recruited from needle and syringe programs in the regional health areas from which treatment entrants were recruited.
Eligible if they injected heroin > 2 times/wk, reported ≥ 1 heroin overdoses in the past 5 year, and could enroll together with an eligible injection partner who met the same criteria.
Sites included 2 indoor and 2 outdoor exchanges in Seattle, as well as a mobile exchange in suburban King County; n = 447 clients who reported opioid use since the beginning of the year (between January 2009 and the date the survey was administered in April or May of 2009).
Longitudinal study of 309 15- to 30-year-old IDUs and non-IDUs who had initiated heroin, cocaine, or crack use within 5 y before study enrollment.
IDUs, most of whom were homeless or in temporary housing, aged ≥ 18 y; participants were recruited via street outreach, distribution of advertising leaflets, and 1-on-1 recruitment within the HRC.
IDUs aged < 30 years, recruited by peer outreach workers with study invitation cards and flyers, contacts with youth-friendly neighborhood groups and community providers, and word of mouth; had to have self-reported use of injection drugs in the past 30 days.
Outreach and word of mouth using targeted sampling methods; eligibility determined by physical evidence of recent injection drug use (“tracks” or multiple venipuncture sites) or participation in previous cross-sections of data collection (final n = 82 who had experienced an overdose and wanted to participate, out of original 552).
IDUs aged < 30 years who had injected in the previous month in 4 neighborhoods of San Francisco; outreach and word of mouth.
Drug users aged 14–29 years who had injected drugs in the previous 6 months; study participants were recruited and interviewed at 6 needle exchanges and 3 youth outreach sites.
763 IDUs from 16 cities of the Russian Federation as part of the Harm Reduction Training Project.
312 current IDUs were recruited and interviewed in community settings by a team of privileged-access interviewers.
Persons were eligible if they had injected illicit drugs at least once in the previous month and resided in the greater Vancouver region.
Users aged ≥ 18 years, residing in an Appalachian county in Kentucky, and had used ≥ 1 of the following drugs to get high in the previous 30 days: prescription opioids, cocaine, heroin, or methamphetamine.
Participants were recruited by a variety of methods, including dissemination of flyers at user contact points such as needle exchanges, advertisements in community articles, and snowball sampling.
Interviewed a sample of 596 16- to 25-year-old patients in Los Angeles and New York who had engaged in misuse of a prescription drug (i.e., opioid, tranquilizer, stimulant, or any combination) ≥ 3 times in the past 90 days.
TABLE 2—
Studies Reporting Trends Across Time in Unintentional Overdose Worldwide, 1980–2013
| Reference | Type of Druga | Location and Time Period | Sample or Source | Measure | Trend or Change |
| CDC71 | All substances | United States, 1990–2001 | CDC, National Center for Injury Prevention and Control | Overdose death rate | 56% increase |
| 11 US states,b 1990–2001 | 145% average increase (range = 28%–325% [FL = 325%]) | ||||
| White et al.11 | All substances | United States, 1999–2008 | Nationwide inpatient samplec | Hospitalization rates | 55% increase |
| Paulozzi et al.72 | All substances | United States, 1990–2003 | National Center for Health Statistics: Whites | Drug-induced death rate | 189% increase |
| National Center for Health Statistics: African Americans | 64% increase | ||||
| Paulozzi et al.73 | All substances | United States, 1999–2004 | NVSS | Unintentional and undetermined drug poisoning mortality rates | 62.0% increase |
| NVSS, metropolitan counties only | 51.0% increase | ||||
| NVSS, nonmetropolitan counties only | 159% increase | ||||
| Degenhardt et al.74 | All substances | New South Wales, Australia, 2001 | Multipled | Drug-related deaths that appeared to be driven by the reduction in heroin supply | 43% decrease |
| Victoria, Australia, 2001 | 85% decrease | ||||
| Edwards et al.75 | All substances | Vermont, 2006–2009 | Medical Examiner’s Office | Drug-induced death rate | 27.4% increase |
| Vermont, 2009–2010 | 16.0% decrease | ||||
| Wunsch et al.76 | All substances | Western Virginia, 1997–2003 | Retrospective, population-based review of medical examiner cases | Deaths with a direct or contributing cause of drugs | 300% increase |
| Hammersley et al.77 | All substances | Glasgow, Scotland, 1991–1992 | The Department of Forensic Medicine and Science Laboratory | Drug-induced death rate | 400% increase |
| Shah et al.78; Mueller et al.79 | All substances | New Mexico, 1990–2005 | New Mexico Office of the Medical Investigator | Unintentional drug overdose death numbers and rates | 176.8% increase |
| Paulozzi et al.80 | All substances | United States, 1979–1990 | NCHS | Unintentional drug poisoning mortality rates | 5.3% increase (average per year) |
| United States, 1990–2002 | 18.1% increase (average per year); 217.6% total | ||||
| Opioid analgesics without heroin and cocaine | United States, 1999–2002 | Number of poisonings on death certificates | 129.2% increase | ||
| Heroin | 12.4% increase | ||||
| Cocaine | 22.8% increase | ||||
| Fingerhut et al.81 | All substances | United States, 1999–2005 | NVSS | Number of poisoning deaths | 65.6% increase |
| Methadone | 467.7% increase | ||||
| Heroin | 2.4% increase | ||||
| Other opioids | 110% increase | ||||
| Cocaine | 62.5% increase | ||||
| Cannabis | 202.7% increase | ||||
| CDC82 | All substances | Florida, 2003–2009 | Florida Medical Examiners Commission | Overdose death rate | 47.5% increase |
| Prescription drugs | 84.2% increase | ||||
| Illicit drugs | 21.4% decrease | ||||
| Madden and Shapiro83 | All substances | Vermont, 2001–2006 | Retrospective review of the Vermont Office of the Chief Medical Examiner | Overdose deaths | 400% increase |
| Methadone | Proportion of overall deaths that include methadone | 300% increase | |||
| Socie et al.84 | All substances | United States, 1996–2006 | CDC WISQARS Fatal Injury Reports” (WISQARS = Web-Based Injury Statistics Query and Reporting System) | Poisoning death rate | 74% increase |
| Ohio, 1996–2006 | 178% increase | ||||
| Ohio, 1999–2008 | 325% increase | ||||
| Wells et al.85 | All substances | England and Wales, 2007–2008 | National Statistics database | Drug poisoning deaths, men | 8% increase |
| Drug poisoning deaths, women | 17% increase | ||||
| Heroin and morphine | Drug poisoning deaths, women | 8% increase | |||
| Cocaine | Drug poisoning deaths, women | 20% increase | |||
| CDC6 | All substances | United States, 1999–2010 | CDC | Drug poisoning deaths, women | 151% increase |
| Drug poisoning deaths, men | 85% increase | ||||
| Opioids | Drug poisoning deaths, women | 500% increase | |||
| Wisniewksi et al.86 | Oxycodone | United States, 1995–2002 | Consolidated from the Drug Abuse Warning Network databasee | Emergency department visits | 560% increase |
| Morphine | 116% increase | ||||
| Hydrocodone | 160% increase | ||||
| Cerdà et al.2 | Prescription analgesics | New York, NY, 1990–2006 | Office of the Chief Medical Examiner of NYC | Overdose death rate | 700% increase |
| CDC87 | Methadone | United States, 1999–2009 | NVSS | Overdose death rate | 550% increase |
| Hawton et al.88 | Coproxamol | England and Wales, 1998–2010 | Office for National Statistics | Number of overdose deaths after withdrawal of coproxamol | 62% decrease (after intervention) |
| The DAWN Report89 | Prescription drugs | United States, 2004–2011 | Drug Abuse Warning Network database | Emergency department visits | 232.5% increase |
| Green et al.90 | Opioids | Connecticut, 1997–2007 | Connecticut Office of the Chief Medical Examiner | Absolute number of overdose deaths | 44% increase |
| Overdose deaths with toxicological data | 80% increase | ||||
| Methadone | Overdose deaths | 379% increase | |||
| Degenhardt et al.91 | Opiods | New South Wales, Australia, 1999–2001 | Australian Bureau of Statistics, et al.f | Opioid deaths | 60% decrease |
| 2000–2002 | Presentations of opioid overdose to emergency departments | 45% decrease | |||
| Calcaterra et al.92 | Pharmaceutical opioids | United States, 1999–2009 | CDC WONDER Database; 15- to 64-year-old patients | Age-adjusted death rate | 292.9% increase |
| Cochella et al.93; Johnson et al.94 | Prescription opioids | Utah, 2007–2008 | Interventiong | Medication-related overdose deaths following program implementation | 14.0% decrease (after intervention) |
| Scott et al.95 | Illicit opioids | Chicago, IL, 2000–2003 | Death certificatesh | Incidence of fatal overdose | 34% decrease |
| Marshall et al.96; Wood et al.97 | Injection drugs | Vancouver, BC, 2001–2005 | British Columbia Coroners Service | Overdose death rates after opening of first medically supervised safe-injection facility | 35% decrease (after intervention) |
| Friedman98 | Heroin and fentanyl | Illinois, 2006–2005 | Poison Control data | Heroin-related calls | 63.6% increase |
| Schwartz et al.99 | Heroin | Baltimore, MD, 1995–2002 vs 2003–2009 | Baltimore City Health Department | Average annual heroin overdose deaths (after buprenorphine became available) | 37% decrease |
| Maxwell et al.100 | Heroin | Chicago, IL, 1996–2000 | The Chicago Recovery Alliance, The Medical Examiner of Cook County | Opioid overdose deaths | 400% increase |
| Chicago, IL, 2000–2001 | After prevention program started providing naloxone | 20% decrease (after intervention) | |||
| Neeleman and Farrell101 | Heroin alone | England and Wales, 1974–1992 | Office of Population Censuses and Surveys tabulations | Lethal self-poisonings (including accidental, suicidal, and unknown) | 1186% increase |
| Methadone with or without heroin | Office of Population Censuses | 823% increase |
Note. CDC = Centers for Disease Control and Prevention; NCHS = National Center for Health Statistics; NVSS = National Vital Statistics System; NYC = New York City; WONDER = Wide-Ranging Online Data for Epidemiologic Research.
All substances = opioid and nonopioid substances, both pharmaceutical and illicit, including alcohol.
Colorado, Delaware, Kentucky, New Mexico, Florida, Massachusetts, North Carolina, Oregon, Washington, Utah, Wisconsin.
Designed to approximate a 20% sample of US community hospitals as defined by the American Hospital Association. Poisoning and nondependent abuse of alcohol and drugs in patients aged 18–24 years.
Hospital emergency departments, ambulance services, and coroner’s systems; treatment entries for heroin dependence compiled by state health departments; numbers of needles and syringes distributed to drug users; and data on arrests for heroin-related incidents and property-related crime incidents compiled by State Police Services.
Medical record and toxicology screening data from a nationally representative hospital sample.
Australian Bureau of Statistics and the Division of Analytical Laboratories, Institute of Clinical Pathology and Medical Research, Western Sydney Area Health Service, the Ambulance Service of New South Wales Case Sheet Database, and other emergency department data.
“Presentations highlighting six recommended prescribing practices were developed and presented to health care workers. Participants were encouraged to utilize the state prescription database and to complete a series of surveys assessing confidence and behavior changes at 0, 1, and 6 months post-presentation. Continuing medical education credits incentivized participation.”93(pS73)
Manually screened death certificates from the Illinois Department of Public Health master death files, 1999–2003, and the Chicago Real Time Death Surveillance System, 2003.
TABLE 3—
Studies Reporting Mortality Rates of Unintentional Drug Overdoses Worldwide, 1980–2013
| Reference | Type of Druga | Location and Time Period | Sample or Source | Mortality Rate per 100 000 Person-Years, Crude Unless Noted |
| Duncan102 | All substances | United States, 1981 | Division of Vital Statistics et al.b | 3.1 (age-adjusted) |
| United States, 1982 | 3.1 (age-adjusted) | |||
| United States, 1983 | 3.1 (age-adjusted) | |||
| United States, 1984 | 3.2 (age-adjusted) | |||
| United States, 1985 | 3.5 (age-adjusted) | |||
| United States, 1986 | 4.0 (age-adjusted) | |||
| United States, 1987 | 3.8 (age-adjusted) | |||
| United States, 1988 | 4.2 (age-adjusted) | |||
| United States, 1989 | 4.1 (age-adjusted) | |||
| United States, 1990 | 3.6 (age-adjusted) | |||
| United States, 1991 | 3.8 (age-adjusted) | |||
| CDC71 | All substances | United States, 2001 | CDC, National Center for Injury Prevention and Control | 7.8 |
| Paulozzi et al.73 | All substances | United States, 2004 | NVSS | 7.8 |
| Warner et al.103 | All substances | United States, 2008 | NVSS | 9.2 (age-adjusted) |
| CDC6 | All substances | United States, 2010 | CDC; female rate | 9.8 |
| Merrall et al.104 | All substances | Scotland, 1996–2000 | Scottish Drug Misuse Database cohortc | 498 (95% CI = 454, 545) |
| Scotland, 2001–2005 | 357 (95% CI = 334, 381) | |||
| Shah et al.78; Mueller et al.79 | All substances | New Mexico, 1990–2005 | New Mexico Office of the Medical Investigator | 10.4 (age-adjusted) |
| Shah et al.105 | All substances | New Mexico, 2005–2009 | New Mexico Office of the Medical Investigator | 17.6 (95% CI = 16.8, 18.5; age-adjusted) |
| Socie et al.84 | All substances | Ohio, 2008 | CDC WISQARS Fatal Injury Reports; Ohio Department of Vital Statistics | 13.7 |
| Wunsch et al.76 | All substances | Metropolitan Virginia, 1997–2003 | Office of the Medical Examinerd | 6.77 (95% CI = 6.12, 7.42) |
| Micropolitan Virginia, 1997–2003 | 7.68 (95% CI = 6.16, 9.20) | |||
| Rural Virginia, 1997–2003 | 10.76 (95% CI = 9.67, 11.85) | |||
| Farrell and Marsden106 | All substances | England and Wales, 1998–2003 | National sample of prisonerse: men | 520 (converted) |
| National sample of prisonerse: women | 590 (converted) | |||
| EMCDDA5 | All substances | European Union, 2010 | EMCDDA; population aged 15–64 y | 2 (converted) |
| Marshall et al.107 | Illicit drugs | British Columbia, 2001–2005 | British Columbia Coroners Servicef | 4.38 (95% CI = 4.10, 4.67) |
| Cocaine | 2.58 | |||
| Milloy et al.108 | Illicit drugs | British Columbia, 2001–2005 | British Columbia Coroners Service | 4.84 (age-adjusted) |
| Among those with First Nations identity | 13.3 (age-adjusted) | |||
| Harlow109 | Narcotics (heroin, morphine, dilaudid, etc.) | Texas, 1976–1987 | Medical examiner or death certificates filed with the Texas Department of Health | 0.13–0.92 |
| Cocaine | Texas, 1983–1987 | 0.04–0.09 | ||
| Galea et al.22; Coffin et al.110 | Cocaine, opioids, alcohol | New York, NY, 1990–1998 | Office of the Chief Medical Examiner of NYCg | 7.3–13.3 |
| Torralba et al.111 | Cocaine and opioids | Barcelona, Spain, 1989–1993 | City residents in the age group 15–49 y; used the Forensic Institute, and the Sistema d’Informacio de Drogues de Barcelona | 15.3 (95% CI = 14.1, 16.5; age- and sex-adjusted) |
| Marzuk et al.112 | Cocaine and opioids | New York, NY, 1990–1992 | Office of the Chief Medical Examiner of NYC and Census data | 1.27 (Upper East Side; age-adjusted); 38.76 (Central Harlem; age-adjusted) |
| Tardiff113 | Cocaine without opioids | New York, NY, 1990–1992 | Office of the Chief Medical Examiner of NYC and Census data | 2.86 |
| Opioids without cocaine | 2.29 | |||
| Cocaine and opioids | 3.42 | |||
| Cerdà et al.2 | Cocaine | New York, NY, 1993–1995 | Office of the Chief Medical Examiner of NYC | 15.5 (age-adjusted) |
| Heroin | 14.1 (age-adjusted) | |||
| Prescription analgesics | New York, NY, 2006 | 2.7 (age-adjusted) | ||
| Methadone | 4.4 (age-adjusted) | |||
| Stenbacka et al.114 | Illicit drugs | Stockholm, Sweden, 1967–2003 | Users with substance abuse problems (n = 1705)h | 277 (95% CI = 258, 295; converted; all-cause) |
| Evans et al.56 | Injection drugs | San Francisco, CA, 1997–2007 | UFO (“U Find Out”) Studyi | 912 (95% CI = 663, 1253; converted; all-cause) |
| Vlahov et al.115 | Injection drugs | 5 US cities,j 1997–2002 | Collaborative Injection Drug Users Studyj | 7.1 |
| Marshall et al.96 | Injection drugs | Vancouver, Canada, 2001–2003 | British Columbia Coroners Service | 253.8 (95% CI = 187.3, 320.3; standardized) |
| 2003–2005 | 165.1 (108.8, 221.4; standardized) | |||
| Hickman et al.116 | Injection drugs | Bristol, England, 2005–2006 | Respondent driven sampling and local Office for National Statistics mortality files; among drug users | 400 (converted) |
| Manfredi et al.117 | Injection drugs | Bologna, Northeastern Italy, 1977–2002 | Open cohort of 1214 IDUs, mostly heroin addicts, referring to a specialized outpatient center | 451.8 (converted) |
| Miller et al.118 | Injection drugs | Vancouver, BC, 1996–2004 | Vancouver Injection Drug User Studyk | 1368 (all-cause) |
| Wang et al.119 | Injection drugs | Baltimore, MD, 1988–2001 | ALIVE cohort study: 1927 actively IDUs HIV seronegative at baseline (308 later HIV seroconverted) | 1390 (converted) |
| ALIVE cohort study, but among seronegative drug users | 560 (converted) | |||
| Brettle et al.120 | Injection drugs | Edinburgh, Scotland, 1986–1994 | HIV-positive patients from the Edinburgh City Hospital cohort records | 1120 (converted) |
| Calcaterra et al.92 | Heroin | United States, 2007 | CDC WONDER Database; 15- to 64-year-old individuals | 1.05 (95% CI = 1.00, 1.09) |
| United States, 2009 | 1.43 (95% CI = 1.38, 1.48) | |||
| Darke et al.41 | Heroin | Sydney, Australia, 2001–2009 | Australian Treatment Outcome Study cohort of 615 heroin usersl | 643 (95% CI = 437, 913; converted) |
| Davidson et al.121 | Heroin | San Francisco, CA, 1997–2000 | Medical examiner’s case files, Census data | 14.29 |
| Ruttenber and Luke122 | Heroin | District of Columbia, 1981 | Deaths associated with injected street preparations of heroin (population-based) | 17.4 |
| Calcaterra et al.92 | Pharmaceutical opioids | United States, 1999 | CDC WONDER Database; 15- to 64-year-old patients | 1.54 (95% CI = 1.49, 1.60; age-adjusted) |
| United States, 2009 | 6.05 (95% CI = 5.95, 6.16; age-adjusted) | |||
| CDC7 | Opioid painkillers | Washington State, 2006 | CDC; health and human services agencies in WA | 6.4 |
| CDC; health and human services agencies in WA, but among only Medicaid-enrolled population | 30.8 (age-adjusted) | |||
| Fingerhut et al.81 | Methadone | United States, 2005 | NVSS | 1.5 |
| CDC87 | Methadone | United States, 2007 | NVSS | 1.8 |
| CDC123 | Methadone | United States, 2009 | NVSS | 1.5 |
| Soyka et al.124 | Methadone and buprenorphine | Munich, Germany | 2694 opioid-dependent patients in substitution treatment through the COBRA study | 1040 (converted; all-cause) |
| CDC82 | All substances | Florida, 2009 | Florida Medical Examiners Commission | 15.7 |
| Prescription drugs | 13.4 | |||
| Illicit drugs | 3.4 | |||
| Hall et al.125 | Prescription drugs | West Virginia, 2006 | Population-based, observational studym | 16.2 |
| Niveau et al.126 | Opioids | Geneva, Switzerland, 1999 | Cantonal Office of Statistics | 3.19 |
| Albert et al.127 | Opioids | Wilkes County, NC, 2009 | Before Project Lazarus | 46.6 |
| North Carolina, 2009 | 11.0 | |||
| Bird128 | Opioids | European Union,n 1990s | Combination of 6 European cohortsn | 870 (95% CI = 810, 940; converted) |
| Bargagli et al.129 | Opioids | Barcelona, Spain, 1990 | Cohorts recruited through EMCDDA protocol | 1296 (converted) |
| Denmark, 1990 | 707 (converted) | |||
| Dublin, Ireland, 1990 | 309 (converted) | |||
| Lisbon, Portugal, 1990 | 112 (converted) | |||
| London, England, 1990 | 737 (converted) | |||
| Rome, Italy, 1990 | 664 (converted) | |||
| Vienna, Austria, 1990 | 661 (converted) | |||
| Clausen et al.130 | Opioids | Norway, 1997–2003 | 3789 opioid-dependent userso | 2100 (converted) after treatment |
| Shah et al.131 | Opioids | England and Wales, 1993–1998 | Coroners’ files; men | 3.7 (converted) |
| Coroners’ files; women | 0.94 (converted) | |||
| Scott et al.95 | Illicit opioids | Chicago, IL, 2002p | Illinois master death files, 1999–2003, and Chicago Real Time Death Surveillance System 2003p | 33.0–35.0 |
| Morgan et al.132 | Antidepressants | England and Wales, 1993 | Coroners’ files | 0.9 (converted; age-adjusted) |
| England and Wales, 2002 | 0.7 (converted; age-adjusted) | |||
| Rocchi et al.133 | Illicit drugs | Italy, 1984–2000 | Direzione Centrale per i Servizi Antidroga of the Italian Ministry of the Interior; men aged 15–44 y | 6.6 (range = 1.6–11.3) avg per year |
| Direzione Centrale per i Servizi Antidroga of the Italian Ministry of the Interior; women aged 15–44 y | 0.7 (range = 0.3–1.1) avg per year | |||
| Fischer et al.134 | Fentanyl | Ontario, 2009 | Provincial coroners’ data (all standardized) | 0.44 |
| British Columbia, 2009 | 0.11 | |||
| Hydromorphone | Ontario, 2009 | 0.24 | ||
| British Columbia, 2009 | 0.45 | |||
| Morphine | Ontario, 2009 | 0.55 | ||
| British Columbia, 2009 | 2.94 | |||
| Oxycodone | Ontario, 2009 | 1.09 | ||
| British Columbia, 2009 | 0.70 |
Note. ALIVE = AIDS Linked to the Intravenous Experience; CDC = Centers for Disease Control and Prevention; CI = confidence interval; COBRA = Cost-Benefit and Risk Appraisal of Substitution Treatments study; EMCDDA = European Monitoring Centre for Drugs and Drug Addiction; IDU = injecting drug user; NVSS = National Vital Statistics System; NYC = New York City; WISQARS = Web-Based Injury Statistics Query and Reporting System; WONDER = Wide-Ranging Online Data for Epidemiologic Research.
All substances = opioid and nonopioid substances, both pharmaceutical and illicit, including alcohol.
Division of Vital Statistics of the US Public Health Service, death certificates, and Drug Enforcement Administration’s annual budget.
Scottish Drug Misuse Database cohort (treatment sample), matched with General Register Office for Scotland.
Retrospective, population-based review of medical examiner cases in the Office of the Medical Examiner.
National sample of 48 771 sentenced prisoners released during 1998–2000 with all recorded deaths included to November 2003.
All unnatural, unexpected, or unattended deaths in the province (n = 904).
All cases of fatal accidental drug overdose occurring in individuals aged 15–64 years.
Users were identified through records in Stockholm in 1967; these individuals were followed in registers recording mortality and cause of death and in patient care stays until 2003.
UFO (“U Find Out”) Study comprised 644 injection drug users aged < 30 y, recruited by peer outreach workers with study invitation cards and flyers, contacts with youth-friendly neighborhood groups and community providers, and word of mouth; had to have self-reported use of injection drugs in the past 30 days.
Collaborative Injection Drug Users Study comprised community-based, recent onset (< 5 y) injection drug users aged 18–35 years (n = 2089) from 5 US cities: Baltimore, MD; Chicago, IL; Los Angeles, CA; New Orleans, LA; and New York, NY.
Self-referral and street outreach from the Downtown Eastside, one of Vancouver’s poorest neighborhood: injection drug users aged 14–29 y (n = 572).
Australian Treatment Outcome Study cohort consists of entrants to treatment of heroin dependence in opioid maintenance, detoxification, and residential rehabilitation; in addition, a group of heroin users not currently in treatment were recruited from needle and syringe programs in the regional health areas from which treatment entrants were recruited.
Population-based (all state residents who died of unintentional pharmaceutical overdoses), observational study using data from medical examiner, prescription drug monitoring program, and opioid treatment program records.
Combination of 6 European cohorts who were recruited according to a common EMCDDA protocol from drug treatment agencies in Barcelona, Spain; Denmark; Dublin, Ireland; Lisbon, Portugal; Rome, Italy; and Vienna, Austria.
3789 opioid-dependent users who applied for and were accepted for opioid maintenance therapy (cross-linked with the Norwegian death register).
Manually screened death certificates from the Illinois Department of Public Health master death files, 1999–2003, and the Chicago Real Time Death Surveillance System 2003. These communities’ average poverty rate is 43%, 2 times that of the rest of the city.
RESULTS
Table 1 shows prevalence of overdose found in relevant articles, organized by type of drug, sample, and type of prevalence (witnessed vs experienced, fatal vs nonfatal, and time point). Lifetime prevalence of witnessed overdose among drug users (n = 17 samples from 18 articles) ranged from 50% to 96%,15–17,32,33,37,39,40,43–45,53,54,57–60,64 with a mean of 73.3%, a median of 70%, and a standard deviation of 14.1%. Although samples differed in demographics, length of drug use, and type of drug involved (e.g., prescription opioids, cocaine), the lifetime prevalence of witnessing an overdose did not differ greatly between studies conducted in different settings and countries.
Two studies reported lifetime prevalence of witnessing a fatal overdose specifically: 1 found that 4 of 24 drug users attending a general medical practice in inner-city Dublin, Ireland, in 1998 to 1999 had witnessed a fatal overdose40; the other reported a 15% prevalence among 763 injection drug users from 16 different cities of the Russian Federation.59 Two studies reported past-year prevalence of witnessed fatal or nonfatal overdose: 50% among 973 users aged younger than 30 years who had injected drugs in the previous month in 4 neighborhoods of San Francisco, California,58 and 58% of 212 users in Dorset, United Kingdom, who had injected in the previous 2 months.62 One study of drug users aged 18 years or older in New York City (n = 1184) reported past-6-month prevalence of witnessing overdose at 35.2%16 and 2 samples of injection drug users reported past-3-month prevalence of witnessing overdose at 48.5% and 50%.32,55
Lifetime prevalence of drug users personally experiencing a nonfatal overdose had a considerably wider range across studies (n = 29 samples), varying from 16.6% to 68.0%,9,13–16,32,37-44,46–48,50,53,56,58-61,63,64,67–69 with a mean of 45.4%, a median of 47%, and a standard deviation of 14.4%. Past-year prevalence of drug users personally experiencing a nonfatal overdose (n = 14 samples) ranged from 4.0% to 38.0%,9,35,36,42,46–50,52,58,62,63,67 with a mean of 18.8%, a median of 16.8%, and a standard deviation of 8.9%. Past-6-month prevalence of drug users personally experiencing a nonfatal overdose ranged from 6.7% to 33% (n = 7 samples),19,34,51,61,65,66,70 with a mean of 18.5%, a median of 17%, and a standard deviation of 10.4%. Two studies reported past-3-month prevalence of overdose: one found that 11.9% of drug users had overdosed out of 644 users younger than 30 years in San Francisco who had injected in the past 30 days56 and the other found a prevalence of 15.2% among injection drug users, most of whom were homeless or in temporary housing, in Los Angeles, California, in 2006.55
Trends
We reviewed articles for overall longitudinal trends of overdose death rates or overdose-related hospitalization rates (Table 2). Rates of increase for overdose deaths in population samples caused by any substance ranged from a 5.3% average increase per year in the United States from 1979 to 1990 to a 400% increase in both Glasgow, Scotland, between 1991 and 1992, and Vermont between 2001 and 2006.6,71–73,75–85
Between 1974 and 1992 in England and Wales, there was a 1186% increase in lethal self-poisonings from heroin alone.101 In the same location between 2007 and 2008, there was an 8% increase in heroin or morphine deaths among women, and a 20% increase in cocaine deaths among women.85 There was a 21.4% decrease in illicit drug overdose deaths in Florida between 2003 and 2009,82 and a 43% to 85% decrease among all drug-related deaths in Australia in 2001.74 In the Australian study, the reduction is believed to have been driven mainly by a reduction in heroin supply. A 34% decrease in illicit drug overdose deaths was seen in the city of Chicago, Illinois, from 2000 to 2003.95 One study reported a 55% increase in hospitalization rates for drug overdoses on all substances among a nationwide sample in the United States from 1999 to 2008.11
An overall trend of increasing deaths from prescription opioid use and decreasing deaths from illicit drug use in the past several years has been noted across most of the literature.80–82,89,90,96,97,99,100 With the exception of Australia, which experienced a 60% decrease in opioid deaths between 1990 and 2001,91 most studies in Table 2 reported increased rates of deaths from opioids.2,6,80–82,87,90,92,100 For example, there was a 467.7% increase reported in methadone deaths in the United States between 1999 and 2005,81 and a 129.2% increase in deaths from prescription opioids, between 1999 and 2002.80
Mortality Rates
Relevant studies that reported either population-based mortality rates attributable to fatal drug overdose, or all-cause and cause-specific death rates among drug users, are presented in Table 3, organized by type of drug, location and time period, and sample. Rates are crude and overdose-related, unless otherwise noted in the table. Rates are reported as number of deaths per 100 000 person-years; we converted original rates from articles that were presented on a different scale accordingly. Mortality rates differed widely depending on the setting and on the source population (i.e., any substance users, injection drug users only, recently released prisoners).
Population-based crude overdose mortality rates (n = 30 samples from 22 articles) ranged from 0.04 to 46.6 per 100 000 person-years.5,7,22,41,71,73,76,81,82,84,92,95,107,109–111,121–123,125–127 This range is likely attributable to the diversity in regions, time periods, and samples. The highest rates were generally seen in cities such as Barcelona, Spain,111 and Chicago among high-poverty communities,95 or in very rural areas such as West Virginia125 and Wilkes County, North Carolina,127 the latter of which was before an intervention. Population-based adjusted or standardized rates (n = 35 samples from 12 articles) ranged from 0.11 to 253.8,2,78,79,92,96,102,103,105,108,111,132,134 the highest rate being that of Vancouver, British Columbia, before the opening of the first medically supervised safe injection facility.96
Several studies reported on overdose mortality rates stratified by gender. Female-specific population-based overdose mortality rates reported included 9.8 in the United States, 0.94 in England and Wales, 0.7 in Italy, and 590 among recently released female prisoners.6,106,131,133 Male rates were 3.7 in England and Wales, 6.6 in Italy, and 520 among recently released male prisoners.106,131,133 Generally, death rates were higher among men than women, with the exception of recently released prisoners.
Among samples that included only drug users, overdose mortality rates were as high as 451.8,115–117 and all-cause mortality rates ranged from 277 to 1368.56,114,118 Among treatment-based samples, rates of drug-related deaths ranged from 309 to 2100.41,104,124,128–130 Among samples of HIV-positive individuals, overdose death rates were 1120 to 1390.119,120
Correlates
Type of drug.
Substances most commonly associated with overdose include cocaine, nonopioid analgesics (i.e., nonsteroidal antiinflammatory drugs), and opioids—a class of drug that includes heroin, as well as prescription opioids such as morphine, methadone, codeine, and oxycodone. Some findings on how class of drug used affects overdose outcome are highlighted here.
Cocaine was one of the major drivers of overdose in the 1990s and early 2000s, especially in urban areas such as New York City.22,23 In a study of witnessed overdoses in New York City in the early 2000s, powdered cocaine use predicted fatality among respondents’ reported last witnessed overdose.17 However, a shift toward opioids has occurred worldwide throughout the past several years.135
In a study of fatal overdoses in Connecticut, 77% of accidental overdose deaths from 1997 to 2007 involved opioids.90 Opioid deaths were also more likely to involve alcohol and benzodiazepines.2,85,90 Several articles focused on fentanyl, an opioid receptor agonist that is used as a filler for street heroin (or laced into heroin and cocaine) and has been more frequently prescribed in recent years.136,137 Fentanyl is estimated to be 80 times more potent than morphine, so a small change in dosage may be fatal. Compounding this issue, many narcotic drug screens do not routinely screen for fentanyl.138 Only 1 of the studies that included prescription medications69 differentiated between those who experienced overdoses secondary to nonmedical use (i.e., using in larger amounts than prescribed or not prescribed for them) and had been prescribed these drugs versus those who experienced overdoses but had never been prescribed these drugs. Of the 596 respondents included in this study, 72.8% had already been prescribed in their lifetime prescription opioids, 45.5% had already been prescribed prescription tranquilizers, and 45.1% had already been prescribed prescription stimulants. None of the mortality articles included in our review had information on whether those who died because of overdoses secondary to prescription drug use had been using these drugs for therapeutic purposes.
Whether drugs are taken in pure form on their own or combination form (including mixed with alcohol) is important.16,77 “Polydrug” use is associated with a much higher risk of death from overdose; a study of opioid overdoses presenting to an emergency department in Switzerland found that up to 90% of patients tested positive for multiple drugs.139 According to the New York City Department of Health and Mental Hygiene, about 98% of overdose deaths that occur in the city involve more than 1 substance.140 In addition, a review of Australian national coroner’s records from 2000 to 2007 found that 72% of drug-related deaths in released prisoners involved polydrug use.141
For studies based on interviews about personal overdose experiences or witnessed overdoses, we cannot know with certainty exactly what type of drug or how many the person overdosed on, but rely on participant responses (e.g., Tracy et al.16). These types of studies also often have inclusion criteria such as had to have injected heroin within the past 2 months15 or had to have injected heroin or cocaine during the preceding 30 days,37 which give us some indication of what drug was likely used, but it is not always specified. Some were treatment samples of specific types of drug users41,43 in which we generally assume for simplicity that if they were heroin injectors, they overdosed on heroin. Some studies do specify “heroin only,” for example, or differentiate between “heroin only” and “heroin and other drugs,”49 though, again, these are often based on self-report. Others still differentiate between single drugs and combination, but are based on autopsy findings or a mix of autopsy findings and circumstances of the fatality that we can be a little more sure about.113 Most of the larger countrywide studies on mortality or trends look at overall deaths or hospitalizations, not distinguishing between type of drug (e.g., White et al.11).
Setting or regional differences.
Drug overdose is not just an urban problem, even though historically more emphasis has been placed on urban areas.142–144 In recent years, rural areas have seen rapid increases in rates of nonmedical prescription drug use and overdose: in rural Virginia between 1997 and 2003, fatalities attributed to overdose increased by 300% (prescription opioids and benzodiazepines were more prevalent than illicit drugs).76 In Utah, prescription opioid deaths increased fivefold during 2000 to 2009.28 Furthermore, prescription drug overdose is now the leading cause of injury death in Ohio, with particularly high rates in the rural Appalachian areas of the state.84
In addition, the setting and circumstances of a drug overdose can tell us a lot about potential outcomes. In a study of fatal overdose in New York City in 1996, deaths were more likely to occur in neighborhoods in the top decile of income inequality than in more equitable neighborhoods.145 This relationship was partially explained by the level of disorder in the environment and the quality of the built environment. When compared with nonoverdose but unintentional deaths, prescription opioid overdose deaths from another study in New York City were more likely to occur in lower-income and “fragmented” neighborhoods, but when compared with heroin fatalities, they were more likely to occur in higher-income and less-fragmented neighborhoods.146 One explanation for this is that higher-income neighborhoods offer a larger supply of prescription opioids through pharmacies and physicians that is not present in more disadvantaged, primarily minority neighborhoods. A study in 10 Spanish cities from 1996 to 2003 found that male overdose deaths were more common in cities with high levels of socioeconomic inequality.147
The physical settings in which users inject also matter. A Vancouver study estimated that users who injected in public places (vs those who injected in private settings) were 4.7 times more likely to experience a nonfatal overdose.19 A study by Bohnert et al. on policing and risk of overdose in New York City found that fatal overdoses were more likely to occur in secluded public places, such as abandoned buildings.20 This is likely attributable to the fact that it is more difficult to find help when someone overdoses, and may be a result of fear of heavy policing in urban areas. Another study that investigated risks of heroin overdose noted injection in an “unusual place” (defined by each individual according to his or her injecting habits) as a risk factor for overdoses.21 One explanation presented for this phenomenon is that tolerance is based on Pavlovian conditioning of cues, and when a user of typically high tolerance injects in an unusual circumstance, they lack the cues that they usually associate with a drug’s effect, causing their tolerance to fail.148
Characteristics of the user.
Lastly, characteristics of the drug user are important to consider as correlates for drug overdose. One characteristic of note is gender. Men are more likely to self-report nonmedical use of prescription drugs, yet more women are more often prescribed drugs prone to abuse.149,150 This might be because of the fact that many common forms of pain such as osteoarthritis, fibromyalgia, lower-back pain, and shoulder pain are more prevalent among women, and women also report higher intensity of pain from these conditions.151,152 The US Centers for Disease Control and Prevention reported that the proportion of drug overdose deaths caused by prescription opioids was highest among women aged 45 to 54 years and among American Indian or Alaska Natives and non-Hispanic White women.153 A study in Australia showed a 70-to-30 male-to-female ratio of nonfatal heroin overdose.142
Another commonly studied correlate is race/ethnicity. A review of coroner case files from British Columbia from 2001 to 2005 found that First Nations individuals had higher rates of mortality from overdose.108 An investigation of fatal accidental drug overdose in New York City between 1990 and 1998 found that overdose deaths were consistently higher among non-Hispanic Blacks and Hispanics compared with non-Hispanic Whites. In addition, cocaine was more common among non-Hispanic Black decedents, whereas opioids and alcohol were more common among Hispanic and non-Hispanic White decedents.22 On the other hand, rates of prescription opioid deaths are higher among non-Hispanic Whites than among respondents of other races/ethnicities.153
Other factors associated with increased risk of nonfatal overdose found in the literature review included belonging to a lower income group while growing up, not graduating high school, being a smoker, having ever received care at a psychiatric facility, ever witnessing a family member overdose, being prescribed tranquilizers, having cocaine dependence, and injecting in the past 90 days.28,36,69,154
Certain subgroups of the population are especially prone to overdose risk, including homeless individuals, HIV-positive individuals, and recently released prisoners.65,120,155,156 Individuals who have recently attended substance abuse treatment or been released from incarceration are at increased risk of overdose, often because they have lost tolerance for their usual doses.26,157 Overdose is also significantly associated with psychiatric disorders, suicidal ideation, and attempted suicide.67,158 Lastly, duration of drug use and reports of previous overdose episodes are associated with overdose.159,160
DISCUSSION
We systematically synthesized the peer-reviewed literature to document the global epidemiological profile of unintentional drug overdoses, and the prevalence, time trends, mortality rates, and correlates of drug overdoses. We found, first, wide variability in the lifetime prevalence of experiencing a nonfatal overdose and in mortality rates attributable to overdoses, depending on the study setting. Second, the majority of studies on longitudinal trends of overdose death rates or overdose-related hospitalization rates showed increases in overdose death rates and in overdose-related hospitalization rates across time, which have led to peaks in these rates now. In particular, an overall trend of increasing deaths from prescription opioid use and decreasing deaths from illicit drug use in the past several years has been noted across most of the literature.80–82,89,90,96,97,99,100 Third, with the increase in prescription opioid overdose deaths, drug overdose is no longer just an urban problem: rural areas have seen an important increase in overdose deaths. Fourth, cocaine, prescription opioids, and heroin are the drugs most commonly associated with unintentional drug overdoses worldwide and the demographic and psychiatric correlates associated with unintentional drug overdoses are similar worldwide. However, more studies examining these correlates are needed from non–English-speaking countries.
Drug overdose is an important, yet inadequately understood, public health problem. A review of existing studies points to several key methodological issues that future studies need to address and limitations in extant studies. Methodological issues include enhancing data collection methods on unintentional fatal and nonfatal overdoses, and collecting more detailed information on drug use history, source of drug use (for prescription drugs), and demographic and psychiatric history characteristics of the individual who overdosed. For example, future studies could employ consistency check strategies to compare medical examiner information on fatal overdoses with available medical records and information from the deceased individuals’ family members.
Future data collection efforts could also include more detailed questions when interviewing individuals who report nonfatal overdoses, and check consistency of such information with hospital discharge data and information from family or other third parties (e.g., friends who witnessed the overdose episode). The field still also lacks studies in rural areas as well as longitudinal studies of population-based drug users (i.e., non–treatment samples) in multiple urban and rural areas that would provide us with comparable prevalence estimates across different contexts.
In addition, several of the selected studies did not disclose how they defined nonfatal overdoses to study respondents,33,34,37 simply mentioning that they asked them if they had ever experienced or witnessed an overdose, which could be somewhat misleading and biased. On the other hand, it should be noted that, among the studies that provided information on the definition of nonfatal overdoses, the definition of nonfatal overdoses was overall extremely consistent and standardized across the reviewed studies, similar to the definition we present in the introduction of this review.12,14–17,36,39,40
The marked increase in prescription opioid overdoses described in the studies reviewed is likely attributable to a rapid increase in sales of prescription opioids during the past decade; the quantity of prescription opioids sold to pharmacies, hospitals, and doctors’ offices in the United States was 4 times larger in 2010 than in 1999.8 The increase in overdoses caused by prescription opioid use in the United States parallels the increase in the availability of prescription opioids since the early to mid-1990s in the United States.90 As described in one of Nora Volkow’s recent presentations to the US Senate:
The number of prescriptions for opioids (like hydrocodone and oxycodone products) have escalated from around 76 million in 1991 to nearly 207 million in 2013, with the United States their biggest consumer globally, accounting for almost 100 percent of the world total for hydrocodone (i.e., Vicodin) and 81 percent for oxycodone (i.e., Percocet).161(p3)
There is a need to invest in research to understand the distinct determinants of this type of overdose worldwide. Several other countries need to collect in a systematic and continuous fashion such data on sales of prescription opioids and other prescription drugs, nonmedical use of prescription drugs, and hospitalization secondary to overdoses on prescription drugs. Moreover, there is the need for future studies to further investigate whether those who overdose while using prescription medication had been prescribed these drugs recently or in the past because only 1 of the reviewed studies included this information.69
Finally, the sparse evidence on the environmental determinants of overdose suggest a need for research that will inform the types of environmental interventions we can use to prevent drug overdose. A combination of studies on individuals who overdose and the settings where overdoses occur will help us better tailor interventions to the types of strategies that are most likely to have a major impact on this epidemic.
Limitations of the reviewed studies are also noted. First, most studies did not collect information on the sources of drug used, which can provide insights into the ways individuals learn about and acquire drugs, and can thus inform prevention opportunities. Drugs can be acquired from family, friends, and drug dealers, but they can also be prescribed for legitimate medical reasons (in the case of prescription drugs). More studies that investigate prescribing patterns, such as the article by Logan et al. on potentially inappropriate prescriptions given in the emergency department,162 are needed. Moreover, only about a third of the mortality rate studies, half of trends studies, and one sixth of the prevalence studies stratify results by specific types of prescription drugs.
Second, it is already well established that there might be an underreporting of intentional overdoses, because when substance users are asked whether their overdose was or was not intentional, most report it as unintentional.29,163,164 In our review, we focused on unintentional overdoses, but there is the possibility that some of these overdoses were truly intentional.
Third, because substance users who experience an overdose are usually polydrug users, it is very difficult to distinguish which and how many drugs were used before an overdose episode.165–168 Because of the high prevalence of multiple drugs being present in overdoses,11,139 it is hard to tease out the effect of one drug over another. Overall, there is a mix of how well studies differentiate, but many aim to show an overall measure of burden of this issue, not truly trying to make a causal association with any 1 type of drug.
Fourth, studies have shown that forensic toxicology laboratories are limited in the number of drugs for which they can screen and that drug levels can change postmortem.165–168 Further complicating this issue is the fact that data collected by medical examiners and coroners are usually inadequate, incomplete, and inconsistent with regard to polydrug use, estimated drug dosage (when, for instance, the individual had a legitimate prescription for at least 1 of the drugs involved in the fatal overdose episode—e.g., a legitimate opioid prescription), and patient characteristics.169
Fifth, if we are to identify potential avenues to prevent drug overdose, more concerted investment needs to be made to understand the environmental drivers of overdose risk, and the individual and interpersonal mechanisms whereby environmental characteristics can increase the risk for overdose. This is particularly important for overdose risk in rural areas, as the bulk of the literature on environmental determinants of overdose has focused on urban areas. This also has important implications for prevention and intervention strategies that need to focus on harm reduction strategies such as the availability of safe injection facilities or mobile safe injection facilities where individuals can inject preobtained drugs under the supervision of a medical doctor, such as facilities that exist in Canada and in some European countries,19 while also offering them treatment for their drug-using behavior.
Acknowledgments
M. Cerdá was supported by US National Institute on Drug Abuse grant DA030449. S. S. Martins was supported by US National Institute of Child and Human Development grant HD060072 and by US National Institute on Drug Abuse grant DA 037866. S. Galea was supported by US Health and Human Services grant HITEP130003-01-00, Department of Defense grant W81XWH-07-1-0409, and grant funding from the Rockefeller Foundation. L. Sampson was supported by the Department of Defense grant W81XWH-07-1-0409.
S. S. Martins was a consultant for Purdue Pharma until December 2014 to collaborate on a manuscript on secondary analyses of National Epidemiologic Survey on Alcohol and Related Conditions data on prescription opioid dependence.
Human Participant Protection
The article is a review of already published articles and considered non–human participant research by Columbia University’s institutional review board.
References
- 1.Paulozzi LJ. Overdoses are injuries too. Inj Prev. 2007;13(5):293–294. doi: 10.1136/ip.2007.016113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cerdá M, Ransome Y, Keyes KM et al. Prescription opioid mortality trends in New York City, 1990–2006: examining the emergence of an epidemic. Drug Alcohol Depend. 2013;132(1-2):53–62. doi: 10.1016/j.drugalcdep.2012.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Wide-Ranging Online Data for Epidemiologic Research (WONDER) 2010. Available at: http://wonder.cdc.gov. Accessed September 27, 2011.
- 4.International Overdose Awareness Day. Overdose: worse than the road toll. Available at: http://www.overdoseday.com/wp-content/uploads/2013/07/Factsheet-Greater-than-the-Road-Toll-KE-FINAL-15-August-2013.pdf. Accessed August 14, 2015.
- 5.Lisbon, Portugal: European Monitoring Centre for Drugs and Drug Addiction; 2012. 2012 annual report on the state of the drugs problem in Europe. [Google Scholar]
- 6.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers and other drugs among women—United States, 1999–2010. MMWR Morbid Mortal Wkly Rep. 2013;62(26):537–542. [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Overdose deaths involving prescription opioids among Medicaid enrollees—Washington, 2004–2007. MMWR Morb Mortal Wkly Rep. 2009;58(42):1171–1175. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 9.Darke S, Williamson A, Ross J, Mills KL, Havard A, Teesson M. Patterns of nonfatal heroin overdose over a 3-year period: findings from the Australian treatment outcome study. J Urban Health. 2007;84(2):283–291. doi: 10.1007/s11524-006-9156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schweitzer VG, Darrat I, Stach BA, Gray E. Sudden bilateral sensorineural hearing loss following polysubstance narcotic overdose. J Am Acad Audiol. 2011;22(4):208–214. doi: 10.3766/jaaa.22.4.3. [DOI] [PubMed] [Google Scholar]
- 11.White AM, Hingson RW, Pan IJ, Yi HY. Hospitalizations for alcohol and drug overdoses in young adults ages 18–24 in the United States, 1999–2008: results from the Nationwide Inpatient Sample. J Stud Alcohol Drugs. 2011;72(5):774–786. doi: 10.15288/jsad.2011.72.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGregor C, Darke S, Ali R, Christie P. Experience of non-fatal overdose among heroin users in Adelaide, Australia: circumstances and risk perceptions. Addiction. 1998;93(5):701–711. doi: 10.1046/j.1360-0443.1998.9357016.x. [DOI] [PubMed] [Google Scholar]
- 13.Ochoa KC, Hahn JA, Seal KH, Moss AR. Overdosing among young injection drug users in San Francisco. Addict Behav. 2001;26(3):453–460. doi: 10.1016/s0306-4603(00)00115-5. [DOI] [PubMed] [Google Scholar]
- 14.Bohnert AS, Tracy M, Galea S. Characteristics of drug users who witness many overdoses: implications for overdose prevention. Drug Alcohol Depend. 2012;120(1-3):168–173. doi: 10.1016/j.drugalcdep.2011.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coffin PO, Tracy M, Bucciarelli A, Ompad D, Vlahov D, Galea S. Identifying injection drug users at risk of nonfatal overdose. Acad Emerg Med. 2007;14(7):616–623. doi: 10.1197/j.aem.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Tracy M, Piper TM, Ompad D et al. Circumstances of witnessed drug overdose in New York City: implications for intervention. Drug Alcohol Depend. 2005;79(2):181–190. doi: 10.1016/j.drugalcdep.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 17.Bohnert AS, Tracy M, Galea S. Circumstances and witness characteristics associated with overdose fatality. Ann Emerg Med. 2009;54(4):618–624. doi: 10.1016/j.annemergmed.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Community-based opioid overdose prevention programs providing naloxone—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(6):101–105. [PMC free article] [PubMed] [Google Scholar]
- 19.Fairbairn N, Wood E, Stoltz JA, Li K, Montaner J, Kerr T. Crystal methamphetamine use associated with non-fatal overdose among a cohort of injection drug users in Vancouver. Public Health. 2008;122(1):70–78. doi: 10.1016/j.puhe.2007.02.016. [DOI] [PubMed] [Google Scholar]
- 20.Bohnert AS, Nandi A, Tracy M et al. Policing and risk of overdose mortality in urban neighborhoods. Drug Alcohol Depend. 2011;113(1):62–68. doi: 10.1016/j.drugalcdep.2010.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gutiérrez-Cebollada J, de la Torre R, Ortuño J, Garcés J, Camí J. Psychotropic drug consumption and other factors associated with heroin overdose. Drug Alcohol Depend. 1994;35(2):169–174. doi: 10.1016/0376-8716(94)90124-4. [DOI] [PubMed] [Google Scholar]
- 22.Galea S, Ahern J, Tardiff K et al. Racial/ethnic disparities in overdose mortality trends in New York City, 1990–1998. J Urban Health. 2003;80(2):201–211. doi: 10.1093/jurban/jtg023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zimmerman JL. Cocaine intoxication. Crit Care Clin. 2012;28(4):517–526. doi: 10.1016/j.ccc.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Vormfelde SV, Poser W. Death attributed to methadone. Pharmacopsychiatry. 2001;34(6):217–222. doi: 10.1055/s-2001-18032. [DOI] [PubMed] [Google Scholar]
- 25.Degenhardt L, Bucello C, Mathers B et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and meta-analysis of cohort studies. Addiction. 2011;106(1):32–51. doi: 10.1111/j.1360-0443.2010.03140.x. [DOI] [PubMed] [Google Scholar]
- 26.Paulozzi LJ. Prescription drug overdoses: a review. J Safety Res. 2012;43(4):283–289. doi: 10.1016/j.jsr.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull World Health Organ. 2013;91(2):102–123. doi: 10.2471/BLT.12.108282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lanier WA, Johnson EM, Rolfs RT, Friedrichs MD, Grey TC. Risk factors for prescription opioid-related death, Utah, 2008–2009. Pain Med. 2012;13(12):1580–1589. doi: 10.1111/j.1526-4637.2012.01518.x. [DOI] [PubMed] [Google Scholar]
- 29.Bohnert AS, Roeder K, Ilgen MA. Unintentional overdose and suicide among substance users: a review of overlap and risk factors. Drug Alcohol Depend. 2010;110(3):183–192. doi: 10.1016/j.drugalcdep.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 30.Merrall EL, Kariminia A, Binswanger IA et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105(9):1545–1554. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. PubMed. Bethesda, MD: US National Library of Medicine, National Institutes of Health.
- 32.Galea S, Worthington N, Piper TM, Nandi VV, Curtis M, Rosenthal DM. Provision of naloxone to injection drug users as an overdose prevention strategy: early evidence from a pilot study in New York City. Addict Behav. 2006;31(5):907–912. doi: 10.1016/j.addbeh.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 33.Tobin KE, Davey MA, Latkin CA. Calling emergency medical services during drug overdose: an examination of individual, social and setting correlates. Addiction. 2005;100(3):397–404. doi: 10.1111/j.1360-0443.2005.00975.x. [DOI] [PubMed] [Google Scholar]
- 34.Werb D, Kerr T, Lai C, Montaner J, Wood E. Nonfatal overdose among a cohort of street-involved youth. J Adolesc Health. 2008;42(3):303–306. doi: 10.1016/j.jadohealth.2007.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Britton PC, Wines JD, II, Conner KR. Non-fatal overdose in the 12 months following treatment for substance use disorders. Drug Alcohol Depend. 2010;107(1):51–55. doi: 10.1016/j.drugalcdep.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Galea S, Nandi A, Coffin PO et al. Heroin and cocaine dependence and the risk of accidental non-fatal drug overdose. J Addict Dis. 2006;25(3):79–87. doi: 10.1300/J069v25n03_10. [DOI] [PubMed] [Google Scholar]
- 37.Lagu T, Anderson BJ, Stein M. Overdoses among friends: drug users are willing to administer naloxone to others. J Subst Abuse Treat. 2006;30(2):129–133. doi: 10.1016/j.jsat.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 38.Brådvik L, Frank A, Hulenvik P, Medvedeo A, Berglund M. Heroin addicts reporting previous heroin overdoses also report suicide attempts. Suicide Life Threat Behav. 2007;37(4):475–481. doi: 10.1521/suli.2007.37.4.475. [DOI] [PubMed] [Google Scholar]
- 39.Baca CT, Grant KJ. What heroin users tell us about overdose. J Addict Dis. 2007;26(4):63–68. doi: 10.1300/J069v26n04_08. [DOI] [PubMed] [Google Scholar]
- 40.Cullen W, Bury G, Langton D. Experience of heroin overdose among drug users attending general practice. Br J Gen Pract. 2000;50(456):546–549. [PMC free article] [PubMed] [Google Scholar]
- 41.Darke S, Mills KL, Ross J, Teesson M. Rates and correlates of mortality amongst heroin users: findings from the Australian Treatment Outcome Study (ATOS), 2001–2009. Drug Alcohol Depend. 2011;115(3):190–195. doi: 10.1016/j.drugalcdep.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 42.Darke S, Sunjic S, Zador D, Prolov T. A comparison of blood toxicology of heroin-related deaths and current heroin users in Sydney, Australia. Drug Alcohol Depend. 1997;47(1):45–53. doi: 10.1016/s0376-8716(97)00070-7. [DOI] [PubMed] [Google Scholar]
- 43.Kerr D, Dietze P, Kelly AM, Jolley D. Improved response by peers after witnessed heroin overdose in Melbourne. Drug Alcohol Rev. 2009;28(3):327–330. doi: 10.1111/j.1465-3362.2009.00029.x. [DOI] [PubMed] [Google Scholar]
- 44.Kerr D, Dietze P, Kelly AM, Jolley D. Attitudes of Australian heroin users to peer distribution of naloxone for heroin overdose: perspectives on intranasal administration. J Urban Health. 2008;85(3):352–360. doi: 10.1007/s11524-008-9273-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia: II. responses to overdose. Addiction. 1996;91(3):413–417. doi: 10.1046/j.1360-0443.1996.91341310.x. [DOI] [PubMed] [Google Scholar]
- 46.Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia: I. Prevalence and correlates of non-fatal overdose. Addiction. 1996;91(3):405–411. [PubMed] [Google Scholar]
- 47.Gossop M, Griffiths P, Powis B, Williamson S, Strang J. Frequency of non-fatal heroin overdose: survey of heroin users recruited in non-clinical settings. BMJ. 1996;313(7054):402. doi: 10.1136/bmj.313.7054.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seal KH, Kral AH, Gee L et al. Predictors and prevention of nonfatal overdose among street-recruited injection heroin users in the San Francisco Bay Area, 1998–1999. Am J Public Health. 2001;91(11):1842–1846. doi: 10.2105/ajph.91.11.1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Taylor A, Frischer M, Goldberg D. Non-fatal overdosing is related to polydrug use in Glasgow. BMJ. 1996;313(7069):1400–1401. doi: 10.1136/bmj.313.7069.1400b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bluthenthal RN, Kral AH, Lorvick J, Erringer EA, Edlin BR. Harm reduction and needle exchange programmes. Lancet. 1998;351(9118):1819–1820. doi: 10.1016/S0140-6736(05)78791-2. [DOI] [PubMed] [Google Scholar]
- 51.Seal KH, Thawley R, Gee L et al. Naloxone distribution and cardiopulmonary resuscitation training for injection drug users to prevent heroin overdose death: a pilot intervention study. J Urban Health. 2005;82(2):303–311. doi: 10.1093/jurban/jti053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jenkins LM, Banta-Green CJ, Maynard C et al. Risk factors for nonfatal overdose at Seattle-area syringe exchanges. J Urban Health. 2011;88(1):118–128. doi: 10.1007/s11524-010-9525-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sherman SG, Cheng Y, Kral AH. Prevalence and correlates of opiate overdose among young injection drug users in a large U.S. city. Drug Alcohol Depend. 2007;88(2-3):182–187. doi: 10.1016/j.drugalcdep.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pollini RA, McCall L, Mehta SH, Celentano DD, Vlahov D, Strathdee SA. Response to overdose among injection drug users. Am J Prev Med. 2006;31(3):261–264. doi: 10.1016/j.amepre.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 55.Wagner KD, Valente TW, Casanova M et al. Evaluation of an overdose prevention and response training programme for injection drug users in the Skid Row area of Los Angeles, CA. Int J Drug Policy. 2010;21(3):186–193. doi: 10.1016/j.drugpo.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Evans JL, Tsui JI, Hahn JA, Davidson PJ, Lum PJ, Page K. Mortality among young injection drug users in San Francisco: a 10-year follow-up of the UFO Study. Am J Epidemiol. 2012;175(4):302–308. doi: 10.1093/aje/kwr318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Seal KH, Downing M, Kral AH et al. Attitudes about prescribing take-home naloxone to injection drug users for the management of heroin overdose: a survey of street-recruited injectors in the San Francisco Bay Area. J Urban Health. 2003;80(2):291–301. doi: 10.1093/jurban/jtg032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Davidson PJ, Ochoa KC, Hahn JA, Evans JL, Moss AR. Witnessing heroin-related overdoses: the experiences of young injectors in San Francisco. Addiction. 2002;97(12):1511–1516. doi: 10.1046/j.1360-0443.2002.00210.x. [DOI] [PubMed] [Google Scholar]
- 59.Sergeev B, Karpets A, Sarang A, Tikhonov M. Prevalence and circumstances of opiate overdose among injection drug users in the Russian Federation. J Urban Health. 2003;80(2):212–219. doi: 10.1093/jurban/jtg024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Powis B, Strang J, Griffiths P et al. Self-reported overdose among injecting drug users in London: extent and nature of the problem. Addiction. 1999;94(4):471–478. doi: 10.1046/j.1360-0443.1999.9444712.x. [DOI] [PubMed] [Google Scholar]
- 61.Kerr T, Fairbairn N, Tyndall M et al. Predictors of non-fatal overdose among a cohort of polysubstance-using injection drug users. Drug Alcohol Depend. 2007;87(1):39–45. doi: 10.1016/j.drugalcdep.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 62.Bennett GA, Higgins DS. Accidental overdose among injecting drug users in Dorset, UK. Addiction. 1999;94(8):1179–1189. doi: 10.1046/j.1360-0443.1999.94811798.x. [DOI] [PubMed] [Google Scholar]
- 63.Bergenstrom A, Quan VM, Van Nam L et al. A cross-sectional study on prevalence of non-fatal drug overdose and associated risk characteristics among out-of-treatment injecting drug users in North Vietnam. Subst Use Misuse. 2008;43(1):73–84. doi: 10.1080/10826080701205109. [DOI] [PubMed] [Google Scholar]
- 64.Havens JR, Oser CB, Knudsen HK et al. Individual and network factors associated with non-fatal overdose among rural Appalachian drug users. Drug Alcohol Depend. 2011;115(1-2):107–112. doi: 10.1016/j.drugalcdep.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fischer B, Brissette S, Brochu S et al. Determinants of overdose incidents among illicit opioid users in 5 Canadian cities. CMAJ. 2004;171(3):235–239. doi: 10.1503/cmaj.1031416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fischer B, Manzoni P, Rehm J. Comparing injecting and non-injecting illicit opioid users in a multisite Canadian sample (OPICAN Cohort) Eur Addict Res. 2006;12(4):230–239. doi: 10.1159/000094425. [DOI] [PubMed] [Google Scholar]
- 67.Tobin KE, Latkin CA. The relationship between depressive symptoms and nonfatal overdose among a sample of drug users in Baltimore, Maryland. J Urban Health. 2003;80(2):220–229. doi: 10.1093/jurban/jtg025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Man LH, Best D, Gossop M, Stillwell G, Strang J. Relationship between prescribing and risk of opiate overdose among drug users in and out of maintenance treatment. Eur Addict Res. 2004;10(1):35–40. doi: 10.1159/000073724. [DOI] [PubMed] [Google Scholar]
- 69.Silva K, Schrager SM, Kecojevic A, Lankenau SE. Factors associated with history of non-fatal overdose among young nonmedical users of prescription drugs. Drug Alcohol Depend. 2013;128(1-2):104–110. doi: 10.1016/j.drugalcdep.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kinner SA, Milloy M, Wood E, Qi J, Zhang R, Kerr T. Incidence and risk factors for non-fatal overdose among a cohort of recently incarcerated illicit drug users. Addict Behav. 2012;37(6):691–696. doi: 10.1016/j.addbeh.2012.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Centers for Disease Control and Prevention. Unintentional and undetermined poisoning deaths—11 States, 1990–2001. MMWR Morbid Mortal Wkly Rep. 2004;53(11):233–238. [PubMed] [Google Scholar]
- 72.Paulozzi LJ, Annest JL. US data show sharply rising drug‐induced death rates. Inj Prev. 2007;13(2):130–132. doi: 10.1136/ip.2006.014357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Paulozzi LJ, Xi Y. Recent changes in drug poisoning mortality in the United States by urban–rural status and by drug type. Pharmacoepidemiol Drug Saf. 2008;17(10):997–1005. doi: 10.1002/pds.1626. [DOI] [PubMed] [Google Scholar]
- 74.Degenhardt L, Day C, Dietze P et al. Effects of a sustained heroin shortage in three Australian States. Addiction. 2005;100(7):908–920. doi: 10.1111/j.1360-0443.2005.01094.x. [DOI] [PubMed] [Google Scholar]
- 75.Edwards EM, Searles J, Shapiro S. Deaths involving drugs in Vermont, 2004 through 2010. Arch Intern Med. 2011;171(18):1676–1678. doi: 10.1001/archinternmed.2011.450. [DOI] [PubMed] [Google Scholar]
- 76.Wunsch MJ, Nakamoto K, Behonick G, Massello W. Opioid deaths in rural Virginia: a description of the high prevalence of accidental fatalities involving prescribed medications. Am J Addict. 2009;18(1):5–14. doi: 10.1080/10550490802544938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hammersley R, Cassidy M, Oliver J, Hammersley R, Cassidy MT, Oliver J. Drugs associated with drug-related deaths in Edinburgh and Glasgow, November 1990 to October 1992. Addiction. 1995;90(7):959–965. doi: 10.1046/j.1360-0443.1995.9079598.x. [DOI] [PubMed] [Google Scholar]
- 78.Shah NG, Lathrop SL, Reichard RR, Landen MG. Unintentional drug overdose death trends in New Mexico, USA, 1990–2005: combinations of heroin, cocaine, prescription opioids and alcohol. Addiction. 2008;103(1):126–136. doi: 10.1111/j.1360-0443.2007.02054.x. [DOI] [PubMed] [Google Scholar]
- 79.Mueller MR, Shah NG, Landen MG. Unintentional prescription drug overdose deaths in New Mexico, 1994–2003. Am J Prev Med. 2006;30(5):423–429. doi: 10.1016/j.amepre.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 80.Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15(9):618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- 81.Fingerhut L. Increases in poisoning and methadone-related deaths: United States, 1999–2005. Centers for Disease Control and Prevention. 2008. Available at: http://www.cdc.gov/nchs/data/hestat/poisoning/poisoning.pdf. Accessed August 14, 2015.
- 82.Centers for Disease Control and Prevention. Drug overdose deaths—Florida, 2003–2009. MMWR Morb Mortal Wkly Rep. 2011;60(26):869–872. [PubMed] [Google Scholar]
- 83.Madden ME, Shapiro SL. The methadone epidemic: methadone-related deaths on the rise in Vermont. Am J Forensic Med Pathol. 2011;32(2):131–135. doi: 10.1097/PAF.0b013e3181e8af3d. [DOI] [PubMed] [Google Scholar]
- 84.Socie E, Hirsch A, Beeghly CB Ohio Department of Health, Centers for Disease Control and Prevention. Columbus, OH: Violence and Injury Prevention Program, Ohio Department of Health; 2010. The Burden of Poisoning in Ohio, 1999–2008. [Google Scholar]
- 85.Wells C. Report: Deaths related to drug poisoning in England and Wales, 2008. Health Stat Q. 2009;(43):48–55. doi: 10.1057/hsq.2009.27. [DOI] [PubMed] [Google Scholar]
- 86.Wisniewski AM, Purdy C, Blondell R. The epidemiologic association between opioid prescribing, non-medical use, and emergency department visits. J Addict Dis. 2008;27(1):1–11. doi: 10.1300/J069v27n01_01. [DOI] [PubMed] [Google Scholar]
- 87.Centers for Disease Control and Prevention. Vital signs: risk for overdose from methadone used for pain relief—United States, 1999–2010. MMWR Morbid Mortal Wkly Rep. 2012;61(26):493–497. [PubMed] [Google Scholar]
- 88.Hawton K, Bergen H, Simkin S, Wells C, Kapur N, Gunnell D. Six-year follow-up of impact of co-proxamol withdrawal in England and Wales on prescribing and deaths: time-series study. PLoS Med. 2012;9(5):e1001213. doi: 10.1371/journal.pmed.1001213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Drug Abuse Warning Network, 2011: National Estimates of Drug-Related Emergency Department Visits. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. HHS publication no. (SMA) 13-4760, DAWN Series D-39. [PubMed] [Google Scholar]
- 90.Green TC, Grau LE, Carver H, Kinzly M, Heimer R. Epidemiologic trends and geographic patterns of fatal opioid intoxications in Connecticut, USA: 1997–2007. Drug Alcohol Depend. 2011;115(3):221–228. doi: 10.1016/j.drugalcdep.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Degenhardt LJ, Conroy E, Gilmour S, Hall W. The effect of a reduction in heroin supply on fatal and non-fatal drug overdoses in New South Wales, Australia. Med J Aust. 2005;182(1):20–23. doi: 10.5694/j.1326-5377.2005.tb06549.x. [DOI] [PubMed] [Google Scholar]
- 92.Calcaterra S, Glanz J, Binswanger I. National trends in pharmaceutical opioid related overdose deaths compared to other substance related overdose deaths: 1999–2009. Drug Alcohol Depend. 2013;131(3):263–270. doi: 10.1016/j.drugalcdep.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cochella S, Bateman K. Provider detailing: an intervention to decrease prescription opioid deaths in Utah. Pain Med. 2011;12(suppl 2):S73–S76. doi: 10.1111/j.1526-4637.2011.01125.x. [DOI] [PubMed] [Google Scholar]
- 94.Johnson EM, Porucznik C, Anderson J, Rolfs R. State-level strategies for reducing prescription drug overdose deaths: Utah’s prescription safety program. Pain Med. 2011;12(suppl 2):S66–S72. doi: 10.1111/j.1526-4637.2011.01126.x. [DOI] [PubMed] [Google Scholar]
- 95.Scott G, Thomas SD, Pollack HA, Ray B. Observed patterns of illicit opiate overdose deaths in Chicago, 1999–2003. J Urban Health. 2007;84(2):292–306. doi: 10.1007/s11524-007-9157-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Marshall BD, Milloy MJ, Wood E, Montaner JS, Kerr T. Reduction in overdose mortality after the opening of North America’s first medically supervised safer injecting facility: a retrospective population-based study. Lancet. 2011;377(9775):1429–1437. doi: 10.1016/S0140-6736(10)62353-7. [DOI] [PubMed] [Google Scholar]
- 97.Wood E, Stoltz JA, Li K, Montaner JS, Kerr T. Changes in Canadian heroin supply coinciding with the Australian heroin shortage. Addiction. 2006;101(5):689–695. doi: 10.1111/j.1360-0443.2006.01385.x. [DOI] [PubMed] [Google Scholar]
- 98.Friedman LS. Real-time surveillance of illicit drug overdoses using poison center data. Clin Toxicol (Phila) 2009;47(6):573–579. doi: 10.1080/15563650902967404. [DOI] [PubMed] [Google Scholar]
- 99.Schwartz RP, Gryczynski J, O’Grady KE et al. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995–2009. Am J Public Health. 2013;103(5):917–922. doi: 10.2105/AJPH.2012.301049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Maxwell S, Bigg D, Stanczykiewicz K, Carlberg-Racich S. Prescribing naloxone to actively injecting heroin users: a program to reduce heroin overdose deaths. J Addict Dis. 2006;25(3):89–96. doi: 10.1300/J069v25n03_11. [DOI] [PubMed] [Google Scholar]
- 101.Neeleman J, Farrell M. Fatal methadone and heroin overdoses: time trends in England and Wales. J Epidemiol Community Health. 1997;51(4):435–437. doi: 10.1136/jech.51.4.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Duncan DF. Drug law enforcement expenditures and drug-induced deaths. Psychol Rep. 1994;75(1 pt 1):57–58. doi: 10.2466/pr0.1994.75.1.57. [DOI] [PubMed] [Google Scholar]
- 103.Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief. 2011;81(22):1–8. [PubMed] [Google Scholar]
- 104.Merrall EL, Bird SM, Hutchinson SJ. Mortality of those who attended drug services in Scotland 1996–2006: record-linkage study. Int J Drug Policy. 2012;23(1):24–32. doi: 10.1016/j.drugpo.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shah NG, Lathrop SL, Flores JE, Landen MG. The influence of living along the U.S.–Mexico border on unintentional drug overdose death, New Mexico (USA), 2005–2009. Drug Alcohol Depend. 2012;125(1-2):19–26. doi: 10.1016/j.drugalcdep.2012.02.023. [DOI] [PubMed] [Google Scholar]
- 106.Farrell M, Marsden J. Acute risk of drug-related death among newly released prisoners in England and Wales. Addiction. 2008;103(2):251–255. doi: 10.1111/j.1360-0443.2007.02081.x. [DOI] [PubMed] [Google Scholar]
- 107.Marshall BD, Milloy M-J, Wood E, Galea S, Kerr T. Temporal and geographic shifts in urban and non-urban cocaine-related fatal overdoses in a Canadian setting. Ann Epidemiol. 2012;22(3):198–206. doi: 10.1016/j.annepidem.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 108.Milloy MJ, Wood E, Reading C, Kane D, Montaner J, Kerr T. Elevated overdose mortality rates among First Nations individuals in a Canadian setting: a population-based analysis. Addiction. 2010;105(11):1962–1970. doi: 10.1111/j.1360-0443.2010.03077.x. [DOI] [PubMed] [Google Scholar]
- 109.Harlow KC. Patterns of rates of mortality from narcotics and cocaine overdose in Texas, 1976–87. Public Health Rep. 1990;105(5):455–462. [PMC free article] [PubMed] [Google Scholar]
- 110.Coffin PO, Galea S, Ahern K, Leon A, Vlahov D, Tardiff K. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990–98. Addiction. 2003;98(6):739–747. doi: 10.1046/j.1360-0443.2003.00376.x. [DOI] [PubMed] [Google Scholar]
- 111.Torralba L, Brugal MT, Villalbi JR, Tortosa MT, Toribio A, Valverde JL. Mortality due to acute adverse drug reactions: opiates and cocaine in Barcelona, 1989–93. Addiction. 1996;91(3):419–426. doi: 10.1046/j.1360-0443.1996.91341911.x. [DOI] [PubMed] [Google Scholar]
- 112.Marzuk PM, Tardiff K, Leon AC et al. Poverty and fatal accidental drug overdoses of cocaine and opiates in New York City: an ecological study. Am J Drug Alcohol Abuse. 1997;23(2):221–228. doi: 10.3109/00952999709040943. [DOI] [PubMed] [Google Scholar]
- 113.Tardiff K, Marzuk P, Leon A et al. Accidental fatal drug overdoses in New York City: 1990–1992. Am J Drug Alcohol Abuse. 1996;22(2):135–146. doi: 10.3109/00952999609001650. [DOI] [PubMed] [Google Scholar]
- 114.Stenbacka M, Leifman A, Romelsjo A. Mortality and cause of death among 1705 illicit drug users: a 37-year follow up. Drug Alcohol Rev. 2010;29(1):21–27. doi: 10.1111/j.1465-3362.2009.00075.x. [DOI] [PubMed] [Google Scholar]
- 115.Vlahov D, Wang C, Ompad D et al. Mortality risk among recent-onset injection drug users in five U.S. cities. Subst Use Misuse. 2008;43(3-4):413–428. doi: 10.1080/10826080701203013. [DOI] [PubMed] [Google Scholar]
- 116.Hickman M, Hope V, Coleman B et al. Assessing IDU prevalence and health consequences (HCV, overdose and drug-related mortality) in a primary care trust: implications for public health action. J Public Health (Oxf) 2009;31(3):374–382. doi: 10.1093/pubmed/fdp067. [DOI] [PubMed] [Google Scholar]
- 117.Manfredi R, Sabbatani S, Agostini D. Trend of mortality observed in a cohort of drug addicts of the metropolitan area of Bologna, North-Eastern Italy, during a 25-year-period. Coll Antropol. 2006;30(3):479–488. [PubMed] [Google Scholar]
- 118.Miller CL, Kerr T, Strathdee SA, Li K, Wood E. Factors associated with premature mortality among young injection drug users in Vancouver. Harm Reduct J. 2007;4:1. doi: 10.1186/1477-7517-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wang C, Vlahov D, Galai N et al. The effect of HIV infection on overdose mortality. AIDS. 2005;19(9):935–942. doi: 10.1097/01.aids.0000171407.30866.22. [DOI] [PubMed] [Google Scholar]
- 120.Brettle RP, Chiswick A, Bell J et al. Pre-AIDS deaths in HIV infection related to intravenous drug use. QJM. 1997;90(10):617–629. doi: 10.1093/qjmed/90.10.617. [DOI] [PubMed] [Google Scholar]
- 121.Davidson PJ, McLean R, Kral A, Gleghorn A, Edlin B, Moss A. Fatal heroin-related overdose in San Francisco, 1997–2000: a case for targeted intervention. J Urban Health. 2003;80(2):261–273. doi: 10.1093/jurban/jtg029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ruttenber AJ, Luke JL. Heroin-related deaths: new epidemiologic insights. Science. 1984;226(4670):14–20. doi: 10.1126/science.6474188. [DOI] [PubMed] [Google Scholar]
- 123.Centers for Disease Control and Prevention. Vital signs: prescription painkiller overdoses: use and abuse of methadone as a painkiller. National Center for Injury Prevention and Control. 2012. Available at: http://www.cdc.gov/VitalSigns/pdf/2012-07-vitalsigns.pdf. Accessed August 14, 2015.
- 124.Soyka M, Apelt S, Lieb M, Wittchen H. One-year mortality rates of patients receiving methadone and buprenorphine maintenance therapy: a nationally representative cohort study in 2694 patients. J Clin Psychopharmacol. 2006;26(6):657–660. doi: 10.1097/01.jcp.0000245561.99036.49. [DOI] [PubMed] [Google Scholar]
- 125.Hall AJ, Logan JE, Toblin RL et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300(22):2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- 126.Niveau G. Rougemont AL, La Harpe R. Methadone maintenance treatment, criminality and overdose-related deaths. An ecological study, 1983–1999. Eur J Public Health. 2002;12(3):224–227. doi: 10.1093/eurpub/12.3.224. [DOI] [PubMed] [Google Scholar]
- 127.Albert S, Brason FW, II, Sanford CK, Dasgupta N, Graham J, Lovette B. Project Lazarus: community-based overdose prevention in rural North Carolina. Pain Med. 2011;12(suppl 2):S77–S85. doi: 10.1111/j.1526-4637.2011.01128.x. [DOI] [PubMed] [Google Scholar]
- 128.Bird SM. Over 1200 drugs-related deaths and 190,000 opiate-users-years of follow-up: relative risks by sex and age group. Addict Res Theory. 2010;18:194–207. [Google Scholar]
- 129.Bargagli AM, Hickman M, Davoli M et al. Drug-related mortality and its impact on adult mortality in eight European countries. Eur J Public Health. 2006;16(2):198–202. doi: 10.1093/eurpub/cki168. [DOI] [PubMed] [Google Scholar]
- 130.Clausen T, Waal H, Thoresen M, Gossop M. Mortality among opiate users: opioid maintenance therapy, age and causes of death. Addiction. 2009;104(8):1356–1362. doi: 10.1111/j.1360-0443.2009.02570.x. [DOI] [PubMed] [Google Scholar]
- 131.Shah R, Uren Z, Baker A, Majeed A. Trends in deaths from drug overdose and poisoning in England and Wales 1993–1998. J Public Health Med. 2001;23(3):242–246. doi: 10.1093/pubmed/23.3.242. [DOI] [PubMed] [Google Scholar]
- 132.Morgan O, Griffiths C, Baker A, Majeed A. Fatal toxicity of antidepressants in England and Wales, 1993–2002. Health Stat Q. 2004;(23):18–24. [PubMed] [Google Scholar]
- 133.Rocchi MB, Miotto P, Preti A. Distribution of deaths by unintentional illicit drug overdose in Italy based on periodicity over time, 1984–2000. Drug Alcohol Depend. 2003;72(1):23–31. doi: 10.1016/s0376-8716(03)00186-8. [DOI] [PubMed] [Google Scholar]
- 134.Fischer B, Jones W, Rehm J. High correlations between levels of consumption and mortality related to strong prescription opioid analgesics in British Columbia and Ontario, 2005–2009. Pharmacoepidemiol Drug Saf. 2013;22(4):438–442. doi: 10.1002/pds.3404. [DOI] [PubMed] [Google Scholar]
- 135.Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013;309(7):657–659. doi: 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- 136.Krinsky CS, Lathrop SL, Crossey M, Baker G, Zumwalt R. A toxicology-based review of fentanyl-related deaths in New Mexico (1986–2007) Am J Forensic Med Pathol. 2011;32(4):347–351. doi: 10.1097/PAF.0b013e31822ad269. [DOI] [PubMed] [Google Scholar]
- 137.Boddiger D. Fentanyl-laced street drugs “kill hundreds.”. Lancet. 2006;368(9535):569–570. doi: 10.1016/S0140-6736(06)69181-2. [DOI] [PubMed] [Google Scholar]
- 138.Soloway RA. Street-smart advice on treating drug overdoses. Am J Nurs. 1993;93(9):65–72. doi: 10.1097/00000446-199309000-00027. [DOI] [PubMed] [Google Scholar]
- 139.Cook S, Moeschler O, Michaud K, Yersin B. Acute opiate overdose: characteristics of 190 consecutive cases. Addiction. 1998;93(10):1559–1565. doi: 10.1046/j.1360-0443.1998.9310155913.x. [DOI] [PubMed] [Google Scholar]
- 140.New York City Department of Health and Mental Hygiene. Illicit drug use in New York City. NYC Vital Signs. 2010;9(1):1–4. [Google Scholar]
- 141.Andrews JY, Kinner SA. Understanding drug-related mortality in released prisoners: a review of national coronial records. BMC Public Health. 2012;12:270. doi: 10.1186/1471-2458-12-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Clark MJ, Bates AC. Nonfatal heroin overdoses in Queensland, Australia: an analysis of ambulance data. J Urban Health. 2003;80(2):238–247. doi: 10.1093/jurban/jtg027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Dietze P, Jolley D, Cvetkovski S. Patterns and characteristics of ambulance attendance at heroin overdose at a local-area level in Melbourne, Australia: implications for service provision. J Urban Health. 2003;80(2):248–260. doi: 10.1093/jurban/jtg028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Degenhardt L, Hall W, Adelstein B. Ambulance calls to suspected overdoses: New South Wales patterns July 1997 to June 1999. Aust N Z J Public Health. 2001;25(5):447–450. [PubMed] [Google Scholar]
- 145.Nandi A, Galea S, Ahern J, Bucciarelli A, Vlahov D, Tardiff K. What explains the association between neighborhood-level income inequality and the risk of fatal overdose in New York City? Soc Sci Med. 2006;63(3):662–674. doi: 10.1016/j.socscimed.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 146.Cerdá M, Ransome Y, Keyes KM et al. Revisiting the role of the urban environment in substance use: the case of analgesic overdose fatalities. Am J Public Health. 2013;103(12):2252–2260. doi: 10.2105/AJPH.2013.301347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Gotsens M, Mari-Dell’Olmo M, Martinez-Beneito MA et al. Socio-economic inequalities in mortality due to injuries in small areas of ten cities in Spain (MEDEA Project) Accid Anal Prev. 2011;43(5):1802–1810. doi: 10.1016/j.aap.2011.04.013. [DOI] [PubMed] [Google Scholar]
- 148.Siegel S. Pavlovian conditioning and drug overdose: when tolerance fails. Addict Res Theory. 2001;9(5):503–513. [Google Scholar]
- 149.Simoni-Wastila L, Ritter G, Strickler G. Gender and other factors associated with the nonmedical use of abusable prescription drugs. Subst Use Misuse. 2004;39(1):1–23. doi: 10.1081/ja-120027764. [DOI] [PubMed] [Google Scholar]
- 150.Raofi S, Schappert S. Medication therapy in ambulatory medical care; United States, 2003–2004. Vital Health Stat. 2006;13(163):1–40. [PubMed] [Google Scholar]
- 151.Rustøen T, Wahl AK, Hanestad BR, Lerdal A, Paul S, Miaskowski C. Gender differences in chronic pain—findings from a population-based study of Norwegian adults. Pain Manag Nurs. 2004;5(3):105–117. doi: 10.1016/j.pmn.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 152.Hunter J, Smith B, Gribbin M. Demographic variables and chronic pain. Clin J Pain. 2001;17(4 suppl):S14–S19. doi: 10.1097/00002508-200112001-00006. [DOI] [PubMed] [Google Scholar]
- 153.Centers for Disease Control and Prevention. Prescription painkiller overdoses: a growing epidemic, especially among women. 2013. Available at: http://www.cdc.gov/vitalsigns/PrescriptionPainkillerOverdoses/index.html. Accessed August 14, 2015.
- 154.Cheng M, Sauer B, Johnson E, Porucznik C, Hegmann K. Comparison of opioid-related deaths by work-related injury. Am J Ind Med. 2013;56(3):308–316. doi: 10.1002/ajim.22138. [DOI] [PubMed] [Google Scholar]
- 155.Green TC, McGowan S, Yokell M, Pouget E, Rich J. HIV infection and risk of overdose: a systematic review and meta-analysis. AIDS. 2012;26(4):403–417. doi: 10.1097/QAD.0b013e32834f19b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Stewart LM, Henderson C, Hobbs M, Ridout S, Knuiman M. Risk of death in prisoners after release from jail. Aust N Z J Public Health. 2004;28(1):32–36. doi: 10.1111/j.1467-842x.2004.tb00629.x. [DOI] [PubMed] [Google Scholar]
- 157.Wines JD, Saitz R, Horton N, Lloyd-Travaglini C, Samet J. Overdose after detoxification: a prospective study. Drug Alcohol Depend. 2007;89(2-3):161–169. doi: 10.1016/j.drugalcdep.2006.12.019. [DOI] [PubMed] [Google Scholar]
- 158.Bohnert AS, Ilgen MA, Ignacio RV, McCarthy JF, Valenstein M, Blow FC. Risk of death from accidental overdose associated with psychiatric and substance use disorders. Am J Psychiatry. 2012;169(1):64–70. doi: 10.1176/appi.ajp.2011.10101476. [DOI] [PubMed] [Google Scholar]
- 159.Ødegård E, Rossow I. Alcohol and non-fatal drug overdoses. Eur Addict Res. 2004;10(4):168–172. doi: 10.1159/000079838. [DOI] [PubMed] [Google Scholar]
- 160.Boyes AP. Repetition of overdose: a retrospective 5-year study. J Adv Nurs. 1994;20(3):462–468. doi: 10.1111/j.1365-2648.1994.tb02382.x. [DOI] [PubMed] [Google Scholar]
- 161. Volkow ND. Prescription opioid and heroin abuse: witness appearing before the House Committee on Energy and Commerce Subcommittee on Oversight and Investigations: Department of Health and Human Services, National Institutes of Health; April 29, 2014.
- 162.Logan J, Liu Y, Paulozzi L, Zhang K, Jones C. Opioid prescribing in emergency departments: the prevalence of potentially inappropriate prescribing and misuse. Med Care. 2013;51(8):646–653. doi: 10.1097/MLR.0b013e318293c2c0. [DOI] [PubMed] [Google Scholar]
- 163.National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System: leading causes of death reports. 2008 [Google Scholar]
- 164.Shai D. Problems of accuracy in official statistics on drug-related deaths. Int J Addict. 1994;29(14):1801–1811. doi: 10.3109/10826089409128258. [DOI] [PubMed] [Google Scholar]
- 165.Skopp G. Postmortem toxicology. Forensic Sci Med Pathol. 2010;6(4):314–325. doi: 10.1007/s12024-010-9150-4. [DOI] [PubMed] [Google Scholar]
- 166.Pounder DJ, Fuke C, Cox DE, Smith D, Kuroda N. Postmortem diffusion of drugs from gastric residue: an experimental study. Am J Forensic Med Pathol. 1996;17(1):1–7. doi: 10.1097/00000433-199603000-00001. [DOI] [PubMed] [Google Scholar]
- 167.Pounder DJ, Adams E, Fuke C, Langford A. Site to site variability of post-mortem drug concentration in liver and lung. J Forensic Sci. 1996;41(6):927–932. [PubMed] [Google Scholar]
- 168.Kostakis C, Byard R. Sudden death associated with intravenous injection of toad extract. Forensic Sci Int. 2009;188(1-3):e1–e5. doi: 10.1016/j.forsciint.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 169.Webster LR, Dasgupta N. Obtaining adequate data to determine causes of opioid-related overdose deaths. Pain Med. 2011;12(suppl 2):S86–S92. doi: 10.1111/j.1526-4637.2011.01132.x. [DOI] [PubMed] [Google Scholar]