Abstract
To review the meniscus from a historical perspective especially on surgical management and general guidelines for arthroscopic meniscectomy procedures for various types of meniscal tears. We searched MEDLINE and PubMed for the years of 1980-2010 using the terms meniscus, meniscal repair, menisectomy, and arthroscopy. Orthopedic surgeons frequently encounter patients with pain or functional impairment of the knee joint and repair or resection of the injured meniscus is one of the most common orthopedic operative procedures. The object of meniscal surgery is to reduce pain, restore functional meniscus and prevent the development of degenerative osteoarthritis in the involved knee. Historically, total meniscectomy was a common procedure performed for meniscus tear symptoms. However, it has been reported that total meniscectomy has deleterious effects on the knee. In the past, the menisci were thought as a functionless remnant tissue. Currently, it is known that the meniscus is an important structure for knee joint function. Menisci provide several vital functions including mechanical support, localized pressure distribution, and lubrication to the knee joint. It is widely accepted that the function of the meniscus can be preserved through minimal excision. An arthroscopic partial meniscectomy preserving more of the meniscus is preferred over total meniscectomy. In recent decades, this shift toward arthroscopic partial meniscectomy has led to the development of new surgical techniques.
Keywords: Menisectomy, Arthroscopy, Prognosis
Introduction
Meniscal injury is a common source of pain and functional impairment of the knee that is frequently encountered by orthopedic surgeons1), and approximately 61 in 100,000 meniscal injury patients undergo meniscectomy2). The goals of surgical intervention for meniscal tears are to relieve pain, facilitate pre-injury level daily living activities, and prevent early degeneration of the knee joint. In the past, meniscectomy was the standard operation because the meniscus was considered a functionless remnant vestige3). In 1942, McMurray4) described that insufficient removal of the meniscus was the cause of failure of meniscectomy. Currently, the meniscus is recognized as being vital for the normal biomechanics of the knee and efforts are made to preserve the meniscus as much as possible to prevent degenerative arthritis. With the increased understanding of the structure, function, and biology of the meniscus and development of new surgical methods, meniscal repair techniques have been improved and arthroscopic partial meniscectomy is preferred over total meniscectomy. However, not all meniscal tears can be repaired and meniscectomy is unavoidable in many cases. In this review article, we review the relevant literature on the anatomical characteristics and biomechanics of the meniscus and describe the principles and indications for arthroscopic meniscectomy.
Anatomy and Function of the Meniscus
The menisci are located between the femur and the tibia. The wedge-shaped fibrocartilaginous structures are situated in the medial and lateral condyles and the anterior horns are connected to each other by a transverse ligament. The menisci, once thought as a vestige of leg muscle, have been considered as a vital structure with various functions: chondropotection through weight distribution by enlarging the contact area between the femur and the tibia5), weight bearing6), joint stabilization2), joint lubrication7), articular cartilage nutrition8), and proprioception9). In 1976, Krause et al.10) reported on the load-transmitting and energy-absorbing functions of the meniscus and Ahmed and Burke11) reported that the medial meniscus transmits 50% of the joint load whereas the lateral meniscus transmits 70% of the joint load.
The medial meniscus is C-shaped and its posterior horn is wider than the anterior horn and the anteroposterior dimension is larger than the mediolateral dimension. Compared to the lateral meniscus, it is larger and more frequently torn because of less mobility caused by firm attachment to the tibial plateau via the coronary ligament. It contributes to the anterior stability of the knee and thus is more vulnerable to tear in anterior cruciate ligament (ACL)-deficient knees. The lateral meniscus is smaller and more circular and covers a larger portion of the articular surface than the medial meniscus does. The posterior horn is connected lateral to the medial epicondyle of the femur via Wrisberg or Humphrey ligament. Although being attached to the articular capsule and the tibia, it is separated posterolaterally from the capsule by the popliteus tendon and thus is more mobile compared to the medial meniscus. Microscopic observation of the meniscus shows a fibrocartilaginous tissue made up of fibroblasts and chondrocytes. The fibrocartilage tissue synthesizes extracellular matrix that is predominantly type I collagen (90-95%). The orientation of collagen fibers is mainly circumferential with some radial and perforation fibers. The predominance of circumferential fibers in the outer one third of the meniscus is effective for distribution of hoop tension that develops due to weight bearing. Other constituents include proteoglycans, elastin, and small amounts of other types of collagen, and water (70%)12). The menisci are relatively avascular excluding 3-5 mm of the peripheral rim (10-30% of the width of the medial and 10-25% of the width of the lateral meniscus) where the parameniscal capillary plexus supplies blood to the synovial and capsular tissues. The vascularized area can be classified into the red-red zone, red-white zone, and white-white zone according to the degree of vascularity13). The capillary plexus gradually decreases with age.
Diagnosis of Meniscal Injuries
The key to the diagnosis of meniscal injuries is careful history taking and assessment of subjective symptoms. The most common symptoms of meniscal injuries include pain along the joint line, swelling, effusions, stiffness, cracking, and locking or catching. Athletes with meniscal tears commonly describe they felt a pop when suddenly stopping or changing directions while running14). Locking is the inability to fully extend the knee that occurs when a torn meniscus fragment gets caught in the hinge mechanism of the knee. It can occur secondary to other conditions including cartilage injuries and patellofemoral chondrosis. For physical examination, the McMurray test and Apley test can be performed as adjunct clinical diagnostic tests in addition to joint line palpation. Imaging modalities, especially magnetic resonance imaging (MRI), are essential for accurate diagnosis. MRI has an accuracy of 64-95% for the diagnosis of meniscal injuries with a sensitivity of 88% sensitivity and a specificity of 57%15).
Meniscal Tear Classification
Tears can be classified according to the arthroscopically observed tear patterns or etiology of the injury. Most commonly, they are classified into vertical longitudinal, oblique, circumferential, complex, transverse or radial, and horizontal cleavage tears12). Of these, radial tears of the posteromedial compartment are the most frequently seen tears and vertical longitudinal tears are most often associated with acute ACL injury16). Degenerative complex tears that generally start from the posterior horn are common in older patients.
Most meniscal tears do not heal spontaneously. Henning et al.17) reported some tears that heal naturally or remain asymptomatic include ≤10 mm short stable vertical longitudinal tears, stable partial tears (≤50% of the meniscal thickness), and ≤3 mm shallow tears. Tear pattern, location, and vascularity are important factors for treatment decision making. The location of a tear can be red-red, red-white, or white-white zone according to the vascular supply and healing prognosis. The red-red zone is fully vascular with an excellent healing prognosis. The red-white zone has vascularity along the periphery only and a good healing prognosis. However, the white-white zone that is completely avascular has a poor prognosis14).
Meniscectomy
1. Total Meniscectomy
In 1897, Bland-Sutton18) described the menisci as "functionless remnants of intra-articular leg muscles" in Ligaments: their nature and morphology. Surgical removal of the meniscus had been introduced in the late 19th century3) and open total meniscectomy was considered as the standard approach for most of the 20th century. It was because studies showed excellent short-term results of meniscectomy including return to hard work or sports19). On the other hand, unfavorable long-term results of total meniscectomy have been documented in the literature20). There are various reports on the biomechanics of the knee after meniscectomy. In 1923, McMurray4) reported that meniscectomy could result in arthritis suggesting a relationship between secondary arthritis and pain affected by weather changes. In 1936, King21) reported that the amount of degeneration was proportional to the size of the removed segment during meniscectomy. In 1948, Fairbank22) described that meniscectomy could predispose degenerative changes if the meniscus is damaged during the procedure, which led surgeons to realize the importance of the menisci and the outcomes of the meniscus removal. In 1976, Krause et al.10) reported that partial meniscectomy caused a 1/3 decrease in the contact area and accordingly three times increase in weight bearing in the knee joint. According to the study by Baratz et al.23) in 1986, the contact area decreased by approximately 75% and the peak contact pressure increased by approximately 235% after medial meniscectomy. In the study by Ahmed and Burke11), pressure on the meniscus increased by 85% in flexion and the contact pressure increased by 100-200% after total meniscectomy. The increase in contact pressure after meniscecomy causes overload of articular cartilage, which results in proteoglycan loss and disaggregation and increased hydration24). The influence of meniscectomy on articular cartilage dysfunction was confirmed with the naked eye or microscopically in animal models25). Tapper and Hoover26) followed 213 patients who had undergone total meniscectomy for 10-30 years and found that only 68% of them obtained good or excellent results and only 38% had no postoperative symptoms. The outcome can be satisfactory when the peripheral rim is preserved in bucket hand tears25). Yocum et al.27) observed that only 54% of the 26 patients achieved satisfactory results at 7 years after meniscectomy and 20 patients had limited range of motion. These study results indicate that meniscectomy is not a harmless procedure. Thus, efforts have been made to preserve the meniscus as much as possible during repair to avoid complications of total meniscectomy3), and partial meniscectomy has been recommended as an alternative when repair is not possible.
2. Partial Meniscectomy
Since first introduced by Ikeuchi28) in the 1960s, arthroscopic meniscectomy has been improved to cause less damage to the meniscus with the development of arthroscopic surgical equipment and techniques. Partial meniscectomy has been preferred over total meniscectomy for symptomatic meniscus injuries. One of the major advantages of the procedure is that the peripheral rim of the meniscus that is responsible for biomechanical function of the knee can be preserved. In addition, arthroscopic partial removal facilitates rapid rehabilitation and early functional recovery with low morbidity. Northmore-Ball et al.29) reported that postoperative satisfaction (good or excellent) was remarkably higher after arthroscopic partial meniscectomy (90%) than open total meniscectomy (68%). Medial meniscecotmy has been thought to produce better results than lateral meniscectomy30). McNicholas et al.31) reported that only 47% of the patients had good or excellent results after lateral meniscecotmy, whereas 80% of the patients were satisfied with the results after medial meniscecotmy. In the study by Burks et al.32), good or excellent results were observed in 88% of the patients at 15 years after surgery, but there were no notable differences between medial and lateral meniscecotmy. After medial meniscectomy, patients with a valgus deformity obtained more satisfactory results and 0.24% lower osteoarthritis grade than those with a varus deformity in the study. Lee et al.33) reported that partial meniscectomy had significance influence on the tibiaofemoral contact mechanics. They measured changes in the contact area and contact stress according to the degree of meniscus resection with the knee in 0°, 30°, and 60° flexion and found that meniscectomy decreases the tibiofemoral contact area and increases the mean contact stress and peak contact stress regardless of the extent of removal. Accordingly, they suggested that the meniscus should be preserved as much as possible during meniscectomy. The short-term results of partial meniscectomy are good. Jaureguito et al.34) reported that 90% of the patients obtained good or excellent results and 85% of the patients could resume their pre-injury level activities at 2 years after partial meniscectomy. However, only 62% of the patients exhibited good or excellent results and only 48% could maintain their pre-injury activity level at 8 years after surgery. In a recent MRI study, radiographic degenerative changes were observed at 5 years after partial meniscectomy in patients who had had normal articular cartilage at the time of surgery35). Partial meniscecotmy appears to produce better results than total meniscecotmy based on biomechanical and clinical evidence. However, we believe that partial meniscus removal is a procedure that causes abnormal biomechanical changes in the knee joint and thus degenerative changes of the articular cartilage can occur accordingly.
The importance of partial meniscecotmy lies in the fact that the peripheral rim of the meniscus that is crucial to the biomechanics of the knee joint can be preserved. In addition, an arthroscopically-assisted procedure would lower morbidity and promote rapid rehabilitation and early functional recovery.
3. Radiographic Changes after Meniscectomy
In 1948, Fairbank22) described radiographic changes of the knee joint in 107 patients after meniscectomy including osteophyte formation on the femoral condyle, squaring of the femoral condyle, and joint space narrowing. Afterwards, radiographic changes after meniscectomy have been the subject of a variety of studies. However, direct comparison of these studies is difficult because of differences in the study populations, surgical techniques, follow-up period, radiographic assessment standards, and the quality of studies36,37). There is no consensus on the relationship between radiographic changes and clinical outcomes. According to Appel38), clinical results and radiographic findings are not always consistent. Scheller et al.39) noted a high percentage of radiographic changes in 75 patients at 5-15 years after partial meniscectomy, but it was not related to subjective symptoms or functional outcome. On the other hand, Roos et al.40) found that radiographic degenerative changes were related to severe pain and dysfunction in 156 patients at 17-22 years after open meniscectomy. Johnson et al.41) observed at least one of the Fairbank's changes in 74% of the patients after total meniscectomy and 39.4% degenerative changes in the meniscectomized knees compared to 6% changes in the contralateral knees. They correlated the number of Fairbank's changes with poor outcomes. In addition, the results were significantly better after medial meniscectomy than lateral meniscectomy and after either medial or lateral removal than removal of both menisci. Jorgensen et al.42) investigated the results of meniscectomy for an isolated meniscus injury in 147 athletes. Radiographic deterioration started at 4.5 years postoperatively and was observed in 89% of the patients at 14.5 years postoperatively. Thus, 46% of the athletes either gave up or reduced sporting activities, which is higher than the percentage in non-athletic patients. Therefore, it is our understanding that meniscectomy can increase the risk of radiographic degenerative changes, which is expected to progress over a long-term period resulting in decreased patient satisfaction.
Indications
Not all meniscal injuries require surgical intervention. The indications for meniscectomy include symptoms refractory to conservative treatment, symptoms that affect activities of daily living, mechanical symptoms (locking, catching, and giving way), avascular zone tears, coexisting degenerative or synovial fluid changes. In case of bucket handle tears where the torn fragment is displaced to the center of the joint, meniscectomy can be an option if anatomic reduction of the fragment is impossible due to degenerative changes or deformation or possible but not maintainable. Other factors that should be considered in making a surgical treatment decision include lower limb alignment, degenerative changes of the articular cartilage, patient's age and level of activity, obesity level, and quadriceps atrophy. Tears that are stable (<1 cm in length) or MRI-detected horizontal tears in the posterior horn do not necessitate a meniscectomy. Partial meniscectomy for horizontal tears in the posterior horn that are usually accompanied by degenerative arthritis should be determined with care because the arthritis can progress drastically after the procedure causing more pain and effusion43). For MRI-detected tears without mechanical symptoms that can be identified through physical examination or history taking, conservative treatment should be the first line of treatment. The goals of meniscectomy are to remove the torn fragment that lodges between the tibia and the femur during joint movements, prevent recurrence by repairing the inner torn portion of the meniscus, stabilize the joint by preserving the capsular attachments of the meniscus as much as possible, and maintain normal articular cartilage by avoiding damage during meniscectomy.
Surgical Techniques
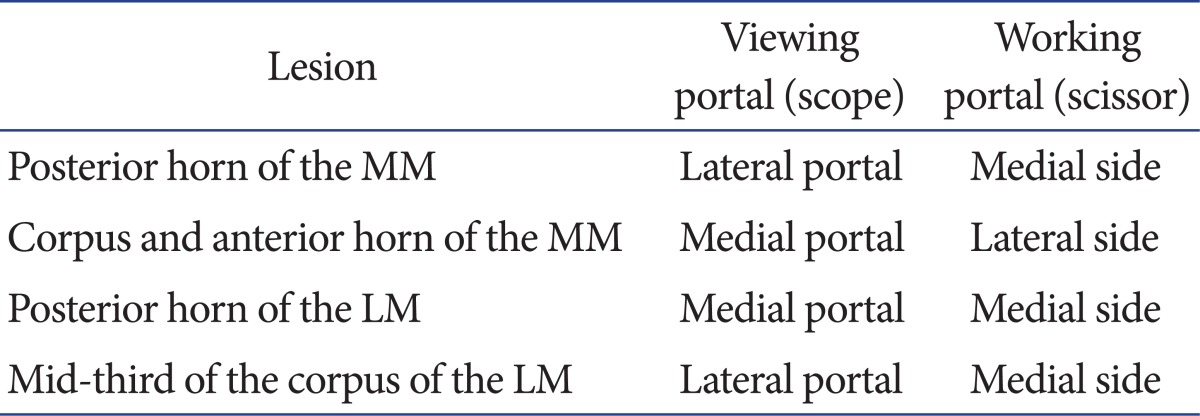
Meniscectomy can be performed using a piecemeal excision or one piece excision technique or a combination of both. Considering that meniscal tears are various in tear pattern and location, the surgeon should be familiar with different types of surgical equipment and alternate use of viewing and working portals. An arthroscope should be placed in the optimal spot and surgical equipment should be positioned as described in Table 1 according to the tear site.
Table 1.
Portal Locations according to Injured Meniscus Sites
MM: medial meniscus, LM: lateral meniscus.
Meniscectomies are generally performed according to the following guidelines43,44): 1) remove with a probe all mobile fragments that are pulled past an imaginary line drawn along the inner margin of the meniscus to the center of the joint, 2) trim the contour to prevent further tearing that can be caused by drastic changes in the shape of the meniscus, 3) it is not necessary to obtain a perfectly smooth rim because remodeling process occurs within 6-9 months45,46), 4) determine the extent of resection by frequently assessing the mobility and texture of the remaining meniscus using a probe. Texture of the normal meniscus should be relatively firm, whereas a damaged or degenerative portion is relatively soft or mushy, 5) It is recommended to preserve the portion where damage is uncertain, 6) use manual instruments for delicate resection or tactile feedback and motorized instruments for debris removal or trimming of frayed fragments, 7) Protect the meniscocapsular junction to preserve the load transmission properties of the remaining rim.
1. Vertical Longitudinal Tear Resection
Identify the tear size through the contralateral portal and reduce the tear. Partially cut the posterior attachment leaving a small bridge of tissue and then completely cut the anterior attachment. Grasp the meniscal fragment anteriorly and detach it from the posterior horn. Remove the central fragment to smoothen the contour and trim the anterior and posterior attachment sites taking care to ensure no occult second tear is hidden behind the central fragment. Probe the incomplete inferior surface of the tear to determine the stability.
2. Oblique Tear Resection
Approach the oblique tear posteriorly. Morselize the fragment using basket forceps or remove a large tear en bloc. Cut the anterior oblique tear with arthroscopic scissors and remove the fragment using a grasper. Trim the anterior and posterior edges of the meniscus to prevent stress risers in the remaining meniscal rim45).
3. Transverse or Radial Tear Resection
After probing the tear, contour the posterior fragment using basket forceps and resect the anterior corner using 90° basket forceps. Preserve sufficient amount of meniscal tissue to create a C-shaped contour.
4. Horizontal Cleavage Tear Resection
After determining whether one or both of the leaves should be resected according to their stability, resect one or both of the flaps of the tear to the end of the cleavage plane using basket forceps. Probe the depth of the tear and if the thickest portion of the remaining leaf is 1-2 mm, resect the remaining leaf. Smoothen the peripheral rim.
5. Degenerative Tear Resection
Remove major flaps with basket forceps and trim the edges using a motorized resector.
Complications
Intraoperative complications of meniscectomy include neurovascular damages, instrument breakage, and anesthesia complications. The most common postoperative complications include deep vein thrombosis, infection, synovitis, arthrofibrosis, effusion, hemarthrosis, extra-articular edema, postoperative stiffness, and continuous pain.
Rehabilitation
Rehabilitation after partial meniscectomy can be performed as tolerated without restrictions or limitations. The goals of postoperative rehabilitation are improvement of symptoms, functional recovery, and prevention of additional damage. Functional recovery refers to maintenance or recovery of range of motion (ROM), general condition, muscle function, and lower extremity neuromuscular coordination47). There are no standard protocols for postoperative rehabilitation. In general, it follows a progressive phasic approach and consists of immediate progressive ROM exercises, neuromuscular reeducation, and muscle strengthening exercises. Before discharge, patients are instructed on how to manage their pain and swelling with rest, elevation of the limb, or icing of the knee (15 minutes per session and 2-3 times a day) and on home exercises for the knee48-50).
Rehabilitation program examples:
1) First postoperative week: maximum protection phase
Aim: inflammation control, maintenance of active and passive ROM of the knee.
Exercises: weight bearing as tolerated, active closed chain exercises (up to 90° knee flexion), patellar mobilization exercises, straight leg raise exercises, and isometric quadriceps muscle contraction exercises.
2) Second postoperative week: moderate protection phase
Aim: full flexion and extension of the knee.
Exercises: full weight bearing, continuation of previous phase exercises, stretching/flexibility exercises, closed chain exercises (up to 90° knee flexion), resisted lower extremity exercises (open chain exercises such as knee flexion), balance exercises, and proprioception exercises.
3) Third postoperative week: minimum protection phase
Aim: gain normal gait pattern and quadriceps muscle strength of 4/5 on the Lovett scale (movement against resistance or gravity or complete ROM against some resistance).
Exercises: continuation of flexibility exercises and closed chain exercises while avoiding extreme flexion, continuation of resisted lower extremity exercises in weight-bearing position, mini-squats up to 90°, and balance exercises.
4) Sixth postoperative week: return to daily living activities and sports
Aim: maintenance of full muscle strength and maximal function.
Exercises: continuation of muscle strength, function, and proprioception exercises and endurance training, jumping, and light running at 4 weeks postoperatively.
Conclusions
Since Fairbank22) reported on the development of degenerative changes after meniscecotmy in 1948, the clinical efficacy of the procedure has been the subject of controversy. The current consensus is that meniscal tear treatment should be performed with a focus on meniscal function preservation. Studies have shown that degenerative changes after meniscectomy can be prevented or delayed by preserving normal tissue as much as possible with minimal resection of the meniscus. Unfortunately, there are no surgical techniques that can be applied regardless of the type of meniscal tears. It is recommended to choose a method that can be used for various types of meniscal tears, easy and rapid to perform, and allow for the use of delicate equipment. Other factors that should be taken into consideration for meniscectomy include the repairability of the meniscus and the influence of combined ligament injury or articular cartilage damage. In addition, patient's age, health status, life style, level of sports activities, and the location and pattern of the meniscal tear. Therefore, we believe that a meniscectomy would provide good clinical improvement and reduce the risk of degenerative changes when it is performed using an accurate surgical technique for preservation of the remaining meniscus on appropriately selected patients.
References
- 1.Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39:1338–1344. doi: 10.1016/j.injury.2008.06.021. [DOI] [PubMed] [Google Scholar]
- 2.Markolf KL, Mensch JS, Amstutz HC. Stiffness and laxity of the knee--the contributions of the supporting structures. A quantitative in vitro study. J Bone Joint Surg Am. 1976;58:583–594. [PubMed] [Google Scholar]
- 3.Dandy DJ, Jackson RW. The diagnosis of problems after meniscectomy. J Bone Joint Surg Br. 1975;57:349–352. [PubMed] [Google Scholar]
- 4.McMurray TP. The semilunar cartilages. Br J Surg. 1942;29:407–414. [Google Scholar]
- 5.Seedhom BB, Dowson D, Wright V. Proceedings: functions of the menisci. A preliminary study. Ann Rheum Dis. 1974;33:111. doi: 10.1136/ard.33.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Voloshin AS, Wosk J. Shock absorption of meniscectomized and painful knees: a comparative in vivo study. J Biomed Eng. 1983;5:157–161. doi: 10.1016/0141-5425(83)90036-5. [DOI] [PubMed] [Google Scholar]
- 7.Mac CM. The movements of bones and joints; the synovial fluid and its assistants. J Bone Joint Surg Br. 1950;32:244–252. doi: 10.1302/0301-620X.32B2.244. [DOI] [PubMed] [Google Scholar]
- 8.Renstrom P, Johnson RJ. Anatomy and biomechanics of the menisci. Clin Sports Med. 1990;9:523–538. [PubMed] [Google Scholar]
- 9.Zimny ML, Albright DJ, Dabezies E. Mechanoreceptors in the human medial meniscus. Acta Anat (Basel) 1988;133:35–40. doi: 10.1159/000146611. [DOI] [PubMed] [Google Scholar]
- 10.Krause WR, Pope MH, Johnson RJ, Wilder DG. Mechanical changes in the knee after meniscectomy. J Bone Joint Surg Am. 1976;58:599–604. [PubMed] [Google Scholar]
- 11.Ahmed AM, Burke DL. In-vitro measurement of static pressure distribution in synovial joints--Part I: Tibial surface of the knee. J Biomech Eng. 1983;105:216–225. doi: 10.1115/1.3138409. [DOI] [PubMed] [Google Scholar]
- 12.Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002;10:168–176. doi: 10.5435/00124635-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10:90–95. doi: 10.1177/036354658201000205. [DOI] [PubMed] [Google Scholar]
- 14.Brindle T, Nyland J, Johnson DL. The meniscus: review of basic principles with application to surgery and rehabilitation. J Athl Train. 2001;36:160–169. [PMC free article] [PubMed] [Google Scholar]
- 15.Raunest J, Oberle K, Loehnert J, Hoetzinger H. The clinical value of magnetic resonance imaging in the evaluation of meniscal disorders. J Bone Joint Surg Am. 1991;73:11–16. [PubMed] [Google Scholar]
- 16.Shelbourne KD, Dersam MD. Comparison of partial meniscectomy versus meniscus repair for bucket-handle lateral meniscus tears in anterior cruciate ligament reconstructed knees. Arthroscopy. 2004;20:581–585. doi: 10.1016/j.arthro.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 17.Henning CE, Clark JR, Lynch MA, Stallbaumer R, Yearout KM, Vequist SW. Arthroscopic meniscus repair with a posterior incision. Instr Course Lect. 1988;37:209–221. [PubMed] [Google Scholar]
- 18.Bland-Sutton J. Ligaments: their nature and morphology. 2nd ed. London: JK Lewis; 1897. [Google Scholar]
- 19.Perey O. Follow-up results of meniscectomy with regard to the working capacity. Acta Orthop Scand. 1962;32:457–460. doi: 10.3109/17453676208989607. [DOI] [PubMed] [Google Scholar]
- 20.Englund M, Roos EM, Roos HP, Lohmander LS. Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology (Oxford) 2001;40:631–639. doi: 10.1093/rheumatology/40.6.631. [DOI] [PubMed] [Google Scholar]
- 21.King D. The function of the semilunar cartilages. J Bone Joint Surg. 1936;18:1069–1076. [Google Scholar]
- 22.Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:664–670. [PubMed] [Google Scholar]
- 23.Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14:270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 24.Lanzer WL, Komenda G. Changes in articular cartilage after meniscectomy. Clin Orthop Relat Res. 1990;(252):41–48. [PubMed] [Google Scholar]
- 25.Korkala O, Karaharju E, Gronblad M, Aalto K. Articular cartilage after meniscectomy. Rabbit knees studied with the scanning electron microscope. Acta Orthop Scand. 1984;55:273–277. doi: 10.3109/17453678408992355. [DOI] [PubMed] [Google Scholar]
- 26.Tapper EM, Hoover NW. Late results after meniscectomy. J Bone Joint Surg Am. 1969;51:517–526. [PubMed] [Google Scholar]
- 27.Yocum LA, Kerlan RK, Jobe FW, Carter VS, Shields CL, Jr, Lombardo SJ, Collins HR. Isolated lateral meniscectomy. A study of twenty-six patients with isolated tears. J Bone Joint Surg Am. 1979;61:338–342. [PubMed] [Google Scholar]
- 28.Ikeuchi H. Meniscus surgery using the Watanabe arthroscope. Orthop Clin North Am. 1979;10:629–642. [PubMed] [Google Scholar]
- 29.Northmore-Ball MD, Dandy DJ, Jackson RW. Arthroscopic, open partial, and total meniscectomy. A comparative study. J Bone Joint Surg Br. 1983;65:400–404. doi: 10.1302/0301-620X.65B4.6874710. [DOI] [PubMed] [Google Scholar]
- 30.Benedetto KP, Rangger C. Arthroscopic partial meniscectomy: 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1993;1:235–238. doi: 10.1007/BF01560216. [DOI] [PubMed] [Google Scholar]
- 31.McNicholas MJ, Rowley DI, McGurty D, Adalberth T, Abdon P, Lindstrand A, Lohmander LS. Total meniscectomy in adolescence. A thirty-year follow-up. J Bone Joint Surg Br. 2000;82:217–221. [PubMed] [Google Scholar]
- 32.Burks RT, Metcalf MH, Metcalf RW. Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy. 1997;13:673–679. doi: 10.1016/s0749-8063(97)90000-1. [DOI] [PubMed] [Google Scholar]
- 33.Lee SJ, Aadalen KJ, Malaviya P, Lorenz EP, Hayden JK, Farr J, Kang RW, Cole BJ. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006;34:1334–1344. doi: 10.1177/0363546506286786. [DOI] [PubMed] [Google Scholar]
- 34.Jaureguito JW, Elliot JS, Lietner T, Dixon LB, Reider B. The effects of arthroscopic partial lateral meniscectomy in an otherwise normal knee: a retrospective review of functional, clinical, and radiographic results. Arthroscopy. 1995;11:29–36. doi: 10.1016/0749-8063(95)90085-3. [DOI] [PubMed] [Google Scholar]
- 35.Williams RJ, 3rd, Warner KK, Petrigliano FA, Potter HG, Hatch J, Cordasco FA. MRI evaluation of isolated arthroscopic partial meniscectomy patients at a minimum five-year follow-up. HSS J. 2007;3:35–43. doi: 10.1007/s11420-006-9031-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Medlar RC, Mandiberg JJ, Lyne ED. Meniscectomies in children. Report of long-term results (mean, 8.3 years) of 26 children. Am J Sports Med. 1980;8:87–92. doi: 10.1177/036354658000800205. [DOI] [PubMed] [Google Scholar]
- 37.Wroble RR, Henderson RC, Campion ER, el-Khoury GY, Albright JP. Meniscectomy in children and adolescents. A long-term follow-up study. Clin Orthop Relat Res. 1992;(279):180–189. [PubMed] [Google Scholar]
- 38.Appel H. Late results after meniscectomy in the knee joint. A clinical and roentgenologic follow-up investigation. Acta Orthop Scand Suppl. 1970;133:1–111. doi: 10.3109/ort.1970.41.suppl-133.01. [DOI] [PubMed] [Google Scholar]
- 39.Scheller G, Sobau C, Bulow JU. Arthroscopic partial lateral meniscectomy in an otherwise normal knee: Clinical, functional, and radiographic results of a long-term follow-up study. Arthroscopy. 2001;17:946–952. doi: 10.1053/jars.2001.28952. [DOI] [PubMed] [Google Scholar]
- 40.Roos EM, Ostenberg A, Roos H, Ekdahl C, Lohmander LS. Long-term outcome of meniscectomy: symptoms, function, and performance tests in patients with or without radiographic osteoarthritis compared to matched controls. Osteoarthritis Cartilage. 2001;9:316–324. doi: 10.1053/joca.2000.0391. [DOI] [PubMed] [Google Scholar]
- 41.Johnson RJ, Kettelkamp DB, Clark W, Leaverton P. Factors effecting late results after meniscectomy. J Bone Joint Surg Am. 1974;56:719–729. [PubMed] [Google Scholar]
- 42.Jorgensen U, Sonne-Holm S, Lauridsen F, Rosenklint A. Long-term follow-up of meniscectomy in athletes. A prospective longitudinal study. J Bone Joint Surg Br. 1987;69:80–83. doi: 10.1302/0301-620X.69B1.3818740. [DOI] [PubMed] [Google Scholar]
- 43.Ahn J, Lee S. Advanced knee arthroscopy. Seoul: Youngchang; 2009. [Google Scholar]
- 44.Metcalf RW. Operative arthroscopy of the knee. Instr Course Lect. 1981;30:357–396. [PubMed] [Google Scholar]
- 45.Newman AP, Daniels AU, Burks RT. Principles and decision making in meniscal surgery. Arthroscopy. 1993;9:33–51. doi: 10.1016/s0749-8063(05)80342-1. [DOI] [PubMed] [Google Scholar]
- 46.Arnoczky SP, Warren RF, Kaplan N. Meniscal remodeling following partial meniscectomy--an experimental study in the dog. Arthroscopy. 1985;1:247–252. doi: 10.1016/s0749-8063(85)80092-x. [DOI] [PubMed] [Google Scholar]
- 47.Wheatley WB, Krome J, Martin DF. Rehabilitation programmes following arthroscopic meniscectomy in athletes. Sports Med. 1996;21:447–456. doi: 10.2165/00007256-199621060-00006. [DOI] [PubMed] [Google Scholar]
- 48.Vervest AM, Maurer CA, Schambergen TG, de Bie RA, Bulstra SK. Effectiveness of physiotherapy after meniscectomy. Knee Surg Sports Traumatol Arthrosc. 1999;7:360–364. doi: 10.1007/s001670050181. [DOI] [PubMed] [Google Scholar]
- 49.Durand A, Richards CL, Malouin F. Strength recovery and muscle activation of the knee extensor and flexor muscles after arthroscopic meniscectomy. A pilot study. Clin Orthop Relat Res. 1991;(262):210–226. [PubMed] [Google Scholar]
- 50.Zarins B, Boyle J, Harris BA. Knee rehabilitation following arthroscopic meniscectomy. Clin Orthop Relat Res. 1985;(198):36–42. [PubMed] [Google Scholar]