Abstract
Anti-Saccharomyces cerevisiae antibodies (ASCAs) have been proposed as serological markers, which may differentiate Crohn's disease (CD) from ulcerative colitis (UC) and predict disease phenotype. Their importance in pathogenesis is unproven. We investigated the relationship between ASCAs, disease phenotype and NOD2/CARD15 genotype in CD and whether ASCAs were related to antibodies to other fungal proteins. Serum from 228 patients [143 CD, 75 UC, 10 with indeterminate colitis (IC)] and 78 healthy controls (HC) were assayed for ASCA. Antibodies (IgA, IgG) to other fungal proteins (Fusarium species ATC20334, Mycoprotein) were measured in the same samples using an in-house enzyme-linked immunosorbent assay (ELISA) assay. ASCAs were present in 57% of CD, 19% of UC, 30% of IC and 8% of HCs. ASCA-positive status was a predictor for CD with sensitivity of 57%, specificity of 87%, positive predictive value of 78% and negative predictive value of 68%. ASCA was associated with proximal (gastroduodenal and small bowel involvement) rather than purely colonic disease (P < 0·001) and with a more severe disease phenotype and requirement for surgery over a median follow-up time of 9 years (P < 0·0001). No associations with NOD2/CARD15 mutations were seen. There was no association between ASCA and antibodies to MP (IgA or IgG). These data implicate ASCA as a specific marker of disease location and progression in CD, emphasizing the heterogeneity within IBD.
Keywords: ASCA, Crohn's disease, disease behaviour, disease location, NOD2, CARD15
INTRODUCTION
The chronic inflammatory bowel diseases (IBD), Crohn's disease (CD) and ulcerative colitis (UC) are now common causes of gastrointestinal disease in the western world [1]. CD and UC may present with similar symptoms, but differentiation is based on clinical features, anatomical distribution and pathological findings [2]. However, in approximately 10% of cases of colonic IBD, indeterminate colitis (IC) is diagnosed, as clear distinction between UC and CD is not possible [3].
The aetiology of CD is unknown, although both host genetic susceptibility [4] and enteric flora [5] are implicated in the characteristic dysregulation of mucosal immunity. Recently, the NOD2/CARD15 gene [6,7] has been identified as an important determinant of susceptibility to CD. The NOD2/CARD15 protein is expressed in a variety of cell types [8–10] and recent data identified bacterial peptidoglycan as its ligand [11,12]. Three common CD-associated NOD2/CARD15 single nucleotide polymorphism (SNP) variants have been identified in European and North American populations: SNP8 [arginine/tryptophan substitution at position 702 (R702W)]; SNP12 [glycine/arginine substitution at position 908 (G908R)] and SNP13 [a frameshift mutation and terminal Leucine truncation (1007fs)] [13]. A number of less common variants have been described, with clear heterogeneity in the importance of these variants between ethnic groups [14,15]. In our Scottish population of CD patients, we have described a lower allele frequency of NOD2/CARD15 variants than in other cohorts in Europe and North America [16]. There is also heterogeneity within CD in the importance of the NOD2/CARD15 contribution, with associations described between NOD2/CARD15 carriage, early onset disease [14], ileal involvement [17] and stricturing/fistulating disease [18]. Defining genotype–phenotype variation is important, but subclassification of CD has proved a great challenge [19], particularly as the disease behaviour changes with time in a large proportion of patients [20].
Antibodies to several specific antigens have been reported in the sera of patients with IBD. It was hoped that studies of such antibodies would provide either insight into disease pathogenesis and heterogeneity or putative serological markers to adjunct/replace current diagnostic protocols. Great interest has been shown in anti-Saccharomyces cerevisiae antibodies (ASCAs), associated first with CD in the 1980s [21]. These antibodies have a 60–70% prevalence in CD patients compared with 10–15% in UC and 0–5% in healthy control subjects [22–24]. Perinuclear antineutrophil cytoplasmic antibodies (pANCA) have been proposed as a marker for UC, with 60–80% prevalence compared with 10% in CD patients [25,26]. Previous reports have suggested that ASCA and pANCA may be of value in differentiating between UC and CD [22,23,27]. The high specificity (85–97%) of these antibodies has potentially important clinical applications [22–24] but the low sensitivity (50–70%), when used alone, rules out their use as clinical screening tools. The pathogenic significance of these antibodies has not been established and it remains unclear whether they arise due to tissue damage, increased permeability or the mucosal immune perturbation seen in CD.
Existing studies investigating the relationship between ASCA and NOD2/CARD15 status in CD have produced conflicting results [3,18], which may reflect clinical and genetic heterogeneity between patient populations. This study aimed to examine the prevalence of ASCA in a Scottish population of IBD patients and healthy controls and to look for associations between ASCA, disease phenotype and NOD2/CARD15 genotype in CD patients. Antibody responses to a novel mycoprotein antigen (MP) were also studied to evaluate whether a more general underlying defect in tolerance to fungal material is a factor in the immune response to S. cerevisiae.
MATERIALS AND METHODS
Patients and controls
The medicine/oncology subcommittee of the Lothian Research Ethics Committee approved the study protocol. Consecutive consenting patients with a definite diagnosis of IBD were recruited from those attending the IBD clinic at the Western General Hospital, Edinburgh. Diagnoses were defined by standard criteria for CD and UC [2]. Patients with IC were those whose initial diagnosis of IBD could not be confirmed clearly as CD or UC, by clinical, endoscopic or histological methods. Healthy controls (HC) were spouses/friends of IBD patients invited to attend for venepuncture at the same time as patients. None of the controls had IBD. Demographics of the subject groups are given in Table 1. Following informed consent, separate blood samples were collected for NOD2/CARD15 genotyping and for assessment of ASCA and MP in serum at a single time-point. Serum samples were stored at −70°C until analysis. Sera were available for 228 IBD patients and 78 HC. Retrospective data were collected by patient interview and case-note review, which comprised demographic details, ethnicity, family history, smoking status, anatomical distribution and dates of symptom onset, diagnosis and surgery. In addition, for CD patients, disease behaviour at diagnosis and latest follow-up was recorded and changes noted. All data were anonymized and entered into a Microsoft Access© database. CD patients were classed for age at diagnosis, disease location and behaviour at both diagnosis and latest follow-up according to the Vienna classification [28] and are shown in Table 2. Follow-up data were available on 123 CD patients, with a median follow-up of 9 years (range 1 month – 54 years).
Table 1.
Demographic data for CD, UC and IC patients and for healthy controls
| Crohn's disease (n = 143) | Ulcerative colitis (n = 75) | Indeterminate colitis (n = 10) | Healthy controls (n = 78) | P-value | |
|---|---|---|---|---|---|
| Sex | |||||
| Female/male | 79/64 | 34/41 | 7/3 | 39/39 | χ2 = 3·36 n.s. |
| Age at sampling | |||||
| Mean (s.d.) | 42·3 (16·1) | 48·4 (14·1) | 41·1 (15·2) | 41·3 (16·7) | P = 0·006* |
| Range | 17–87 | 24–79 | 23–68 | 20–74 | |
| Age of onset | |||||
| Mean (s.d.) | 28·1 (14·0) | 36·3 (14·4) | 29·5 (15·0) | n.a. | P < 0·001* |
| Range | 5–76 | 16–76 | 9–67 | ||
| Known family history** | |||||
| n | 31 | 16 | 5 | 4 | χ2 = 17·3 |
| (%) | 22% | 21% | 50% | 5% | P = 0·001 |
| Smoking status | |||||
| Current | 32 (22%) | 6 (8%) | 5 (50%) | 16 (20%) | χ2 = 20·7 |
| Ex-smoker | 67 (47%) | 41 (55%) | 2 (20%) | 48 (62%) | P = 0·002 |
| Never | 42 (30%) | 28 (37%) | 3 (30%) | 13 (17%) | |
| Unknown | 2 (1%) | 1 (1%) | |||
n.s.: Not significant.
Significantly higher in UC than all other groups (Kruskal–Wallis test)
some patients were adopted and had no knowledge of birth family.
n.a.: Not applicable.
Table 2.
Vienna classification of CD patients and corresponding ASCA status
| Vienna classification | n (%) | Median ASCA BI | ASCA positive n (%) | P-value‡ |
|---|---|---|---|---|
| Disease location at diagnosis | ||||
| Ileum (L1) | 45 (31) | 1·89 | 31 (68·9) | |
| Colon (L2) | 55 (39) | 0·82 | 21 (38·2) | P = 0·002 |
| Ileocolon (L3) | 21 (15) | 1·33 | 14 (66·7) | |
| Upper GI (L4) | 16 (11) | 1·57 | 13 (81·3) | |
| Perianal only | 2 (1) | 0·94 | 1 (50·0) | |
| Unknown | 4 (3) | |||
| With perianal disease | 42 (29) | 1·34 | 29 (69·1) | P = 0·07 |
| Without perianal disease | 97 (68) | 1·03 | 51 (52·6) | |
| Age at onset/diagnosis | ||||
| Less than 40 years (A1) | 118 (83) | 1·12 | 69 (58·5) | n.s. |
| Over 40 years (A2) | 24 (17) | 1·09 | 13 (54·2) | |
| Unknown | 1 | |||
| Juvenile onset (0–16) | 17 (12) | 1·31 | 13 (76·4) | |
| Early adult onset (17–39) | 102 (71) | 1·09 | 57 (55·9) | n.s. |
| Late adult onset (>40) | 24 (17) | 1·09 | 13 (54·2) | |
| Disease behaviour at diagnosis | ||||
| Inflammatory (B1) | 91 (64) | 0·94 | 42 (46·2) | |
| Stricturing (B2) | 12 (8) | 1·69 | 10 (83·3) | P = 0·003 |
| Penetrating (B3) | 28 (20) | 1·65 | 21 (75·0) | |
| Unknown | 12 (8) | |||
| Change in disease behaviour: diagnosis to latest follow-up | ||||
| Unchanged inflammatory (B1) | 40 (28) | 0·75 | 9 (23·7) | |
| Inflammatory to stricturing (B1–B2) | 16 (11) | 0·98 | 8 (50·0) | P < 0·0001 |
| Inflammatory to penetrating (B1–B3) | 33 (23) | 1·64 | 25 (75·8) | |
| Unknown | 2 | |||
| Need for surgery | ||||
| Yes | 91 (64) | 1·64 | 64 (70·3) | P < 0·0001 |
| No | 52 (36) | 0·79 | 17 (32·7) | |
Details of statistical tests in text. n.s.: Not significant.
ASCA enzyme-linked immunosorbent assay (ELISA) method
The Medizym ASCA Combi kit (Sterilab Sciences, Harrogate, UK) was used to measure ASCA IgG + IgA in patients’ sera, according to the manufacturer's instructions. The optical density (OD) of the developed assay was measured using a spectrophotometric ELISA reader at 405 nm wavelength. Results were interpreted by calculating the binding index (BI) with the formula: BI = ODsample/ODcut-off control. The cut-off control, positive and negative control samples were provided in the kit. A BI of ≥ 1 was considered to be a positive result, <1 was considered to be a negative result.
Mycoprotein antigen preparation and ELISA
Unless stated otherwise, all reagents were from Sigma-Aldrich, Poole, Dorset, UK. Freeze-dried mycoprotein (MP) from the fungus Fusarium species ATCC 20334 (F. graminearum) were supplied by Marlow Foods Ltd. (Stokesley, UK). MP was heated in distilled water for 10–15 min, pepsin (10 µg/ml in 0·1 m HCl) was added and incubated for 1 h at 37°C. The preparation was neutralized with alkali, the supernatant collected for ELISA use and stored at −20°C. The MP supernatant was diluted (1 : 100) in bicarbonate/carbonate buffer, pH 9·6, and 100 µl added to each well of a 96-well high-binding ELISA plate (Greiner) and incubated for 5 h at 22°C. Plates were washed three times in ELISA wash [0·9% saline (Baxter’s), 0·05% Tween 20] and blocked with ELISA wash containing 10 µg/ml human haemoglobin and 1% adult bovine serum. Plates were incubated for 1 h at 37°C and washed again. Serum samples diluted (1 : 100) in ELISA wash containing 1% adult bovine serum, were added to the plates in duplicate against standard and quality control samples, which were selected previously by screening stored sera from patients under investigation at the Gastrointestinal Unit, Western General Hospital, Edinburgh. The standard sample was used to construct a standard curve. Plates were incubated overnight at 4°C. Alkaline phosphatase-conjugated antibody, specific for either IgG or IgA, was diluted in ELISA diluent at 1 : 1000 and incubated at 22°C for 5 h. The assay was developed using p-nitrophenyl phosphate dissolved in diethanolamine buffer and measured by optical density on a spectrophotometric ELISA reader at 405 nm wavelength. Results were calculated from the standard curve.
Statistical analysis
Sensitivity was the probability of a positive ASCA in a patient with CD; specificity was the probability of a negative ASCA in a patient with UC or HC. The positive predictive value (PPV) was the probability of having CD and a positive ASCA. The negative predictive value (NPV) was the probability of having UC or HC and a negative ASCA. The χ2 test was used for analysis of discrete variables. Mann–Whitney and Kruskal–Wallis tests were used to compare the quantitative ASCA BI results between patient groups. Multivariate analysis of ASCA status compared with other variables was carried out using a binary logistic regression analysis. Data were analysed using Minitab™ Statistical Software, version 13·32 (Minitab Inc., PA, USA) or GraphPad Prism® version 4 (GraphPad Software, San Diego, CA, USA) and considered significant at P < 0·05.
RESULTS
ASCA: marker of Crohn's disease?
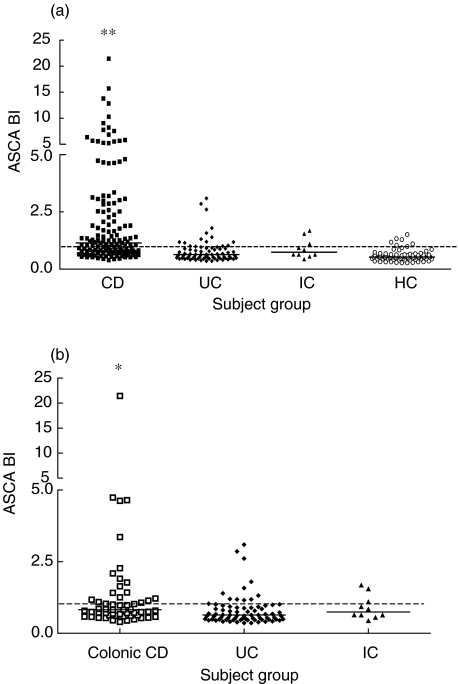
ASCA BI were calculated and individuals defined as ASCA-positive (ASCA+) or -negative (ASCA−). For the CD patients, 81/143 (57%) were ASCA+ compared with 14/75 (19%) UC patients, 3/10 (30%) IC patients and 6/78 (8%) HC (χ2 = 64·7, P < 0·001). The sensitivity of ASCA+ status for CD was 57%, the specificity 87%, PPV was 78% and NPV was 68%. ASCA BI were significantly higher in CD compared with all other groups (Krusal-Wallis, P < 0·0001, Fig. 1a).
Fig. 1.
ASCA as a disease marker. Column scatter plot of ASCA BI of patients in (a) all subject groups and (b) those with colonic CD, UC or IC. Dotted line denotes the ASCA BI cut-off value of 1. All values above the line are ASCA-positive. (a) Median ASCA BI: CD = 1·144, UC = 0·638, IC = 0·743, HC = 0·532. **ASCA BI of CD patients is significantly higher than all other groups (P < 0·001, Kruskal–Wallis). (b) Median ASCA BI: colonic CD = 0·824, UC = 0·638, IC = 0·743. *ASCA BI of colonic CD was significantly higher than that of UC or IC (P = 0·0031, Kruskal–Wallis).
ASCA status was compared between patients with isolated colonic CD and those with UC or IC. ASCA BI of patients with colonic CD were significantly higher than those with UC and IC (Kruskal–Wallis, P = 0·0031, Fig. 1b). There was a significant difference in the number of ASCA+ patients with colonic CD (21/55, 38%), UC (14/75, 18%) or IC (3/10, 30%), χ2 = 6·155, P = 0·046. For the IC patients, one ASCA+ patient was later re-classified as CD, but no other patient had diagnostic features of either CD or UC, so were still classed as IC. The other two ASCA+ IC patients were classed as truly indeterminate or with CD-like disease. For the ASCA− IC, two had CD-like disease, three had UC-like disease and two were truly indeterminate.
No associations were found between ASCA and sex, smoking status, family history or treatment with Infliximab or Azathioprine (data not shown).
ASCA: marker of Crohn's disease location?
ASCA was found to be a marker of proximal CD: 81% with upper GI disease (L4) and 68% of patients with disease involving the ileum (L1 or L3) at diagnosis were ASCA+ compared with 38% of patients with colonic disease (χ2 = 15·2, P = 0·002). ASCA BI of patients with colonic disease (L3) were significantly lower than those with more proximal CD [L1, L2 or L4 (Kruskal–Wallis, P < 0·001)].
Several patients (29%) had concomitant perianal disease. In comparison, patients with perianal disease gave a trend for higher ASCA BI values than those without (Table 2, Mann–Whitney, P = 0·07). An increased proportion of patients with perianal disease were ASCA+ (χ2 = 3·26, P = 0·07).
ASCA: marker of age of onset of Crohn's disease?
No association was found between age of onset of CD and ASCA status using 40 years as the criteria. Further comparison between juvenile onset (<17 years) and early adult onset (17–39 years, Table 2) still gave no significant difference.
ASCA: marker of Crohn's disease behaviour?
Comparison of ASCA BI with behaviour at diagnosis showed that those patients with stricturing (B2) or penetrating (B3) disease had significantly higher ASCA BI than those with inflammatory (B1) disease (Kruskal–Wallis, P = 0·003, Table 2).
Of those patients with inflammatory (B1) disease at diagnosis (n = 91), 40 were B1 at follow-up, while 49 patients had stricturing (B2) or penetrating (B3) disease at follow-up (Table 2). Patients who changed from B1 to B2 or B3 disease between diagnosis and follow-up had higher ASCA BI than those whose disease remained B1 (Kruskal–Wallis, P < 0·0001, Table 2). At diagnosis, 12 patients had stricturing disease and 28 had penetrating disease. At follow-up 4/12 remained with stricturing disease but eight had changed to penetrating disease. There was no significant difference between the ASCA BI of those who had B2 or B3 disease at both diagnosis and follow-up, and those who changed from B2 to B3 (Kruskal–Wallis, P = 0·173, data not shown).
ASCA: marker of genotype?
Genotypic data for the CD patients were available for the three common NOD2/CARD15 gene variants (Table 3a). There were no differences between ASCA+ and ASCA- patients in the number of variants, overall carriage rate or allele frequency. A non-significant trend was seen between carriage of two abnormal copies of the NOD2/CARD15 gene and ASCA positivity (Table 3b, χ2 = 3·285, P = 0·07).
Table 3.
Analyses of ASCA status of CD patients by NOD2/CARD15 genotype
| NOD2/CARD15 genotype* | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Single heterozygous variant | Composite heterozygous variant | Homozygous variant | |||||||
| (a) ASCA status | n | Wild-type | SNP 18 | SNP 12 | SNP 13 | SNPs 12 & 13 | SNPs 8 & 13 | SNPs 8 & 12 | SNP 8 |
| ASCA+ | 81 | 65 | 5 | 2 | 2 | 3 | 0 | 1 | 3 |
| ASCA− | 62 | 43 | 10 | 2 | 6 | 0 | 1 | 0 | 0 |
A multivariate binary logistic regression analysis was performed for ASCA status and the following variables: sex, family history, smoking status, genotype, disease location at diagnosis, age at onset, disease behaviour at diagnosis, disease behaviour at latest follow-up and requirement for surgery. Of these, more severe disease behaviour at latest follow-up was found to be significantly and independently associated with ASCA status when all other factors were taken into account [P = 0·001, odds ratio = 3·21 (95% CI 1·58–6·52)].
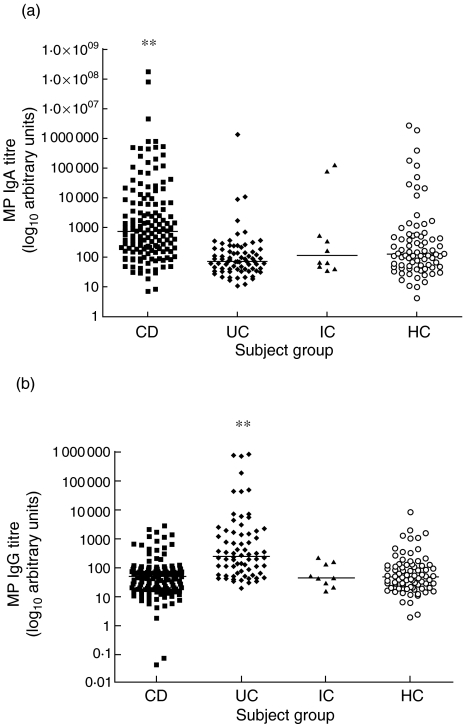
Antibody responses to mycoprotein
The serum titres of both IgA and IgG against the MP antigen were measured and are shown in Fig. 2a,b. CD patients had significantly higher IgA titres than the other subject groups (Kruskal–Wallis, P < 0·0001, Fig. 2a). IgG MP titres were significantly higher in UC patients compared with other subject groups (Kruskal–Wallis, P < 0·0001, Fig. 2b). There was no correlation between ASCA BI levels and MP antibody titres (ASCA versus MP IgA, r = 0·280; ASCA versus MP IgG, r = 0·049). No correlation was found with disease location or phenotype in CD with either MP IgG or IgA, or with other demographic descriptors (data not shown).
Fig. 2.
Antibody titres to mycoprotein. Column scatter graphs of MP antibody titres for IgA (a) and IgG (b) in the different subject groups. Small bars denote median values. Antibody titres are in arbitrary units. (a) Median MP IgA titres: CD = 754, IC = 118, UC = 72·5, HC = 132. **MP IgA titre was significantly higher in CD compared with other subject groups (P < 0·001, Kruskal–Wallis). (b) Median MP IgG titres: CD = 50·4, IC = 44·0, UC = 238, HC = 47·2. **MP IgG titre was significantly higher in UC compared with other subject groups (P < 0·001, Kruskal–Wallis).
DISCUSSION
In the present study we assessed the prevalence of ASCA in a Scottish cohort of IBD patients and healthy subjects and looked for associations with disease phenotype and NOD2/CARD15 genotype in the CD patients. A number of standardized ASCA assays have become commercially available, with differing degrees of specificity and sensitivity, although reconstructed receiver–operator curves have shown good concordance between different assays [29]. Thus our results can be compared directly with other studies, and the differences seen attributed to our population of patients rather than the methodology.
ASCA was found to be specific for CD, but of low sensitivity, which was in concordance with other studies [22–24]. Although ASCA BI levels were higher in patients with colonic CD than those with UC or IC, the considerable overlap between groups indicates that in isolation ASCA is not of great clinical usefulness in distinguishing between these patient groups. The concomitant use of pANCA and other serological markers [30] may aid in more easily differentiating between IC patients [23]. While these assays were not available for this study, it is in IC cases that ASCA/pANCA would perhaps be most useful to differentiate between the UC- or CD-like disease seen, as well as for possible further categorization of CD patients into clinically distinct subgroups, based on the ratio of the ASCA/pANCA levels measured [30,31].
Establishing phenotypic associations of CD subgroups may be important in terms of clinical practice and for the further understanding of disease pathogenesis. ASCA levels were raised in those patients who progressed to a severe disease phenotype and required surgery. In addition, ASCA was found predominantly in those CD patients with more proximal disease as others have shown [22,31–33]. Whereas Vasiliaukas et al. stated that the presence, but not levels of antibodies were associated with disease location [31], in our patients, ASCA BI increased with proximity of disease. Disease location and behaviour are dynamic −changing over time [19,20]. In this study, ASCA status was determined on a single sample for each patient. If indeed, ASCA status is stable over time [34], regardless of disease activity or location, then a high ASCA BI may be indicative of future development of a severe disease phenotype once other contributory factors to ASCA levels have been taken into account, as borne out in the multivariate analysis. A longitudinal study of ASCA levels from diagnosis in patients whose disease behaviour changes would be important in confirming such relationships.
Does the presence of ASCA have a genetic basis? Although we found no relationship with familial CD, others have found associations, where both CD patients and unaffected family members have raised levels of antibodies compared with healthy controls [32,34,35]. These data gave rise to the hypothesis that ASCA may represent a specific, genetically determined breakdown in a mechanism of innate tolerance to yeast or fungal molecular patterns, to which the intestinal epithelium is exposed. Genetic linkage studies have not shown a linkage with the IBD1 locus on chromosome 16 [13]. However, recent data have suggested that not only is there an association between NOD2/CARD15 variants and ASCA, but that the presence of both is synergistic to produce fibrostenosing disease in paediatric CD [36]. In this study no association was found between ASCA and NOD2/CARD15 variant carriage rate or allele frequency. Higher ASCA levels were seen in patients carrying two NOD2/CARD15 variants, but this was not significant and may be due simply to the overall low allele frequency in our patients [16]. Indeed, our data strengthen the evidence for the lack of association of ASCA and NOD2/CARD15 in that, despite a lower allele frequency of NOD2/CARD15 variants, our population has comparable levels of ASCA. Other investigators also failed to find any such association, despite a 35% prevalence of NOD2/CARD15 variants [18]. Similarly, ASCA seropositivity would not appear to be due to the downstream effects of NOD2/CARD15 variants. Both NOD2/CARD15 and ASCAs have been associated with ileal disease [18]; yet, in spite of this mutual association, independent mechanisms of CD pathogenesis must be acting in each case.
Patients with IBD have abnormal responses to food antigens [37,38], suggested to be secondary to inflammation and damage to the integrity of the intestinal wall, causing increased exposure of the immune system to antigenic contents of the bowel lumen [21], including S. cerevisiae antigens in baker's yeast. However, the highly specific association of ASCA with CD is hard to explain as such, and there is no correlation between ASCA and intestinal permeability [34]. Thus the physiological importance of ASCA remains unclear. The presence of IgG ASCA-reactive antigens in the granulomas of bowel resections and on infiltrating lymphocytes and neutrophils in inflamed tissue from CD patients [39], are consistent with antigen specificity (or cross-reactivity) and suggest that S. cerevisiae itself may have some primary pathogenic role in CD. We hypothesized that a defect in immunological tolerance to S. cerevisiae may indicate a global loss of tolerance to fungal antigens, and so antibodies to MP were measured in our study. However, no correlation was found between ASCA and MP antibody titres. Surprisingly, MP IgA titres were higher in CD patients, while MP IgG titres were higher in UC patients. The importance of this observation is unclear; explanations may include differences in intestinal permeability or Th1/Th2 polarization of immune responses occurring in CD and UC.
In a similar way, the antibody class of ASCA may be important. While various studies have measured both IgA and IgG ASCA, their results were given the general term of ASCA+ [31,34,40]. It has been observed that a few patients have only IgG- or IgA–ASCA, but these levels tended to be lower than in those patients who had both antibody classes (possibly indicating a lower antigenic load?) and no association with any clinical grouping has been shown [31]. Therefore, in this study an assay to measure both together was used in our study, although in the light of the MP results this may need to be re-addressed. Oshitani et al. did look at IgG subclasses of ASCAs and found that whereas both IgG1 and IgG3 were additionally raised in Behçet's disease, only IgG4 was increased in both UC and CD patients, possibly as a result of the chronic inflammation that occurs in IBD [41].
While no correlation with MP was seen, in CD other antibodies have been identified against epitopes on bacterial antigens: outer-membrane porin C (OmpC) from Escherichia coli and the bacterial sequence I2 [30]. I2, present in the mucosa of CD patients with active disease, has been associated with Pseudomonas fluorescens[42]. For all these antigens, the actual epitopes to which they are produced have not been elucidated, but it is still possible that specific immunological defects could underlie the variation and severity of disease observed in different patients.
In conclusion, this study has confirmed that ASCA is specific for CD, although in isolation its low sensitivity will limit its use in clinical differentiation between IBDs. ASCA was a marker for proximal CD and for a more severe disease phenotype, but was not associated with NOD2/CARD15 variants in our patient population. No correlation was found between degree of ASCA and MP antibody responses, providing further evidence that the ASCA response may be specific rather than secondary to mucosal injury. Further investigations, including the relationship with other genotypic markers may provide significant steps forward in the understanding of CD, in terms of pathogenesis and in the creation of diagnostic and predictive clinical models.
| (b) ASCA status | n | Homozygous wild-type† | Single heterozygous variant | Composite heterozygous variant | Single homozygous variant | NOD2 variant allele frequency |
|---|---|---|---|---|---|---|
| ASCA+ | 81 | 65 (80%) | 9 (11%) | 4 (5%) | 3 (4%) | 5·4% |
| ASCA− | 62 | 43 (69%) | 18 (29%) | 1 (2%) | 0 | 4·7% |
No. of CD patients with each genotype.
No. (percentage) of CD patients in each genotype group.
Acknowledgments
We wish to acknowledge Sterilab Services, Harrogate for their help in provision of the Medizym ASCA kits.
REFERENCES
- Rubin GP, Hungin AP, Kelly PJ, Ling J. Inflammatory bowel disease: epidemiology and management in an English general practice population. Aliment Pharmacol Ther. 2000;14:1553–9. doi: 10.1046/j.1365-2036.2000.00886.x. [DOI] [PubMed] [Google Scholar]
- Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol. 1989;24(Suppl.):2–6. doi: 10.3109/00365528909091339. [DOI] [PubMed] [Google Scholar]
- Joossens S, Reinisch W, Vermeire S, et al. The value of serologic markers in indeterminate colitis: a prospective follow-up study. Gastroenterology. 2002;122:1242–7. doi: 10.1053/gast.2002.32980. [DOI] [PubMed] [Google Scholar]
- Shanahan F. Crohn's disease. Lancet. 2002;359:62–9. doi: 10.1016/S0140-6736(02)07284-7. [DOI] [PubMed] [Google Scholar]
- Blumberg RS, Saubermann LJ, Strober W. Animal models of mucosal inflammation and their relation to human inflammatory bowel disease. Curr Opin Immunol. 1999;11:648–56. doi: 10.1016/s0952-7915(99)00032-1. [DOI] [PubMed] [Google Scholar]
- Hugot JP, Chamaillard M, Zouali H, et al. Association of NOD2/CARD15 leucine-rich repeat variants with susceptibility to Crohn's disease. Nature. 2001;411:599–603. doi: 10.1038/35079107. [DOI] [PubMed] [Google Scholar]
- Ogura Y, Bonen DK, Inohara N, et al. A frameshift mutation in NOD2/CARD15 associated with susceptibility to Crohn's disease. Nature. 2001;411:603–6. doi: 10.1038/35079114. [DOI] [PubMed] [Google Scholar]
- Ogura Y, Inohara N, Benito A, Chen FF, Yamaoka S, Nunez G. Nod2, a Nod1/Apaf-1 family member that is restricted to monocytes and activates NF-kappaB. J Biol Chem. 2001;276:4812–8. doi: 10.1074/jbc.M008072200. [DOI] [PubMed] [Google Scholar]
- Rosenstiel P, Fantini M, Brautigam K, et al. TNF-alpha and IFN-gamma regulate the expression of the NOD2 (CARD15) gene in human intestinal epithelial cells. Gastroenterology. 2003;124:1001–9. doi: 10.1053/gast.2003.50157. [DOI] [PubMed] [Google Scholar]
- Gutierrez O, Pipaon C, Inohara N, et al. Induction of Nod2 in myelomonocytic and intestinal epithelial cells via nuclear factor-kappa B activation. J Biol Chem. 2002;277:41701–5. doi: 10.1074/jbc.M206473200. [DOI] [PubMed] [Google Scholar]
- Girardin SE, Boneca IG, Viala J, et al. NOD2/CARD15 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection. J Biol Chem. 2003;278:8869–72. doi: 10.1074/jbc.C200651200. [DOI] [PubMed] [Google Scholar]
- Bonen DK, Ogura Y, Nicolae DL, et al. Crohn's disease-associated NOD2/CARD15 variants share a signaling defect in response to lipopolysaccharide and peptidoglycan. Gastroenterology. 2003;124:140–6. doi: 10.1053/gast.2003.50019. [DOI] [PubMed] [Google Scholar]
- Watts DA, Satsangi J. The genetic jigsaw of inflammatory bowel disease. Gut. 2002;50(Suppl. 3):III31–6. doi: 10.1136/gut.50.suppl_3.iii31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesage S, Zouali H, Cezard JP, et al. CARD15/NOD2/CARD15 mutational analysis and genotype–phenotype correlation in 612 patients with inflammatory bowel disease. Am J Hum Genet. 2002;70:845–57. doi: 10.1086/339432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugimura K, Taylor KD, Lin YC, et al. A novel NOD2/CARD15 haplotype conferring risk for Crohn disease in Ashkenazi Jews. Am J Hum Genet. 2003;72:509–18. doi: 10.1086/367848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crichton DN, Arnott IDR, Watts D, et al. NOD2/CARD15 mutations in a Scottish Crohn's disease population. Gastroenterology. 2002;122(Suppl.):M1420. [Google Scholar]
- Ahmad T, Armuzzi A, Bunce M, et al. The molecular classification of the clinical manifestations of Crohn's disease. Gastroenterology. 2002;122:854–66. doi: 10.1053/gast.2002.32413. [DOI] [PubMed] [Google Scholar]
- Abreu MT, Taylor KD, Lin Y-C, et al. Mutations in NOD2/CARD15 are associated with fibrostenosing disease in patients with Crohn's disease. Gastroenterology. 2002;123:679–88. doi: 10.1053/gast.2002.35393. [DOI] [PubMed] [Google Scholar]
- Arnott ID, Satsangi J. Crohn's disease or Crohn's diseases? Gut. 2003;52:460–1. doi: 10.1136/gut.52.4.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louis E, Michel V, Hugot JP, et al. Early development of stricturing or penetrating pattern in Crohn's disease is influenced by disease location, number of flares, and smoking but not by NOD2/CARD15 genotype. Gut. 2003;52:552–7. doi: 10.1136/gut.52.4.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main J, McKenzie H, Yeaman GR, et al. Antibody to Saccharomyces cerevisiae (bakers’ yeast) in Crohn's disease. Br Med J. 1988;297:1105–6. doi: 10.1136/bmj.297.6656.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinton JF, Sendid B, Reumaux D, et al. Anti-Saccharomyces cerevisiae mannan antibodies combined with antineutrophil cytoplasmic autoantibodies in inflammatory bowel disease: prevalence and diagnostic role. Gut. 1998;42:788–91. doi: 10.1136/gut.42.6.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters M, Joossens S, Vermeire S, Vlietinck R, Bossuyt X, Rutgeerts P. Diagnostic value of anti-Saccharomyces cerevisiae and antineutrophil cytoplasmic autoantibodies in inflammatory bowel disease. Am J Gastroenterol. 2001;96:730–4. doi: 10.1111/j.1572-0241.2001.03613.x. [DOI] [PubMed] [Google Scholar]
- Ruemmele FM, Targan SR, Levy G, Dubinsky M, Braun J, Seidman EG. Diagnostic accuracy of serological assays in pediatric inflammatory bowel disease. Gastroenterology. 1998;115:822–9. doi: 10.1016/s0016-5085(98)70252-5. [DOI] [PubMed] [Google Scholar]
- Satsangi J, Landers CJ, Welsh KI, Koss K, Targan S, Jewell DP. The presence of anti-neutrophil antibodies reflects clinical and genetic heterogeneity within inflammatory bowel disease. Inflamm Bowel Dis. 1998;4:18–26. doi: 10.1097/00054725-199802000-00004. [DOI] [PubMed] [Google Scholar]
- Seibold F, Weber P, Schoning A, Mork H, Goppel S, Scheurlen M. Neutrophil antibodies (pANCA) in chronic liver disease and inflammatory bowel disease: do they react with different antigens? Eur J Gastroenterol Hepatol. 1996;8:1095–100. doi: 10.1097/00042737-199611000-00012. [DOI] [PubMed] [Google Scholar]
- Rutgeerts P, Vermeire S. Serological diagnosis of inflammatory bowel disease. Lancet. 2000;356:2117–8. doi: 10.1016/s0140-6736(00)03488-7. [DOI] [PubMed] [Google Scholar]
- Gasche C, Scholmerich J, Brynskov J, et al. A simple classification of Crohn's disease. Inflamm Bowel Dis. 2000;6:8–15. doi: 10.1097/00054725-200002000-00002. Report of the Working Party of the World Congress of Gastroenterology, Vienna 1998. [DOI] [PubMed] [Google Scholar]
- Vermeire S, Joossens S, Peeters M, et al. Comparative study of ASCA (anti-Saccharomyces cerevisiae antibody) assays in inflammatory bowel disease. Gastroenterology. 2001;120:827–33. doi: 10.1053/gast.2001.22546. [DOI] [PubMed] [Google Scholar]
- Landers CJ, Cohavy O, Misra R, Yang H, Lin YC, Braun J, Targan SR. Selected loss of tolerance evidenced by Crohn's disease-associated immune responses to auto- and microbial antigens. Gastroenterology. 2002;123:689–99. doi: 10.1053/gast.2002.35379. [DOI] [PubMed] [Google Scholar]
- Vasiliauskas EA, Kam LY, Karp LC, Gaiennie J, Yang H, Targan SR. Marker antibody expression stratifies Crohn's disease into immunologically homogeneous subgroups with distinct clinical characteristics. Gut. 2000;47:487–96. doi: 10.1136/gut.47.4.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annese V, Andreoli A, Andriulli A, et al. Familial expression of anti-Saccharomyces cerevisiae mannan antibodies in Crohn's disease and ulcerative colitis: a GISC study. Am J Gastroenterol. 2001;96:2407–12. doi: 10.1111/j.1572-0241.2001.04043.x. [DOI] [PubMed] [Google Scholar]
- Bernstein CN, Orr K, Blanchard JF, Sargent M, Workman D. Development of an assay for antibodies to Saccharomyces cerevisiae: easy, cheap and specific for Crohn's disease. Can J Gastroenterol. 2001;15:499–504. doi: 10.1155/2001/605470. [DOI] [PubMed] [Google Scholar]
- Vermeire S, Peeters M, Vlietinck R, et al. Anti-Saccharomyces cerevisiae antibodies (ASCA), phenotypes of IBD, and intestinal permeability: a study in IBD families. Inflamm Bowel Dis. 2001;7:8–15. doi: 10.1097/00054725-200102000-00002. [DOI] [PubMed] [Google Scholar]
- Sutton CL, Yang H, Li Z, Rotter JI, Targan SR, Braun J. Familial expression of anti-Saccharomyces cerevisiae mannan antibodies in affected and unaffected relatives of patients with Crohn's disease. Gut. 2000;46:58–63. doi: 10.1136/gut.46.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubinsky MC, Lee-Uy N, Lin Y-C, et al. Synergism of NOD2/CARD15 and ASCA (anti-Saccharomyces cerevisiae antibodies) contributes to disease behavior in pediatric Crohn's disease (CD) patients. Gastroenterology. 2003;124(Suppl.):M1556. [Google Scholar]
- Paganelli R, Pallone F, Montano S, et al. Isotypic analysis of antibody response to a food antigen in inflammatory bowel disease. Int Arch Allergy Appl Immunol. 1985;78:81–5. doi: 10.1159/000233867. [DOI] [PubMed] [Google Scholar]
- Knoflach P, Park BH, Cunningham R, Weiser MM, Albini B. Serum antibodies to cow's milk proteins in ulcerative colitis and Crohn's disease. Gastroenterology. 1987;92:479–85. doi: 10.1016/0016-5085(87)90145-4. [DOI] [PubMed] [Google Scholar]
- Oshitani N, Hato F, Suzuki K, et al. Cross-reactivity of yeast antigens in human colon and peripheral leukocytes. J Pathol. 2003;199:361–7. doi: 10.1002/path.1276. [DOI] [PubMed] [Google Scholar]
- Sandborn WJ, Loftus EV, Jr, Colombel J-F, et al. Evaluation of serologic disease markers in a population-based cohort of patients with ulcerative colitis and Crohn's disease. Inflamm Bowel Dis. 2001;7:192–201. doi: 10.1097/00054725-200108000-00003. [DOI] [PubMed] [Google Scholar]
- Oshitani N, Hato F, Jinno Y, et al. IgG sub-classes of anti-Saccharomyces cerevisiae antibody in inflammatory bowel disease. Eur J Clin Invest. 2001;31:221–5. doi: 10.1046/j.1365-2362.2001.00798.x. [DOI] [PubMed] [Google Scholar]
- Wei B, Huang T, Dalwadi H, Sutton CL, Bruckner D, Braun J. Pseudomonas fluorescens encodes the Crohn's disease-associated I2 sequence and T-cell superantigen. Infect Immun. 2002;70:6567–75. doi: 10.1128/IAI.70.12.6567-6575.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]