Abstract
The objective of this paper is to describe the recent history, current situation and perspectives for further development of the integrated system of primary care in the Czech Republic. The role of primary care in the whole health care system is discussed and new initiatives aimed at strengthening and integrating primary care are outlined. Changes brought about by the recent reform processes are generally seen as favourable, however, a lack of integration of health services under the current system is causing various kinds of problems. A new strategy for development of primary care in the Czech Republic encourages integration of care and defines primary care as co-ordinated and complex care provided at the level of the first contact of an individual with the health care system.
Keywords: primary health care, integrated care, Czech Republic
Introduction
In the Czech Republic, the context in which health care is being delivered has changed dramatically over recent years. The introduction of major health and political reforms, characterised by expansion of market economy, privatisation of government services, and democratisation and decentralisation, has created a turbulent and uncertain environment for the development and management of health services. Issues of efficiency, cost-containment, consumer choice and accountability are in the forefront. Despite the concerns with improving the performance of health systems, until recently, a number of important issues, particularly equity and integrated delivery of health care, remained largely neglected [1].
The objective of this paper is to describe the recent history, current situation and perspectives for further development of the integrated system of primary care in the Czech Republic. The role of primary care in the whole health care system is discussed and new initiatives aimed at strengthening and integrating primary care are outlined.
The issues of primary care are attracting growing interest among international agencies and similar bodies and becoming part of preparatory activities related to the process of accession to the European Union. In our review, we were able to draw on critical analyses of the Czech health care system and evaluations of its recent reforms performed as a part international collaborative projects funded by the World Health Organisation, the Organisation for Economic Co-operation and Development, and the European Union's PHARE Programme. We also conducted searches of medical bibliographic databases and contacted subjects involved in administration of primary care and organisation of health care. Information from both formal and informal sources was used in producing this paper.
The demographic and political situation in the Czech Republic
Before discussing the specific issues of primary care in the Czech Republic, it is useful to outline the political context, in which the reforms of health care provision are taking place, and to summarise the current situation with respect to the health status of the Czech population. The process of democratisation in the former Czechoslovakia began in 1989, leading to democratic elections in 1990. A legal separation of the Czech and Slovak Republics took place in 1992, leading to the establishment of the Czech Republic on 1 January 1993. The Czech Republic has been a member of the Organisation for Economic Co-operation and Development (OECD) since 1995 and a member of the North Atlantic Treaty Organisation (NATO) since 1999. Currently, the main priority is to gain membership of the European Union.
Czech Republic is one of the healthiest of the central and eastern European countries and one of the few where the process of transition led to substantial reduction of mortality rates. Infant mortality (5.2 per 1000 live births in 1998) and life expectancy (71.1 years for men and 78.1 years for women in 1998) are better than in most CEE countries but worse than in Western Europe [2]. See Table 1.
Table 1.
Basic demographic and health status indicators: Czech Republic, 1985–1998
| Indicator | 1985 | 1990 | 1995 | 1998 | |
|---|---|---|---|---|---|
| Live births | Number Per 1000 |
135,881 13.1 |
130,564 12.6 |
96,097 9.3 |
90,535 8.8 |
| Deaths under 1 year of age | Number Per 1000 |
1,694 12.5 |
1,410 10.8 |
740 7.7 |
472 5.2 |
| Life expectancy at birth (in years) | Males Females |
67.5 74.7 |
67.6 75.4 |
69.7 76.6 |
71.1 78.1 |
In 1994, for the first time since 1918, the number of deaths exceeded the number of births by around 10,000. This trend has continued and the population is currently falling by around 1/1000 per year. The population is expected to continue to decline, whilst the number of people above 65 years of age (14% in 1999) will rise [2].
Health care and policy in the Czech Republic
The transition toward the market economy after 1989 has been accompanied by a series of fundamental changes in the Czech health care system. The main features of the changing health system included introduction of free choice of a GP, direct access to specialists and specialist departments, and an emergence of private health sector. Patients are allowed to register with a new GP every six months without giving a reason for that (in addition to the necessity to re-register when moving house etc.) and there is virtually no restriction on access to specialists. This is still considered by many to be one of the most valued “liberties” achieved during the transition but is also acknowledged as an important issue in terms of cost and quality of care.
The efforts to encourage competition and free-market reform in the Czech Republic have been described as one of the most aggressive of the former Warsaw Pact countries. In 1990 and 1991, a dramatic liberalisation of the health care system took place. The principle of free choice of health care facility was implemented. Former regional and district health authorities were broken down. In 1991, new laws were approved, especially the General Health Insurance Law and the Law on the General Insurance Fund. Since then, the health care system has moved towards a compulsory insurance model, with a number of insurers financing health care providers on the basis of contracts [2]. In 1992, a mandatory employment-based health insurance system was introduced. The move from a controlled socialist structure to an insurance-based, fee-for-service model occurred in a very short time [3]. The role of state in relation to health services has remained one of the most controversial issues throughout the reform process [4].
To date, the reform of the health care system does not appear to have caused any adverse effects to the health status of the population. For the most part, indicators are showing positive trends [2]. There are, however, some indications of regional differences in the level of improvements in health care after 1989 [5].
History of primary care in the Czech Republic
A systematic and comprehensive analysis of the development of primary care in the Czech Republic until 1997 was performed within the framework of a PHARE project by a panel of Czech and foreign experts [6]. Before the Second World War, services provided by private and family doctors were funded mainly by health insurance companies in the form of capitation payments. The socialisation of health care after the war led to establishing health care centres and polyclinics that were part of the regional “Institutes of National Health” [7]. Enormous separation of specialised activities from activities of the so-called district and company doctors, deterioration of their status as physicians and sometimes the distance between the facilities and places of residence are the most commonly acknowledged problems of the socialist system of primary care [6]. The low attractiveness of the work of general practitioners used to be perceived as a particular problem and never satisfactorily resolved [8].
Health care reforms in the last decade led to fundamental structural changes in Czech primary care. Primary care was the first area considerably affected by “privatisation”. It is believed that the possibility to operate as independent (private) providers has increased the attractiveness of general practice to some extent. GPs have succeeded in becoming an organised professional group able to defend their professional interests through scientific and professional societies and their increasing role is also reflected in the field of medical education. Departments of general practice or family medicine have been established at all Czech medical schools and training in these disciplines is now a part of undergraduate medical curricula [9].
Decades of deepened specialisation fixed the division between specialists and general practitioners in the outpatient sphere. For instance when the fee for services system was introduced during the early stages of health care reform, the average income of primary care physicians was much lower than incomes of outpatient specialists. This was largely because of the low cost of human work still inherent in the overall price lists that served as a basis for funding and possibly also because of the lack of technical equipment [6].
Current situation
Providers
The full range of primary health care services currently provided in the Czech Republic includes general medical care, maternal and child health, gynaecology, dentistry/stomatology, home care by nurses, 24-hour emergency cover and a number of preventive services such as immunisation or screenings. There is also open access to some specialists, e.g. psychiatrists, venereologists and dermatologists. There are no restrictions on patients' choice of primary health care physician [2].
Primary health care is organised at district level. The district health office is responsible for ensuring that their area has accessible primary health care services. Citizens register with a primary care physician of their choice and can reregister with a new physician every six months. There are four first-contact doctors in the Czech health care system: general practitioners for adults, general practitioners for children and youth (paediatricians), ambulatory gynaecologists and dentist/stomatologists.
In 1999, there were about 4800 GPs for adults, 2250 GPs for children and youth, 480 home care agencies, 6200 stomatologists and 1255 ambulatory gynaecologists [9]. In the late 1990s, about 70–80% of all outpatient treatments and examinations were provided in private facilities [6]. The development of home care agencies is a relatively recent phenomenon in the Czech Republic [10].
The average number of inhabitants per a primary care physician in 1994 and 1998 is given in Table 2.
Table 2.
The average number of inhabitants per a primary care physician in 1994 and 1998
| Population per doctor in primary care | 1994 | 1998 |
|---|---|---|
| 1 GP for adults | 1670 | 1780 |
| 1 GP for children and youth | 1150 | 1170 |
| 1 stomatologist | 1760 | 1770 |
| 1 ambulatory gynaecologist | 4840 | 4890 |
Source: European Observatory on health care Systems, 1999.
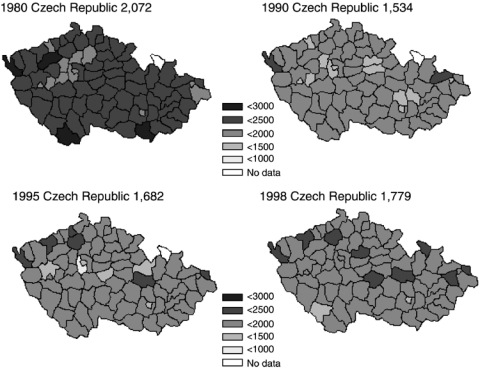
A slight increase in the average number of adults cared for by one general practitioner can be seen. There are, however, considerable geographical differences in the number of population per doctor [11], the ratio being lowest in the capital Prague. See Figure 1.
Figure 1.
Number of persons older than 14 years per 1 GP for adults in districts of the Czech Republic in 1980, 1990, 1995, and 1998. (Source: DPS-99 UZIS CR).
The entry of doctors into primary health care practice is controlled through licensing by the Medical Chamber and the issuing of permits by the district health office. Doctors then contract with health insurance funds. The private practices are managed differently depending on the local situation. A group of primary health care physicians may work together in health centres: these are polyclinics that provide primary health care. The centres are owned by the local community (municipality) and run by a director. Primary health care physicians who are in private practice pay a rent for using the facilities of the centres that tend to be relatively high. The rest of primary health care physicians work alone [2].
Since 1981, physicians have to complete the first level of postgraduate specialisation before they enter general practice (which takes thirty months). Further specialisation after the first level is optional and usually takes between 3 and 5 years [2]. Women represent two thirds of the total number of general practitioners. Most general practitioners belong to the age group of 40–70 years [6].
Zavazalova et al. studied attitudes and satisfaction with their job among 68 general practitioners [12]. All respondents reported that they systematically extended their education and training and 97% of them were keen to master and use new procedures. One third of the respondents were satisfied with their job. On average, they worked 50 hours per week and examined 236 patients per week in their surgery.
The possibility of a free choice of a GP introduced during the reform process, led to the transfer of approximately 30% of the GP clientele, especially in urban areas. The majority of GPs work independently, employing a nurse who also does administrative work and often home visits as well. At the moment, there is little motivation to establish group practices or horizontal contracts among the GPs.
Contents of primary care and services provided by GPs
As to the effective legal order of the Czech Republic the term of primary care is not specified by any legal regulation related to health care. The contents and forms of primary care or the position of primary care providers and their competencies are not officially determined. The fundamental legal regulation determining health care provision in the Czech Republic, the Act No 20/1966 Coll., on Care of Public Health as amended, stipulates individual types of health care and conditions of their implementations. The traditional division of care into outpatient, inpatient, balneologic, company health care etc. still persists [6].
The range of activities GPs are allowed to perform results from regular negotiations between the General Health Insurance Fund and the Czech Medical Chamber [13]. The OECD study team also reported that “…patients have no motivation for rational judgement about the real necessity of their visits to a physician. A number of visits are merely for administrative reasons … and the high number of contacts leads consequently to the higher quantity of prescriptions and higher number of referrals.”
Based on data from a study of primary care in 29 European countries published by NIVEL in the early 1990s, the range of services that Czech GPs provide is considerably narrower and makes up only 30–60% of the services offered by their Western counterparts. For instance, small surgical interventions, otorhinolaryngological or ophthalmological treatments are not commonly performed by GPs in the Czech Republic [13]. This is believed to be partly due to the fact that Czech GPs generally do not have the same level of access to technical equipment (X-ray, ultrasound or modern laboratory devices) as their European counterparts.
A recent review of the Czech health care system (so-called HiT report) [2], concluded that health centres providing primary care tend to be well resourced, most have electrocardiograms, ultrasound and often X-ray equipment. They also have some diagnostic laboratory facilities and employ nurses and physiotherapists. The authors, however, acknowledge that primary health care doctors who work alone usually have immediate access to fewer facilities. In accord with other reviews, the authors also emphasise that a large part of the work of primary care physicians involves certification of absences from work and referral rates to specialists are high. Recent introduction of financial incentives for primary health care physicians to take on more tasks might have resulted into some providing more specialised services to their patients.
GPs and specialists, lack of integration
Direct access to specialists is based on the Act No. 216/1992 Coll., stipulating the Health Rules for provision and reimbursement of health care services in terms of general health insurance [6], and is often perceived by the general public as one of the major improvements resulting from the reform.
Drbal studied the relations between specialists providing care in outpatient departments of hospitals and general practitioners [14]. The results are based on a questionnaire survey among 101 general practitioners and 141 specialists and other health care workers (head physicians, managers etc.). The data suggest that 80% of specialists felt that they were sometimes or often providing services that could be performed by a GP. They believed this was largely because their patients did not have sufficient trust in the quality of care provided by their GP.
The current system of financing is believed to encourage physicians to perform many unnecessary examinations and interventions and leads to multiple examinations of the same patient by several physicians without any co-ordination or information sharing. Apart from the obvious issues of wasting of scarce resources, these multiple tests are often invasive and uncomfortable for the patient (blood tests, endoscopy) and sometimes clearly harmful (unnecessary X-rays, interactions with multiple drug treatments) [15].
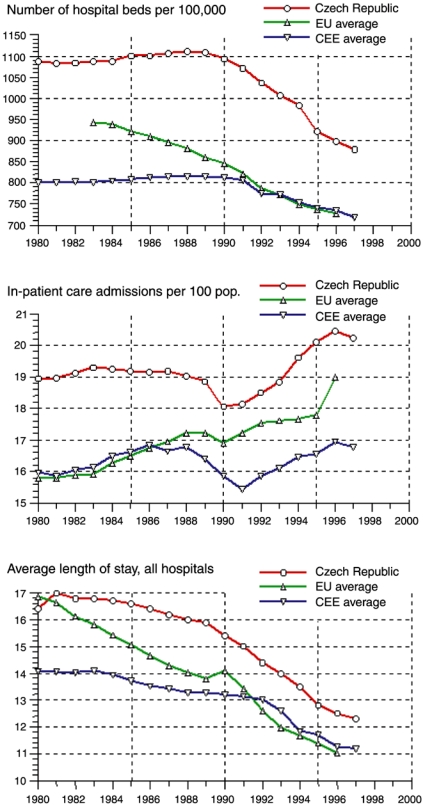
In 1998, Papes reported that there are about 2 million hospitalisations and 155 million visits to ambulatory care per year in the Czech Republic (which has a population of 10 million) [16]. The number of hospital beds in the Czech Republic is still considerably greater than in many countries of Western Europe or other Central and Eastern European countries. Most of the hospital beds in the Czech Republic are acute beds (more than 75%). The number of hospital admissions in the Czech Republic showed a marked increase in the early 1990s, a trend that only reversed in 1997. Given the frequency of hospital admissions, the average length of stay in both acute and non-acute care hospitals in the Czech Republic is also extremely high. See Figure 2.
Figure 2.
Indicators of hospital care in the Czech Republic, Central and Eastern Europe (CEE) and the European Union (EU). Source: WHO HFA.
Hrobon et al. used the Appropriateness Evaluation Protocol (AEP) to assess appropriateness of admission and continuing hospitalisation of 260 patients admitted consecutively to department of internal medicine of a teaching hospital [17]. Twenty-four percent of the total of 260 admissions and 54% of 1869 evaluated days of stay failed the AEP criteria in that the patients could be well served by lower treatment intensity in outpatient clinics, nursery homes or their own homes. Results of a similar study performed at a department of surgery indicated that 8% of the admissions and 27% of days of stay were probably unnecessary [18].
This trend is in clear contrast with recent developments in, e.g. UK where providers are stimulated to bring services to patients rather than send patients to hospital and general practitioners are encouraged to further delegate work that does not require a doctor [19].
Main issues to be addressed
Major problems related to the primary care position in the current health care system identified within the most comprehensive analysis so far were:
Way of funding that prompts physicians to enrol a large number of patients and to organise many examinations and visits.
Narrow scope of provided diagnostic and therapeutic procedures, frequent referrals to specialist and to hospitals even in cases that could be treated by the general practitioner.
Generally low standard of technical equipment.
Lack of complex information about the patient and legislation that does not specify the obligation of health care professionals to inform the general practitioner about extraordinary interventions required in acute conditions or procedures in chronic conditions.
Direct access to all specialists based on the vaguely formulated legislation with many exceptions.
Formal demands on education and practice before granting the approval to open the practice [6].
According to the reform proposals from the 1990s, integrated primary care should constitute the basis of the new system. However, some argue that this emphasis on primary health care has been more declaratory than actual [13]. The need to enhance the role of the GPs in the health care system has been proclaimed since the beginning of transformation of the Czech health care system after 1989, however, little has been done in terms of creating the necessary conditions or regulating the costs of services provided. In 1997, Meijerman et al. concluded that
“… no conditions to enhance the general practitioner position and to create a fully integrated system of health-social care … have been established. Therefore, primary care represents a weak, neglected and legislatively unspecified part of the health care system” [6].
The incentives offered by the original reimbursement system favoured high levels of activity and little co-operation. The lack of an efficient gate-keeping system at primary health care level and the presence of large numbers of ambulatory-based specialists encouraged overuse of specialists rather than generalists.
The HiT report concluded that many of current problems in the Czech health care system are caused by a lack of integration [2]. Sufficient levels of communication are still missing, partial solutions and improvisations are often adopted and group interests prevail over the national ones. The authors argue that the Czech health care system has become more democratic, but still not fully humanistic.
Perspectives and challenges for integrated primary health care in the Czech Republic
The new official strategy for development of primary care in the Czech Republic defines primary care as co-ordinated and complex care provided at the level of the first contact of an individual with the health care system and on the basis of a long-term continual approach to the individual [15]. Primary care is seen as a set of activities provided by health care professionals in the field of health promotion, prevention, diagnostics, treatment, rehabilitation and care. These activities are to be performed, as close to the patients' social environment as possible and respect their bio-psycho-social needs. Primary care should be accessible twenty-four hours a day, seven days a week and related to other parts of the health care system (secondary and tertiary care).
In the proposed strategy for development of primary, three specific stages are distinguished:
Strengthening of the role of primary care in the whole system of health care.
Strengthening of the role of primary care as a co-ordinator of health care (including the role of general practitioner as a gate-keeper and co-ordinator of treatment strategy for individual patients).
Strengthening of the integration of health and social care [15].
The strategy assumes that all current providers of primary care will be involved in providing primary care services under the new model, i.e. the main providers will consist of general practitioners for adults and general practitioners for children and youth. Gynaecologists and dentists/stomatologists will remain a part of the system of primary care. Other primary care services will include health and pharmaceutical emergency services [15]. Most recent materials distributed by the Association for Home Care in the Czech Republic (PHARE) also emphasise the role of family, friends, neighbours, emergency lines and self-care in providing comprehensive primary care.
The family doctor/general practitioner position is being established as another type of a physician providing health care for all age categories, and therefore such a physician will be able to provide health care for all registered family members. It is assumed that the introduction of family doctors/general practitioners will depend on demographic and economic factors and that there may be higher preference for both types of existing GPs in regions with no need of the care integration (such as large agglomerations). However, it is assumed that the old and new types of general practitioners will co-exist and the number of family doctors will gradually increase [15].
A number of solutions has been proposed to reverse the current overuse of specialist care: gate-keeping system at primary health care level, changing the reimbursement systems for primary health care doctors, DRG payments for hospitals, and reductions in physician numbers and hospital beds [2].
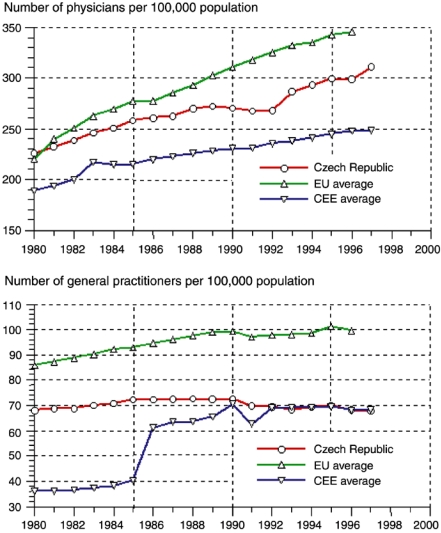
A review of country experiences of integrated health services by the WHO Study Group concluded that integrated health services are cost-effective, integration is easier at lower level and savings can be achieved by hiring one multipurpose health worker instead of several single-purpose workers [1]. The latter may prove problematic in a setting where the number of health care workers, particularly physicians, is relatively high. See Figure 3.
Figure 3.
Number of physicians and general practitioners per 100,000 population in the Czech Republic, Central and Eastern Europe (CEE) and the European Union (EU). Source: WHO HFA.
The existing surplus of specialists is intended to be reduced by retraining specialists to work in other specialities such as public health or general practice. This is planned, but has not yet been fully implemented [2]. From the point of view of human resources, one might indeed give priority to ensuring integration of services provided by existing specialists rather than to immediate and radical replacement of relatively well trained specialists by new generalist-type health workers.
One of the main unresolved issues concerns the development and implementation of a system of ongoing monitoring and evaluation in primary care. The problem is not restricted to the specific issues of primary care or aspects of integration of services that are currently provided. Lack of analytical capacity and a tendency for decision making to be based on political preferences or strongly held beliefs of individual policy makers seem to be a general characteristic of the Czech health care system. There is little tradition of health needs assessment, thorough analyses of effectiveness and quality of particular interventions or indeed of reform processes and organisational changes as such. Moreover, owning information is still considered a source of power and this makes the task of information analysis very difficult [20]. In the absence of any concrete data that would allow to compare the results of different strategies that were implemented in the Czech Republic over the recent years, it is very difficult to draw any firm conclusions about the advantages of certain strategies or attempt any predictions about the success of the new strategy to be implemented.
As apparent from the above-mentioned srategy for the development of integrated primary care in the Czech Republic, an important role of GPs (and the new family doctors) as gate-keepers and co-ordinators is envisaged in the new system. It is, however, not clear, how far this can function under the current system of financing and under the pressure of the various financial and other incentives inherent in the overall system of health care organisation and financing. Moreover, the prevalent atmosphere, when people find ideas such as strategic planning or regulation largely unacceptable and tend to perceive them as part of the old discredited control system, does not seem conducive to introduction of more regulation in a form of gate-keeping or other.
There is currently considerable interest in looking to Western Europe for inspiration and a certain degree of willingness to implement, what is usually described as, the European model of health care. The context of the situation in the Czech Republic, traditions with respect to social organisation and attitudes to health and health issues, and also the economic situation of the country, will all play an important role and pose many specific issues when trying to implement new concepts such as a family doctor. It remains to be seen how far these new concepts are effective and viable in the context of the Czech Republic.
Conclusion
Recent major reforms of the Czech health care system led to a great degree of decentralisation and disintegration of the former system. The changes brought about by the reform processes are generally seen as favourable, however, a lack of integration of health services under the current system is causing various kinds of problems. We believe that a promising way to solve the current problems lies in adopting a systemic approach to the administration of the whole health care system and in introduction of systemic measures that promote integration of the relatively isolated health and social services at all levels. In this context, integrated care should be seen not only as a managerial tool but also, and more importantly, as a method of better satisfaction of health needs of the sick individuals as well as the whole population. The success of the new strategies is uncertain, unless they are accompanied by a meaningful system of monitoring and evaluation.
Acknowledgments
We would like to thank Dr Alena Steflova of the Czech Ministry of Health for providing us with most useful information. The work on this review was partly supported by the Internal Grant Agency of the Czech Ministry of Health (contract NO6160-3/2000).
Contributor Information
Jan Holcik, Department of Social Medicine and Health Care Administration, Masaryk University, Medical Faculty, Jostova 10, 662 43 Brno, Czech Republic.
Ilona Koupilova, Department of Social Medicine and Health Care Administration, Masaryk University, Medical Faculty, Jostova 10, 662 43 Brno, Czech Republic and Senior Lecturer in Epidemiology, European Centre on Health of Societies in Transition, London School of Hygiene & Tropical Medicine, Keppel Street, London WC1E 7HT, UK.
References
- 1.WHO. Integration of health care delivery. Report of a WHO Study Group. Geneva: WHO; 1996. (WHO Technical Report Series 861). [PubMed] [Google Scholar]
- 2.Health care systems in transition: Czech Republic. European Observatory on Health Care Systems. 1999.
- 3.Massaro TA, Nemec J, Kalman I. Health system reform in the Czech Republic. Policy lessons from the initial experience of the general health insurance company. Journal of the American Medical Association. 1994;271(23):1870–4. [PubMed] [Google Scholar]
- 4.Drbal C. The nation and health care [in Czech] Casopis Lekaru Ceskych. 1994;133(2):35–6. [PubMed] [Google Scholar]
- 5.Koupilova I, McKee M, Holcik J. Neonatal mortality in the Czech Republic during the transition. Health Policy. 1998;46(1):43–52. [PubMed] [Google Scholar]
- 6.Meijerman A, Papes Z, Pfeiffer J, Struk P, Steflova A, editors. Development of primary care in the Czech Republic. Final report. PHARE CZ 9201-24.01-L002. Prague: 1997. [Google Scholar]
- 7.Stich Z. Health Care in Czechoslovakia. Prague: 1961. [Google Scholar]
- 8.Sipr K. How to increase the attractiveness and efficiency of the work of a general practitioner [in Czech]? Ceske Zdravotnictvi. 1971;19(9):386–9. [PubMed] [Google Scholar]
- 9.Seifert B, Struk P. Abstracts from the Annual Meeting of EUPHA; 9–11 December 1999. Prague: Czech initiatives and perspectives in primary health care; p. 153. [Google Scholar]
- 10.Misconiova B. Comprehensive home care in the Czech Republic. Caring. 1998;17(4):38–41. [PubMed] [Google Scholar]
- 11.Holcik J, Koupilova I, Gerylovova A. Health needs: geographical distribution and relation to use of health services in districts of the Czech Republic [in Czech] Casopis Lekaru Ceskych. 1997;136(21):662–5. [PubMed] [Google Scholar]
- 12.Zavazalova H, Bremer C, Motan J, Zaremba V, Vozehova S. General physicians at the beginning of health services transformation [in Czech] Casopis Lekaru Ceskych. 1997;136(16):507–8. [PubMed] [Google Scholar]
- 13.Jaros J, Kalina K, editors. Czech Health Care System: Delivery and Financing. OECD study. Czech Association for Health Services Research; 1998. [Google Scholar]
- 14.Drbal C. The role of specialist ambulatory care in the health care system [in Czech] Zdravotnictvi v Ceske republice. 1999;2(2–3):70–5. [Google Scholar]
- 15.Steflova A. Development of primary care in the Czech Republic [in Czech] Lekarske listy. 1998 Jan 16;:1–3. [Google Scholar]
- 16.Papes Z. Primary care and health care system [in Czech] Zdravotnictvi v Ceske republice. 1998;1(4):8–13. [Google Scholar]
- 17.Hrobon P, Chlumsky J, Jirasek V, Kvapil M. Assessment of the need for and length of hospitalisation at an internal medicine department [in Czech] Vnitrni Lekarstvi. 1998;44(9):541–6. [PubMed] [Google Scholar]
- 18.Hrobon P, Schwarz J, Smutny S, Wald M. Experience with the use of criteria for evaluation the need for hospitalisation in a surgery department [in Czech] Rozhledy v Chirurgii. 1998;77(9):408–13. [PubMed] [Google Scholar]
- 19.Handysides S. New roles for general practitioners. British Medical Journal. 1994;308(6927):513–6. doi: 10.1136/bmj.308.6927.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenmoller M. Health systems reforms in Central and Eastern European countries. A fondo: health systems reforms. [cited 2000 Oct 24]. Available from: URL: http://www.ee-iese.com/66/afondoart4.html.