Abstract
Risk stratification is crucial in prevention. Circulating microRNAs have been proposed as biomarkers in cardiovascular disease. Here a miR panel consisting of miRs related to different cardiovascular pathophysiologies, was evaluated to predict outcome in the context of prevention. MiR-34a, miR-223, miR-378, miR-499 and miR-133 were determined from peripheral blood by qPCR and combined to a risk panel. As derivation cohort, 178 individuals of the DETECT study, and as validation cohort, 129 individuals of the SHIP study were used in a case-control approach. Overall mortality and cardiovascular events were outcome measures. The Framingham Risk Score(FRS) and the SCORE system were applied as risk classification systems. The identified miR panel was significantly associated with mortality given by a hazard ratio(HR) of 3.0 (95% (CI): 1.09–8.43; p = 0.034) and of 2.9 (95% CI: 1.32–6.33; p = 0.008) after adjusting for the FRS in the derivation cohort. In a validation cohort the miR-panel had a HR of 1.31 (95% CI: 1.03–1.66; p = 0.03) and of 1.29 (95% CI: 1.02–1.64; p = 0.03) in a FRS/SCORE adjusted-model. A FRS/SCORE risk model was significantly improved to predict mortality by the miR panel with continuous net reclassification index of 0.42/0.49 (p = 0.014/0.005). The present miR panel of 5 circulating miRs is able to improve risk stratification in prevention with respect to mortality beyond the FRS or SCORE.
Similar content being viewed by others
Introduction
Ischemic heart disease is the major cause of death in western countries and is progressively occurring with increasing age1. Until the year 2050, the United Nations predict a constant decrease of the age group 25–49 years and, at the same time, an increase of individuals aged 50 years and above in developed countries2.
Given these facts, the need for new and improved preventive strategies arises. Use of an individualized therapy allows specific treatments of patients and may thereby be beneficial for the patient as well as for the healthcare system3, 4. Therefore, identification of patients suitable for specific therapies is of major importance. In primary care studies5, 6 as well as in clinical routine commonly scoring systems like the Framingham risk score (FRS)7 or the SCORE system of the European Society of Cardiology8 are used to identify patients at risk for overt cardiovascular events.
Recently, the use of various biomarkers has been proposed to facilitate such an identification processes. Several biomarkers are able to amend the prognostic ability of e.g. the FRS9. In this regard, it has been shown that elevated C-reactive protein (CRP) levels as biomarker for inflammation defines a patient population that benefits from statin therapy3. This underlines the potential of biomarkers as a useful tool e.g. in primary prevention. Furthermore, the use of a multiple biomarker approach, reflecting different pathophysiological aspects, has been shown to add useful prognostic information and, therefore, consistently improved risk estimation for incident cardiovascular event9.
MicroRNAs (miRs) are single-stranded, non-coding nucleotide sequences functioning by binding to specific target mRNAs and inhibiting their translational processing10. MiRs were detected in various body fluids and can also reliably be measured in peripheral blood11. Circulating miRs have been shown to be valid biomarkers in a broad spectrum of cardiovascular diseases such as acute myocardial infarction or stable heart disease12, 13. MiRs show specific regulation patterns in a transcript and disease related manner. This raises the question for an implementation of miRs as biomarkers for prevention on a multi-marker level.
Based on published literature and own work, several microRNAs seem promising to be included in such a multi-marker approach for the prediction of cardiovascular morbidity and mortality. MiR-34a was shown to regulate cardiac aging14. Furthermore, miR-34a is associated with left ventricular remodeling after myocardial function14,15,16. MiR-223 modulates inflammation, regulating granulocyte function17 and controlling cardiomyocyte glucose metabolism18.
MiR-378 counteracts obesity by controlling brown fat expansion19 and blocks cardiac hypertrophy20. MiR-133 modulates skeletal muscle proliferation and differentiation20, 21 and seems to control cardiac hypertrophy22.
Finally, the cardiac expressed miR-499, the prototype miR used as potential diagnostic biomarker indicating myocardial infarction23, that was suggested to also be a marker of myocyte damage in various cardiovascular diseases24.
The present study tests and validates the prognostic ability of these selected miRs for the prediction of cardiovascular outcome and death using a sample of primary care patients and an independent general population-sample. We further determined the potential amendatory prognostic information of circulating miRs within a multi marker approach on top of the established FRS or SCORE.
Methods
Study Population
For this investigation, data of two independent prospective cohorts were utilized. First, a derivation cohort was used to evaluate the prognostic value of the proposed miR panel in a low to intermediate risk real-world population representative for individuals presenting themselves to their primary care physician. Second, the predictive value of the miR panel was validated in a population-based sample excluding individuals with prevalent cardiovascular diseases to evaluate the use of the miR panel in the context of primary prevention. The local ethics review board approved the protocols of both studies an they were conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from each individual.
Derivation Cohort
As derivation cohort, data of the prospective longitudinal Diabetes Cardiovascular Risk Evaluation Targets and Essential Data for Commitment of Treatment (DETECT) study was use25. This study consists of a representative German sample of 3,188 primary care offices run by physicians including medical practitioners, general practitioners, and general internists. Here, 55,518 unselected consecutive individuals were enrolled on two predefined half-days. For laboratory analyses, a random sub-sample of 7,519 participants in 1,000 primary care practices was selected. Out of this sub-sample, 178 representative individuals were randomly chosen. This sample was used for the present analyses including 21 subjects who reached the pre-defined combined endpoint of occurrence of a cardiovascular event and overall mortality within a 5-year follow-up period and 157 controls. Cardiovascular event was defined as first occurrence of death from cardiovascular causes, non-fatal myocardial infarction or need for coronary revascularization including coronary bypass surgery and percutaneous coronary intervention. State of health and medical history within the follow-up period was obtained at the 5-year follow-up in 2008 from the primary care physician or by the institution in which the patients were previously treated using standardized assessment forms.
Venous blood samples were obtained at enrollment, immediately frozen and stored at −80 °C until further analyses. The DETECT study was approved by the ethics committee of the Carl Gustav Carus Medical Faculty, Technical University of Dresden (NCT01076608).
Validation Cohort
The Study of Health in Pomerania (SHIP) served as external validation cohort26. The SHIP is a population-based study that enrolled adult German residents of West Pomerania in northeastern Germany. For the present analyses, 64 individuals without a history of cardiovascular disease (CVD; including coronary artery disease, heart failure, history of stroke or peripheral artery disease) who died (death from any cause, primary endpoint) within a 12-year follow-up period were randomly chosen as cases. As controls, 65 additional individuals without prevalent CVD were selected from this study. Cases and controls were matched according to age and gender in a 1:1 ratio. As secondary outcome measure the combined endpoint of cardiovascular death, non-fatal myocardial infarction or stroke was used, reached by 43 out of the 129 individuals of the study cohort. Within the SHIP study a mortality follow-up is performed annually collecting information on vital status from population registries. Here, death certificates are obtained from the local health authorities. The underlying cause of death is validated independently by two medical doctors specialized in internal medicine. In case of disagreement a third internist is consulted. Further, a morbidity follow-up was obtained by postal questionnaires. Non- responders were contacted by telephone. Results were validated by the general practitioners26.
For all subjects, non-fasting blood samples were drawn, aliquoted and stored at −80 °C for further analysis. All study participants gave written informed consent. The SHIP study was approved by the ethics committee of the University of Greifswald.
Laboratory Analyses
MicroRNA Panel
To test the hypothesis that a panel of distinct miRs is able to provide relevant prognostic information in prevention we selected 5 specific miRs. Selection was based on literature review of the authors as well as our own work. Criteria for selection were valid published data on an association with known cardiovascular risk factors or aspects of cardiovascular disease as well as the ability for quantification as circulating miRs in peripheral blood with respect to a potential use as biomarkers. Our selection included miR-34a with its role to regulate cardiac aging14, miR-223 in the context of inflammation17, 18, miR-378 associated with brown fat expansion19 and cardiac hypertrophy20, miR-133 with association to cardiac hypertrophy22, and the cardio-specific miR-49924. These microRNAs were quantified by qRT-PCR.
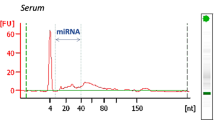
RNA Isolation and Quantification of miR levels
For isolation of total RNA, 250 μL EDTA-plasma was mixed with 700 µl TRIzol BD (Sigma; T3809), RNA was further isolated using the miRNeasy kit (Qiagen; 217004) using a Qiacube (Qiagen) sample preparation automat. The procedure was carried out in accordance to the manufacture’s protocol, with the exception that 30 µl of RNase-free purified water were used for final RNA elution.
RNA was then diluted 1:10 with H2O. The diluted RNA (5 μL) was reverse transcribed using the TaqMan microRNA Stemloop RT kit (ABI) according to the manufacture’s protocol. Subsequently, 3 μL of the product was used for detecting miR levels of miRs-34a, miR-223, miR-378, miR-499 and miR-133 by (q)PCR using TaqMan microRNA Assay kits (ABI) (Supplementary Methods). For qPCR using hydrolysis probes the VIAA7 Real-Time PCR System (ABI) was used. Relative miR levels were calculated as 2−(CT[microRNA]). For the current analyses, no normalization was done. RNA isolation and miR quantification were performed by experienced technicians blinded to the study participants clinical characteristics at a RNA core lab at the Goethe University Frankfurt.
Conventional Laboratory Analyses
Lipids and serum creatinine were measured at the respective study site using standardized laboratory methods. Glomerular filtration rate was estimated (eGFR) using the abbreviated Modification of Diet in Renal Disease (MDRD) formula. In the DETECT study, cardiac troponin I, NT-proBNP and CRP were quantified using commercially available assays with troponin I (Advia Centaur TnI- Ultra, Siemens), NT-proBNP and hsCRP (both Roche Diagnostics) and hsCRP. All measurements were carried out by experienced staff blinded to the participant’s characteristics.
Statistical Analyses
Continuous variables are given as mean with corresponding standard deviation (SD) or as median with interquartile range in case of a skewed distribution. Associations between miRs and biomarkers such as laboratory parameters as well as clinical parameters were assessed with Spearman rank correlation coefficient. Survival functions were derived from a Kaplan-Meier estimator. To estimate the prognostic property of the miRs, Cox proportional hazards models for all-cause mortality or the combined cardiovascular endpoint were estimated. The miR measurements were taken as predictors. As the proportional hazards assumptions have been emphasized by the chi square statistic for Schoenfeld residuals, hazard ratios (HR) are given per standard deviation (SD) increase as well as after dichotomization with threshold based on an optimized Youden index. Wald confidence intervals and corresponding p-values are provided. HRs were calculated for an un-adjusted model as well as after adjustment for (i) age and sex and (ii) a combination of the Framingham risk score variables (age, gender, cholesterol, HDL, smoking, blood pressure). Along with the singular miRs, a score from a multivariate miR panel was calculated by means of an unadjusted logistic regression model with occurence of an event ((i) death and (ii) combined endpoint) as binary outcome: the setting of the model coefficients gives rise to a linear combination of predictors, such that its logit-transform is the risk estimated by the model, which defines the predicted score. To evaluate the additional prognostic information of the miR panel beyond a model based on a combination of the Framingham risk score variables receiver operator characteristic (ROC) analyses, Harrell’s c-index as well as reclassification indices have been used. Differences between respective area under the curve in the ROC analyses and between c-indices were calculated by the methods proposed by DeLong27 and Kang28. The continuous net reclassification index (NRI)29, and the absolute and relative integrated discrimination improvement (IDI)30 were calculated with a cNRI of 0.39 (0.61) considered as having relevant power31. All analyses were done using R 3.1.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Characteristics of the derivation cohort
The derivation cohort comprised 178 representative individuals of the DETECT study, including 101 (56.7%) females, with median age of 55.5 (46–69) years. The characteristics of this study sub-cohort in comparison to the overall DETECT cohort are shown as Supplementary Table 1. Within the follow-up period of 5 years, 12 of these study participants died and 21 experienced the combined endpoint of a cardiovascular event or death. Table 1 provides the baseline characteristics of the derivation cohort classified by event state. As expected, individuals with poor outcome had a higher cardiovascular risk profile with respect to traditional risk factors such as arterial hypertension, dyslipidemia or diabetes (all p < 0.05) compared to event-free survivors. This is also depicted by a higher FRS with 0.42 compared to a FRS of 0.11 (p < 0.001). In accordance, individuals who experienced an event had both more often a history of heart failure and higher levels of NT-proBNP compared to those with an event-free follow-up. Evaluation of a potential association of continuous variables associated with risk, such as total cholesterol or C-reactive protein (CRP), and the selected miRs showed a weak but significant correlation of CRP with miR-378 (r = 0.22, p = 0.002) and miR-133 (r = 0.14, p = 0.048) (see Supplementary Table 2A).
Prognostic value of selected circulating miRs and their combination in the derivation cohort
Individual levels of the selected 5 miR miRs-34a, miR-223, miR-378, miR-499 and miR-133 were not associated with the combined endpoint. All-cause 5-year mortality was associated with reduced miR-133 levels (HR: 0.09; 95% CI: 0.01, 0.86; p = 0.037) and showed a trend for the association with lower miR-223 levels (HR: 0.30; 95% CI: 0.08, 1.07; p = 0.063) (Table 2).
Combination of the 5 miRs as panel showed a robust association with overall mortality with HR of 3.03 (95% CI: 1.09, 8.43; p = 0.034) in an unadjusted model and of 2.89 (95% CI: 1.32, 6.33; p = 0.008) after adjustment for the FRS variables (Table 2) or for the biomarkers NT-proBNP or troponin I (Supplementary Table 3). Nevertheless, no significant association with the combined endpoint was observed (Tables 2 and 3).
Furthermore, the miR panel significantly improved the discriminatory value of the FRS variables to identify patients at risk to die within 5 years with an increase of the area under the curve in the receiver operator characteristic analysis from 0.77 to 0.85 (p = 0.039)32. The respective c-index tended to be improved from 0.73 to 0.85 (p = 0.074).
Validation cohort, characteristics and differences to the derivation cohort
Of the 129 individuals of the SHIP validation cohort, 64 died and 43 experienced a cardiovascular event within the 12-year follow-up period. In this primary prevention population, the proportion of traditional risk factors did not differ between individuals who died and survivors. The respective baseline characteristics classified according to event status are given as Table 3.
In this population-based sample, the associations of CRP with miR-378 and miR-133 observed in the derivation cohort could not be replicated; furthermore a weak negative correlation of CRP and miR-499 was seen (r = −0.20, p = 0.03) (Supplementary Table 2B).
Prognostication using circulating miRs in the validation cohort
The predictive information of the prognostic miR panel observed in the derivation cohort could be confirmed in the validation cohort with a HR of 1.31 (95% CI: 1.03, 1.66; p = 0.03) to predict all-cause mortality after adjusting for the FRS variables. Using cardiovascular events as outcome measure, application of the prognostic miR panel resulted in a HR of 1.29 (95% CI: 0.99, 1.69; p = 0.0) in a FRS adjusted model. Comparable results are seen if SCORE instead of FRS variables were used for adjustment (Table 4).
In order to more closely reflect a potential real world application, the prognostic miR panel was further evaluated in a dichotomized fashion, providing the information high vs. low mortality risk. Here, the miR panel showed a FRS independent association with mortality and cardiovascular events with HR of 1.31 (95% CI: 1.03, 1.66; p = 0.03) and of 1.29 (95% CI: 0.99, 1.69; p = 0.06), respectively (Supplementary Table 4). Of interest, none of the 5 miRs showed a significant association with cardiovascular events or mortality, if analyzed individually (Supplementary Table 5). As sensitivity analysis, all possible 4 marker combinations were calculated yielding HRs from 1.13 to 1.33 for the prediction of death (Supplementary Table 6).
To further evaluate, if the prognostic miR panel provides information beyond that provided by the established risk scores such as the FRS or SCORE, reclassification analyses were performed. Here, a risk stratification model based on the FRS or the SCORE variables was significantly improved regarding the prediction of mortality by addition of the 5 miR panel. This is substantiated by a continuous net reclassification index (cNRI) of 0.42 (p = 0.014) and 0.49 (p = 0.005) as well as an integrated discrimination improvement (IDI) of 0.03 (p = 0.047) and 0.027 (p = 0.065) of a base model using FRS or SCORE variables, respectively, (Table 5). Nevertheless, the miR panel was not able to improve the c-index of a model based on the FRS or the SCORE variables (Data not shown).
Discussion
The results of the present study suggest, for the first time, that a panel of specific circulating miRs, measured from peripheral venous blood samples, may provide valid prognostic information in the context of risk prediction in prevention.
The proposed panel includes 5 distinct miRs that represent different pathomechanisms, namely age, inflammation, metabolism, and muscle damage that are known to play important roles in cardiovascular disease development and progression.
If analyzing the miRs individually, not as panel, the selected miR did not show a reproducible association with outcome. In contrast, the combined use of the 5 miRs as a panel showed a robust prediction of mortality in the derivation and validation cohort independently of the clinical risk variables. Furthermore, the miR panel significantly improved the prognostic value of e.g. the FRS variables to identify patients who will die with e.g. an AUC improvement from of 0.77 to 0.85 (p = 0.039) in the derivation cohort and a cNRI of 0.42 (p = 0.014) in the validation cohort. Within the validation cohort the prognostic power of our panel provided a lower HR compared to the validation cohort. As the validation cohort represents patients at risk whereas the validation study stems from a population based cohort with low risk this difference is what one would expect.
There are very few data on the potential use of miRs as biomarkers for outcome prediction in cardiovascular prevention. Zampetaki et al. evaluated 19 candidate miRs in a population based cohort of 820 individuals with respect to their relation with incident myocardial infarction. Here, a significant association of miR-126, miR-223 and miR-197 was observed33. Moreover, this study revealed that platelets are a major contributor to circulating levels of miR-126.
Furthermore, an association of circulating miR levels with clinical outcome could be shown in studies investigating patients with acute coronary syndrome. In those studies, the muscle-enriched miR-133a34, 35 and miR-49936, 37 were suggested to provide prognostic information, although the added value to the classical myocardial damage marker troponin was only marginal.
Conventional biomarkers associated with inflammation such as C-reactive protein38, with left ventricular wall stress such as natriuretic peptides39 or with myocardial damage such as cardiac troponins40, 41 have shown prognostic value in general population cohorts. Furthermore, the concept of using a combination of markers picturing different pathophysiologic mechanisms of cardiovascular disease development and progression has been proposed to improve risk estimation if added to conventional risk models as used in daily clinical routine9, 42, 43.
Use of miR signatures provides superior diagnostic information compared to a single miR44 in evaluation of acute myocardial infarction supporting the concept of using a miR panel rather than a specific miR that might reflect only one aspect of cardiovascular disease development.
Given the multifunctional mechanisms involved in cardiovascular disease development and mortality, it is not surprising that combining analytes of different biomarkers reflecting different underlying pathophysiological mechanisms will therefore provide superior information as also exemplified in the present study for circulating miRs.
Limitations
The most important limitation of the presents study relates to the limited number of endpoints in our case-control cohorts. It is one of the first studies evaluating the use of a miR panel for risk prediction; given this limitation, a prospectively and independently validation of the observed results is needed. Moreover, the used risk scores were developed mainly to predict cardiovascular events in population-based cohorts. In the present study, while the miR panel robustly predicted overall mortality, the prognostic value for cardiovascular endpoints was less convincing.
Conclusion
A panel of 5 selected circulating miRs associated with distinctive pathophysiological mechanisms is able to improve risk stratification in primary and secondary prevention with respect to mortality beyond and amendatory to the widely-used Framingham Risk Score.
References
Finegold, J. A., Asaria, P. & Francis, D. P. Mortality from ischaemic heart disease by country, region, and age: statistics from World Health Organisation and United Nations. Int. J. Cardiol. 168, 934–45 (2013).
World Population Prospects: The 2012 Revision (2014).
Ridker, P. M. et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N. Engl. J. Med. 359, 2195–207 (2008).
Ohsfeldt, R. L., Olsson, A. G., Jensen, M. M., Gandhi, S. K. & Paulsson, T. Cost-effectiveness of rosuvastatin 20 mg for the prevention of cardiovascular morbidity and mortality: a Swedish economic evaluation of the JUPITER trial. J. Med. Econ. 15, 125–33 (2012).
Chamnan, P. et al. A simple risk score using routine data for predicting cardiovascular disease in primary care. Br. J. Gen. Pract. 60, e327–34 (2010).
Conroy, R. M. et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur. Heart J. 24, 987–1003 (2003).
Wilson, P. W. et al. Prediction of coronary heart disease using risk factor categories. Circulation 97, 1837–47 (1998).
Perk, J. et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012): The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 33, 1635–1701 (2012).
Blankenberg, S. et al. Contribution of 30 biomarkers to 10-year cardiovascular risk estimation in 2 population cohorts: the MONICA, risk, genetics, archiving, and monograph (MORGAM) biomarker project. Circulation 121, 2388–97 (2010).
Bartel, D. P. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116, 281–97 (2004).
Fichtlscherer, S. et al. Circulating microRNAs in patients with coronary artery disease. Circ. Res. 107, 677–84 (2010).
Gupta, S. K., Bang, C. & Thum, T. Circulating microRNAs as biomarkers and potential paracrine mediators of cardiovascular disease. Circ. Cardiovasc. Genet 3, 484–8 (2010).
Small, E. M. & Olson, E. N. Pervasive roles of microRNAs in cardiovascular biology. Nature 469, 336–42 (2011).
Boon, R. A. et al. MicroRNA-34a regulates cardiac ageing and function. Nature 495, 107–10 (2013).
Lv, P. et al. Circulating miR-208b and miR-34a are associated with left ventricular remodeling after acute myocardial infarction. Int. J. Mol. Sci. 15, 5774–88 (2014).
Yang, Y. et al. MicroRNA-34a Plays a Key Role in Cardiac Repair and Regeneration Following Myocardial Infarction. Circ. Res. 117, 450–9 (2015).
Johnnidis, J. B. et al. Regulation of progenitor cell proliferation and granulocyte function by microRNA-223. Nature 451, 1125–9 (2008).
Lu, H., Buchan, R. J. & Cook, S. A. MicroRNA-223 regulates Glut4 expression and cardiomyocyte glucose metabolism. Cardiovasc. Res. 86, 410–20 (2010).
Pan, D. et al. MicroRNA-378 controls classical brown fat expansion to counteract obesity. Nat. Commun. 5, 4725 (2014).
Nagalingam, R. S. et al. A cardiac-enriched microRNA, miR-378, blocks cardiac hypertrophy by targeting Ras signaling. J. Biol. Chem. 288, 11216–32 (2013).
Chen, J.-F. et al. The role of microRNA-1 and microRNA-133 in skeletal muscle proliferation and differentiation. Nat. Genet. 38, 228–33 (2006).
Carè, A. et al. MicroRNA-133 controls cardiac hypertrophy. Nat. Med. 13, 613–8 (2007).
Adachi, T. et al. Plasma microRNA 499 as a biomarker of acute myocardial infarction. Clin. Chem. 56, 1183–5 (2010).
Corsten, M. F. et al. Circulating MicroRNA-208b and MicroRNA-499 reflect myocardial damage in cardiovascular disease. Circ. Cardiovasc. Genet 3, 499–506 (2010).
Wittchen, H.-U. et al. Cardiovascular risk factors in primary care: methods and baseline prevalence rates - the DETECT program. Curr. Med. Res. Opin. 21, 619–630 (2005).
Völzke, H. et al. Cohort profile: the study of health in Pomerania. Int. J. Epidemiol. 40, 294–307 (2011).
DeLong, E. R., DeLong, D. M. & Clarke-Pearson, D. L. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44, 837–45 (1988).
Kang, L., Chen, W., Petrick, N. A. & Gallas, B. D. Comparing two correlated C indices with right-censored survival outcome: a one-shot nonparametric approach. Stat. Med. 34, 685–703 (2015).
Pencina, M. J., D’Agostino, R. B., D’Agostino, R. B. & Vasan, R. S. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat. Med. 27, 157-72–12 (2008).
Pencina, M. J., D’Agostino, R. B. & Vasan, R. S. Statistical methods for assessment of added usefulness of new biomarkers. Clin. Chem. Lab. Med. 48, 1703–11 (2010).
Pencina, M. J., D’Agostino, R. B., Pencina, K. M., Janssens, A. C. J. W. & Greenland, P. Interpreting incremental value of markers added to risk prediction models. Am. J. Epidemiol. 176, 473–81 (2012).
Leistner, D. M. Moderne Risikostratifizierung in der kardiovaskulaeren Medizin: Untersuchungen zum Stellenwert neuer Risikofaktoren und Biomarker. (Berlin: Medizinische Fakultät Charité - Universitätsmedizin Berlin 2016).
Zampetaki, A. et al. Prospective study on circulating MicroRNAs and risk of myocardial infarction. J. Am. Coll. Cardiol. 60, 290–9 (2012).
Widera, C. et al. Diagnostic and prognostic impact of six circulating microRNAs in acute coronary syndrome. J. Mol. Cell. Cardiol. 51, 872–5 (2011).
Eitel, I. et al. Relation of circulating MicroRNA-133a concentrations with myocardial damage and clinical prognosis in ST-elevation myocardial infarction. Am. Heart J. 164, 706–14 (2012).
Gidlöf, O. et al. Circulating cardio-enriched microRNAs are associated with long-term prognosis following myocardial infarction. BMC Cardiovasc. Disord. 13, 12 (2013).
Olivieri, F. et al. Admission levels of circulating miR-499-5p and risk of death in elderly patients after acute non-ST elevation myocardial infarction. Int. J. Cardiol. 172, e276–8 (2014).
Ridker, P. M., Hennekens, C. H., Buring, J. E. & Rifai, N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N. Engl. J. Med. 342, 836–43 (2000).
Wang, T. J. et al. Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N. Engl. J. Med. 350, 655–63 (2004).
de Lemos, J. A. et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA 304, 2503–12 (2010).
Leistner, D. M. et al. Circulating troponin as measured by a sensitive assay for cardiovascular risk assessment in primary prevention. Clin. Chem. 58, 200–8 (2012).
Kistorp, C. et al. N-terminal pro-brain natriuretic peptide, C-reactive protein, and urinary albumin levels as predictors of mortality and cardiovascular events in older adults. JAMA 293, 1609–16 (2005).
Zethelius, B. et al. Use of multiple biomarkers to improve the prediction of death from cardiovascular causes. N. Engl. J. Med. 358, 2107–16 (2008).
Meder, B. et al. MicroRNA signatures in total peripheral blood as novel biomarkers for acute myocardial infarction. Basic Res. Cardiol. 106, 13–23 (2011).
Acknowledgements
We thank all individuals who participated in the DETECT and SHIP study. We further thank all investigators and study staff that contributed to these two studies. This evaluation was supported by the German Centre for Cardiovascular Research (DZHK) to the DZHK partner sites Rhine-Main (Frankfurt) and Greifswald and by SFB834 Project B1 to Stefanie Dimmeler.
Author information
Authors and Affiliations
Contributions
T.K. and J.N.B. did the literature search and wrote the first manuscript draft. T.K., J.N.B., D.L., L.P., G.K.S., H.L., S.S., D.P., W.M., M.D., H.U.W., S.E.B., U.W., S.B.F., S.D., A.M.S. enrolled patients, collected samples or were the trial Management Group members. Study supervision by T.K., S.B.F., S.D., A.M.Z. L.P., J.K. and S.G. did the statistical analyses. L.P., J.N.B., J.K., S.G. and T.K. had access to the raw data and analysed the data. W.M., H.U.W., S.B.F., A.M.Z. provided administrative, technical, or material support. All authors were involved in Analysis and interpretation of data as well as revised critically the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no Competing Interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Keller, T., Boeckel, JN., Groß, S. et al. Improved risk stratification in prevention by use of a panel of selected circulating microRNAs. Sci Rep 7, 4511 (2017). https://doi.org/10.1038/s41598-017-04040-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-04040-w
This article is cited by
-
MicroRNAs and Cardiovascular Disease Risk
Current Cardiology Reports (2024)
-
Small Molecules with Big Impacts on Cardiovascular Diseases
Biochemical Genetics (2020)
-
Looking to the Future: Spotlight on Emerging Biomarkers for Predicting Cardiovascular Risk
Current Epidemiology Reports (2018)
-
MicroRNAs in Heart Failure, Cardiac Transplantation, and Myocardial Recovery: Biomarkers with Therapeutic Potential
Current Heart Failure Reports (2017)