Abstract
Purpose
Intracranial electrodes are sometimes implanted in patients with refractory epilepsy to identify epileptic foci and propagation. Maximal recording of EEG activity from regions suspected of seizure generation is paramount. However, the location of individual contacts cannot be considered with current manual planning approaches. We propose and validate a procedure for optimizing intracranial electrode implantation planning that maximizes the recording volume, while constraining trajectories to safe paths.
Methods
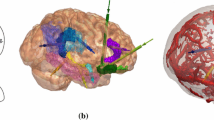
Retrospective data from 20 patients with epilepsy that had electrodes implanted in the mesial temporal lobes were studied. Clinical imaging data (CT/A and T1w MRI) were automatically segmented to obtain targets and structures to avoid. These data were used as input to the optimization procedure. Each electrode was modeled to assess risk, while individual contacts were modeled to estimate their recording capability. Ordered lists of trajectories per target were obtained. Global optimization generated the best set of electrodes. The procedure was integrated into a neuronavigation system.
Results
Trajectories planned automatically covered statistically significant larger target volumes than manual plans \(({p}<0.001)\). Median volume coverage was \(419\,\hbox { mm}^{3}\) for automatic plans versus \(23\,\hbox { mm}^{3}\) for manual plans. Furthermore, automatic plans remained at statistically significant safer distance to vessels \(({p}<0.05)\) and sulci \(({p}<0.001)\). Surgeon’s scores of the optimized electrode sets indicated that 95 % of the automatic trajectories would be likely considered for use in a clinical setting.
Conclusions
This study suggests that automatic electrode planning for epilepsy provides safe trajectories and increases the amount of information obtained from the intracranial investigation.









Similar content being viewed by others
References
Engel J, Pedley TA (2008) Epilepsy: a comprehensive textbook. Wolters Kluwer Health/Lippincott Williams & Wilkins, Philadelphia
Olivier A, Boling WW, Tanriverdi T (2012) Techniques in epilepsy surgery: the MNI approach. Cambridge medicine. Cambridge University Press, Cambridge
Guenot M, Isnard J, Ryvlin P, Fischer C, Ostrowsky K, Mauguiere F, Sindou M (2001) Neurophysiological monitoring for epilepsy surgery: the Talairach SEEG method. Stereotact Funct Neurosurg 77(1–4):29–32
Cossu M, Schiariti M, Francione S, Fuschillo D, Gozzo F, Nobili L, Russo GL (2012) Stereoelectroencephalography in the presurgical evaluation of focal epilepsy in infancy and early childhood. J Neurosurg Pediatr 9(3):290–300. doi:10.3171/2011.12.PEDS11216
Guénot MM (2011) SEEG-guided RF-thermocoagulation of epileptic foci: a therapeutic alternative for drug-resistant non-operable partial epilepsies. Adv Tech Stand Neurosurg 36:61–78
Tanriverdi T, Ajlan A, Poulin N, Olivier A (2009) Morbidity in epilepsy surgery: an experience based on 2449 epilepsy surgery procedures from a single institution. J Neurosurg 110(6):1111–1123. doi:10.3171/2009.8.JNS08338
Grewal S, Gotman J (2005) An automatic warning system for epileptic seizures recorded on intracerebral EEGs. Clin Neurophysiol 116(10):2460–2472. doi:10.1016/j.clinph.2005.05.020
Janjarasjitt S (2014) Spectral exponent characteristics of intracranial EEGs for epileptic seizure classification. IRBM. doi:10.1016/j.irbm.2014.07.005
Brown MW III, Porter BE, Dlugos DJ, Keating J, Gardner AB, Storm PB Jr, Marsh ED (2007) Comparison of novel computer detectors and human performance for spike detection in intracranial EEG. Clin Neurophysiol 118(8):1744–1752. doi:10.1016/j.clinph.2007.04.017
Zelmann R, Mari F, Jacobs J, Zijlmans M, Dubeau F, Gotman J (2011) A comparison between detectors of high frequency oscillations. Clin Neurophysiol 123(1):106–116. doi:10.1016/j.clinph.2011.06.006
Beriault S, Al Subaie F, Mok K, Sadikot AF, Pike GB (2011) Automatic trajectory planning of DBS neurosurgery from multi-modal MRI datasets. Medical image computing and computer-assisted intervention: MICCAI International Conference on Medical Image Computing and Computer-Assisted Intervention 14(Pt 1), pp 259–266
Beriault S, Subaie FA, Collins DL, Sadikot AF, Pike GB (2012) A multi-modal approach to computer-assisted deep brain stimulation trajectory planning. Int J Comput Assist Radiol Surg 7(5):687–704. doi:10.1007/s11548-012-0768-4
Beriault S, Xiao Y, Bailey L, Collins DL, Sadikot AF, Pike GB (2012) Towards computer-assisted deep brain stimulation targeting with multiple active contacts. Medical image computing and computer-assisted intervention : MICCAI International Conference on Medical Image Computing and Computer-Assisted Intervention 15(Pt 1), pp 487–494
D’Albis T, Haegelen C, Essert C, Fernandez-Vidal S, Lalys F, Jannin P (2014) PyDBS: an automated image processing workflow for deep brain stimulation surgery. Int J Comput Assist Radiol Surg. doi:10.1007/s11548-014-1007-y
Essert C, Haegelen C, Lalys F, Abadie A, Jannin P (2012) Automatic computation of electrode trajectories for deep brain stimulation: a hybrid symbolic and numerical approach. Int J Comput Assist Radiol Surg 7(4):517–532
Guo T, Parrent A, Peters T (2007) Automatic target and trajectory identification for deep brain stimulation (DBS) procedures. Medical Image Computing and Computer-Assisted Intervention-MICCAI 2007, pp 483–490
Liu Y, Dawant BM, Pallavaram S, Neimat JS, Konrad PE, D’Haese P-F, Noble JH (2012) A surgeon specific automatic path planning algorithm for deep brain stimulation. In: SPIE Medical Imaging, International Society for Optics and Photonics, pp 83161D–83161D-83110
De Momi E, Caborni C, Cardinale F, Casaceli G, Castana L, Cossu M, Ferrigno G (2014) Multi-trajectories automatic planner for StereoElectroEncephaloGraphy (SEEG). Int J Comput Assist Radiol Surg. doi:10.1007/s11548-014-1004-1
De Momi E, Caborni C, Cardinale F, Castana L, Casaceli G, Cossu M, Ferrigno G (2013) Automatic trajectory planner for stereoelectroencephalography procedures: a retrospective study. IEEE Trans Biomed Eng 60(4):986–993
Zombori G, Rodionov R, Nowell M, Zuluaga MA, Clarkson M, Micallef C, et al. (2014) A computer assisted planning system for the placement of SEEG electrodes in the treatment of epilepsy. In: Stoyanov D, Collins DL, Sakuma I, Abolmaesumi P, Jannin P (eds) Information processing in computer-assisted interventions, vol 8498. Lecture notes in computer science. Springer, pp 118–127. doi:10.1007/978-3-319-07521-1_13
Zelmann R, Beriault S, Mok K, Haegelen C, Hall J, Pike GB, Collins DL (2014) Automatic optimization of depth electrode trajectory planning. In: Clinical image-based procedures translational research in medical imaging, pp 99–107
Mok K, Barecki R, Podaras M, Chatillion C, Sherafat E, Olivier A (2011) Towards detailed representation of cortical anatomy and vasculature in neuronavigation. In: Epilepsy currents, 12(s1):125
Collins DL, Pruessner JC (2010) Towards accurate, automatic segmentation of the hippocampus and amygdala from MRI by augmenting ANIMAL with a template library and label fusion. NeuroImage 52(4):1355–1366. doi:10.1016/j.neuroimage.2010.04.193
Danielsson P-E (1980) Euclidean distance mapping. Comput Graph Image Process 14(3):227–248
Collins D, Zijdenbos A, Baaré W, Evans A (1999) ANIMAL+ INSECT: improved cortical structure segmentation. In: Information processing in medical imaging. Springer, pp 210–223
Frangi A, Niessen W, Vincken K, Viergever M (1998) Multiscale vessel enhancement filtering. Medical image computing and computer-assisted interventation–MICCAI’98, pp 130–137
Aubert-Broche B, Griffin M, Pike GB, Evans AC, Collins DL (2006) Twenty new digital brain phantoms for creation of validation image data bases. IEEE Trans Med Imaging 25(11):1410–1416. doi:10.1109/TMI.2006.883453
Eskildsen SF, Ostergaard LR (2006) Active surface approach for extraction of the human cerebral cortex from MRI. Medical image computing and computer-assisted intervention: MICCAI International Conference on medical image computing and computer-assisted intervention, 9(Pt 2), pp 823–830
Coupe P, Manjon JV, Fonov V, Pruessner J, Robles M, Collins DL (2011) Patch-based segmentation using expert priors: application to hippocampus and ventricle segmentation. Neuroimage 54(2):940–954. doi:10.1016/j.neuroimage.2010.09.018
Avants BB, Epstein CL, Grossman M, Gee JC (2008) Symmetric diffeomorphic image registration with cross-correlation: evaluating automated labeling of elderly and neurodegenerative brain. Med Image Anal 12(1):26–41. doi:10.1016/j.media.2007.06.004
Collins DL, Holmes CJ, Peters TM, Evans AC (1995) Automatic 3D model based neuroanatomical segmentation. Hum Brain Map 3(3):190–208
Mazziotta J, Toga A, Evans A, Fox P, Lancaster J, Zilles K, Mazoyer B (2001) A probabilistic atlas and reference system for the human brain: International Consortium for Brain Mapping (ICBM). Philos Trans R Soc Lond Ser B Biol Sci 356(1412):1293–1322. doi:10.1098/rstb.2001.0915
Mercier L, Del Maestro RF, Petrecca K, Kochanowska A, Drouin S, Yan CX, Collins DL (2011) New prototype neuronavigation system based on preoperative imaging and intraoperative freehand ultrasound: system description and validation. Int J Comput Assist Radiol Surg 6(4):507–522. doi:10.1007/s11548-010-0535-3
Cardinale F, Cossu M, Castana L, Casaceli G, Schiariti MP, Miserocchi A, Lo Russo G (2013) Stereoelectroencephalography: surgical methodology, safety, and stereotactic application accuracy in 500 procedures. Neurosurgery 72(3):353–366. doi:10.1227/NEU.0b013e31827d1161 discussion 366
Ryvlin P, Kahane P (2005) The hidden causes of surgery-resistant temporal lobe epilepsy: extratemporal or temporal plus? Current Opin Neurol 18(2):125–127
Liu Y, Konrad P, Neimat J, Tatter S, Yu H, Datteri R, Dhaese P (2014) Multi-surgeon, multi-site validation of a trajectory planning algorithm for deep brain stimulation procedures. IEEE Trans Biomedi Eng 99:1–10. doi:10.1109/TBME.2014.2322776
Rieder C, Kroeger T, Schumann C, Hahn HK (2011) GPU-based real-time approximation of the Ablation zone for radiofrequency ablation. IEEE Trans Vis Comput Graph 17(12):1812–1821. doi:10.1109/TVCG.2011.207
Essert C, Marchal M, Fernandez-Vidal S, D’Albis T, Bardinet E, Haegelen C, Jannin P (2012) Automatic parameters optimization for deep brain stimulation trajectory planning. DBSMC 2012:20
von Ellenrieder N, Beltrachini L, Muravchik CH (2012) Electrode and brain modeling in stereo-EEG. Clin Neurophysiol 123(9):1745–1754. doi:10.1016/j.clinph.2012.01.019
Khlebnikov R, Kainz B, Muehl J, Schmalstieg D (2011) Crepuscular rays for tumor accessibility planning. IEEE Trans Vis Comput Graph 17(12):2163–2172. doi:10.1109/TVCG.2011.184
Acknowledgments
This study was supported in part by the Canadian Institute of Health Research (CIHR MOP-74725) and the Natural Sciences and Engineering Research Council of Canada (NSERC 238739-06). RZ was supported by a Canadian Imperial Bank of Commerce-Montreal Neurological Institute (CIBC-MNI) Postdoctoral Fellowship and a Savoy Foundation Postdoctoral Fellowship. The authors would like to thank Anna Kochanowska and Simon Drouin for the implementation of IBIS GUI.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zelmann, R., Beriault, S., Marinho, M.M. et al. Improving recorded volume in mesial temporal lobe by optimizing stereotactic intracranial electrode implantation planning. Int J CARS 10, 1599–1615 (2015). https://doi.org/10.1007/s11548-015-1165-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-015-1165-6