Introduction
Pediculosis is caused by subspecies of the Anoplura insect: Pediculus humanus capitis (head lice), Pediculus humanus corporis (body lice), and Phthirus pubis (pubic lice). These obligate ectoparasites exclusively feed on human blood. Hematologic derangements are not commonly recognized complications of pediculosis. We describe a case of severe, symptomatic iron deficiency anemia and eosinophilia in the setting of a generalized pruritic rash found to be consistent with pediculosis corporis and capitis.
Case report
A 74-year-old woman with a history of paranoid schizophrenia presented to our emergency department with several weeks of progressive fatigue and exertional dyspnea, culminating in a presyncopal episode and altered mental status. She denied melena, hematochezia, hemoptysis, hematemesis, weight loss, poor appetite, and anorexia. Her medical history was otherwise notable for poor hygiene and at least 5 months of recurrent lice infestations. She lived alone in a single-room unit (marginal low-income housing).
Examination was notable for pale conjunctiva, skin pallor, diffuse linear excoriations with accentuation at the upper shoulders and waist, and hyperpigmented lichenified papules and plaques at the waist and bilateral axillary folds. There were neither burrows nor lesions involving hands, wrists, areola, genitalia, or buttocks. Impetiginization was absent. Numerous nits were identified on scalp hair shafts and lice along clothing seams (Fig 1).
Fig 1.
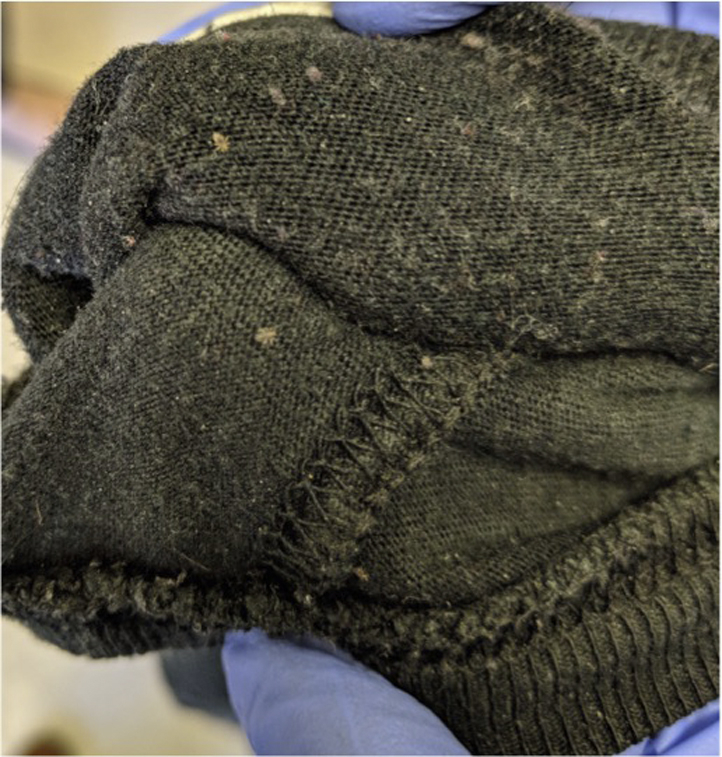
Diagnosis of pediculosis corporis requires careful clothing inspection to assess for lice within clothing seams, as pictured here with a different patient. Nits are also often seen.
Laboratory values at presentation were notable for hemoglobin, 3.8 g/dL (mean corpuscular volume, 72 fL); absolute eosinophil count (AEC), 540/μL (reference, 0-500); iron, 35 μg/dL (reference, 65-175); and ferritin, 5 ng/mL (reference, 22-322). Esophagogastroduodenoscopy and colonoscopy found a hiatal hernia and diverticulosis without active foci of bleeding. Full-body computerized tomography scan did not identify a significant source of bleeding.
The patient received several units of packed red blood cells, with subsequent normalization of hemoglobin, and was started on oral ferrous sulfate for iron deficiency. The patient showered. Home clothing and bedding was replaced by the patient's guardian. Permethrin 5% cream had been applied before dermatology consultation for empiric treatment of scabies. Permethrin 1% lotion was applied to hair and scalp followed by use of a nit comb and repeat permethrin application a week later. AEC peaked at 1600/μL on day 5 of admission—4 days after showering, discarding clothes, and initial application of permethrin.
Discussion
We present a case of pediculosis capitis and corporis associated with severe, symptomatic iron deficiency anemia and eosinophilia in a patient with a history of mental health illness and recurrent lice infestations. Recognition of excoriations and eczematous lesions localized to skin areas in close contact with clothing seams and subsequent visualization of lice along clothing seams were crucial in making the diagnosis of pediculosis corporis. Extensive workup did not find an internal bleeding source to account for profound anemia.
Although a causal relationship between lice infestation and iron deficiency anemia has not been clearly established, multiple case reports suggest heavy infestation can result in iron deficiency anemia caused by chronic, low-volume blood loss.1, 2, 3, 4, 5 These cases included children, homeless adults, and those with severe psychiatric comorbidities and were associated with profound iron deficiency anemia with hemoglobin values ranging from 2.2 to 5.7 g/dL in the setting of an otherwise unremarkable workup (Table I). Because hemoglobin levels are not routinely checked for pediculosis, we postulate that its association with anemia may be more prevalent than currently appreciated. In heavy or prolonged pediculosis infestation, health care providers should assess for symptoms and signs of anemia followed by checking a hemoglobin/hematocrit level if warranted based on assessment.
Table I.
Demographic and hematologic characteristics of other reported cases of severe pediculosis
| Study | Patient characteristics | Site | Hgb (MCV) | Iron studies | Absolute eosinophil count∗ |
|---|---|---|---|---|---|
| Gus et al1 | 61-year-old homeless man who presented with weakness | Head, body | 4.0 g/dL (60.6 μm3) | F 6 ng/dL | 3.0 k/μL |
| 55-year-old homeless woman who presented with dyspnea | Not reported | 3.2 g/dL (71.0 μm3) | F 5 ng/dL | 0 | |
| 43-year-old homeless man who presented with rash | Not reported | 5.7 g/dL (89.7 μm3) | F 19 ng/dL | 1.4 k/μL | |
| 52-year-old homeless man who presented with weakness | Not reported | 4.7 g/dL (76.0 μm3) | F 6 ng/dL | 0 | |
| 50-year-old homeless man who presented after assault | Not reported | 4.4 g/dL (63.8 μm3) | F 8 ng/dL | 0.77 k/μL | |
| 54-year-old homeless woman who presented with abdominal pain | Not reported | 5.7 g/dL (77.9 μm3) | F 11 ng/dL | 0.03 k/μL | |
| Hau and Muhi-Iddin2 | 11-year-old child who presented with pallor. Father had psychiatric problems and mother had learning disability. | Head, body | 4.2 g/dL (61.8 fL) | F 2 ng/dL I <1.8 μmol/L |
Not reported |
| Althomali et al4 | 23-year-old woman with severe depression who presented with fatigue and exertional chest pain | Head | 2.2 g/dL (60 μm3) | F 1.19 ng/dL I 3 μg/dL |
Not reported |
| Nara et al3 | 70-year-old man who died secondary to hypothermia (26.4°C) | Body | 4.6 g/dL (not reported) | Bone marrow analysis suggestive of iron deficiency anemia | Not reported |
| Takcı et al5 | 72-year-old woman who presented with 6-month history of generalized eczematous rash | Head | Anemia, Hgb not reported | Consistent with Iron deficiency, F not reported | Not reported |
F, Ferritin; Hgb, hemoglobin; I, iron; MCV, mean corpuscular volume.
Absolute eosinophil count calculated by multiplying percentage of eosinophils with white blood cell count, as reported in the original publication.
In addition to our case, eosinophilia (defined as AEC ≥ 500/μL) has been reported in 3 cases of lice infestation (Table I), with an AEC range of 770 to 3000/μL, and presence of body lice has been independently associated with AEC greater than 450/μL.6 Typically, hypereosinophilia (AEC > 1500/μL) would prompt a clinician to evaluate for internal organ involvement. In our case, eosinophilia increased for several days after body lice treatment, peaked at 1600/μL, and then declined to 980/μL the following day with subsequent normalization. Data are needed to better understand the clinical relevance of eosinophilia in lice infestation.
Other complications of pediculosis include secondary bacterial skin infections (impetigo, cellulitis), conjunctivitis, and lymphadenopathy. Prompt recognition and treatment of pediculosis corporis is also important for halting the spread of potentially life-threatening infections for which body lice are vectors: Bartonella quintana, Borrelia recurrentis, and Rickettsia prowazekii. In urban homeless populations, body lice infestation and B quintana infection (trench fever, bacillary angiomatosis) remain pertinent health conditions.7, 8 Homeless people have sporadic access to washing facilities, and those in high-income countries are substantially more likely to have mental health disorders,9 which can separately increase risk of pediculosis from neglect. In the context of global migration, body lice infestation is increasingly relevant in Europe and B recurrentis infection (relapsing fever) is seen in migrants from, or with close contact with individuals from, the horn of Africa.10
Body lice infestation reflects poor personal hygiene. Infested individuals should be bathed. Clothing/bedding should be discarded or washed in hot water (≥130°F) with high-heat machine drying. Although in our case, permethrin was administered before dermatology consultation, pediculicides are generally not required to treat body lice. In contrast, head lice infestation requires use of a topical pediculicide followed by removal of remaining lice with a nit comb every 2 to 3 days to decrease possibility of reinfestation. Depending on the pediculicide used, repeat treatment 7 to 10 days later may be needed to kill hatched lice before new eggs are produced, as many treatments are partially ovicidal.
Pediculosis continues to be a significant ailment on a global scale, including in the United States and Europe, where it is an increasingly relevant health condition because of growing homeless and migrant populations. Health care providers should utilize physical examination findings and clothing inspection to make the diagnosis of pediculosis corporis. In patients with heavy or prolonged pediculosis, health care providers have a potentially critical opportunity to identify iron deficiency anemia that may otherwise remain undetected until end-organ damage has occurred. Clinical relevance of eosinophilia in lice infestation is unclear. Body lice remain key vectors for contemporary B quintana, B recurrentis, and R prowazekii infections.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Guss D.A., Koenig M., Castillo E.M. Severe iron deficiency anemia and lice infestation. J Emerg Med. 2011;41(4):362–365. doi: 10.1016/j.jemermed.2010.05.030. [DOI] [PubMed] [Google Scholar]
- 2.Hau V., Muhi-Iddin N. A ghost covered in lice: a case of severe blood loss with long-standing heavy pediculosis capitis infestation. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-206623. bcr2014206623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nara A., Nagai H., Yamaguchi R. An unusual autopsy case of lethal hypothermia exacerbated by body lice-induced severe anemia. Int J Legal Med. 2016;130(3):765–769. doi: 10.1007/s00414-015-1266-3. [DOI] [PubMed] [Google Scholar]
- 4.Althomali S.A., Alzubaidi L.M., Alkhaldi D.M. Severe iron deficiency anaemia associated with heavy lice infestation in a young woman. BMJ Case Rep. 2015:2015. doi: 10.1136/bcr-2015-212207. bcr2015212207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Takcı Z., Tekin O., Karadağ A.S. A pediculid case: autosensitization dermatitis caused by pediculosis capitis. Turkiye Parazitol Derg. 2012;36(3):185–187. doi: 10.5152/tpd.2012.44. [DOI] [PubMed] [Google Scholar]
- 6.Brouqui P., Stein A., Dupont H., Gallan P., Badiaga S. Ectoparasitism and vector-borne diseases in 930 homeless people from Marseilles. Medicine (Baltimore) 2005;84(1):61–68. doi: 10.1097/01.md.0000152373.07500.6e. [DOI] [PubMed] [Google Scholar]
- 7.Bonilla D.L., Kabeya H., Henn J., Kramer V.L., Kosoy M.Y. Bartonella quintana in body lice and head lice from homeless persons, San Francisco, California, USA. Emerg Infect Dis. 2009;15(6):912–915. doi: 10.3201/eid1506.090054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drali R., Sangaré A.K., Boutellis A. Bartonella quintana in body lice from scalp hair of homeless persons, France. Emerg Infect Dis. 2014;20(5):907–908. doi: 10.3201/eid2005.131242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fazel S., Khosla V., Doll H., Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225. doi: 10.1371/journal.pmed.0050225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Meco E., Di Napoli A., Amato L.M. Infectious and dermatological diseases among arriving migrants on the Italian coasts. Eur J Public Health. 2018;28(5):910–916. doi: 10.1093/eurpub/cky126. [DOI] [PubMed] [Google Scholar]



