Overview
The anatomy of the hand is complex, intricate, and fascinating. Its integrity is absolutely essential for our everyday functional living. Our hands may be affected by many disorders, most commonly traumatic injury. For any physician or therapist treating hand problems, the mastery of such anatomy is fundamental to provide the best quality of care. (See the image below.) [1, 2, 3, 4, 5, 6, 7]
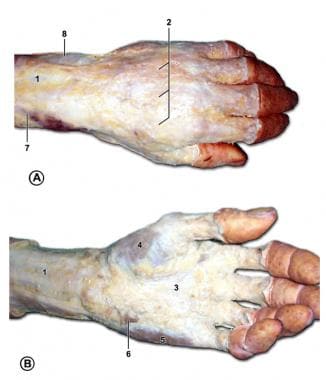
 Surface anatomy of the left hand. A is the dorsum of the left hand, and B is the palm of the left hand. Number 1 is the position of the extensor retinaculum, 2 is the position of the flexor retinaculum, 3 is the position of the head of the metacarpals, 4 is the ulnar artery, 5 is the radial artery, 6 is the level of the deep palmar arch, and 7 is the level of the superficial palmar arch.
Surface anatomy of the left hand. A is the dorsum of the left hand, and B is the palm of the left hand. Number 1 is the position of the extensor retinaculum, 2 is the position of the flexor retinaculum, 3 is the position of the head of the metacarpals, 4 is the ulnar artery, 5 is the radial artery, 6 is the level of the deep palmar arch, and 7 is the level of the superficial palmar arch.
A total of 27 bones constitute the basic skeleton of the wrist and hand. The hand is innervated by three nerves — the median, ulnar, and radial nerves — each of which has sensory and motor components. The muscles of the hand are divided into intrinsic and extrinsic groups.
Bones
As previously mentioned, a total of 27 bones constitute the basic skeleton of the wrist and hand. These are grouped into carpals, metacarpals, and phalanges (see the image below). These bones form the intricate structure of the wrist and hand, allowing for a wide range of movements necessary for daily tasks and complex functions. [8, 9]
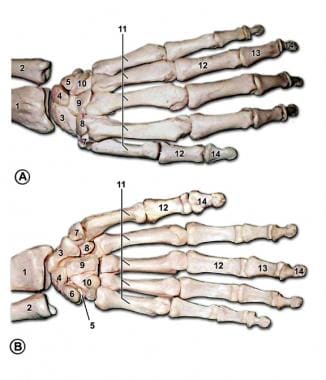 Bones of the left hand. A is the dorsal view, and B is the palmar view. Number 1 is the radius, 2 is the ulna, 3 is the scaphoid, 4 is the lunate, 5 is the triquetral, 6 is the pisiform, 7 is the trapezium, 8 is the trapezoid, 9 is the capitate, 10 is the hamate, 11 is the metacarpal bones, 12 is the proximal phalanx, 13 is the middle phalanx, and 14 is the distal phalanx.
Bones of the left hand. A is the dorsal view, and B is the palmar view. Number 1 is the radius, 2 is the ulna, 3 is the scaphoid, 4 is the lunate, 5 is the triquetral, 6 is the pisiform, 7 is the trapezium, 8 is the trapezoid, 9 is the capitate, 10 is the hamate, 11 is the metacarpal bones, 12 is the proximal phalanx, 13 is the middle phalanx, and 14 is the distal phalanx.
The wrist is the most complex joint in the body. It is formed by eight carpal bones grouped into two rows, with very restricted motion between them. From radial to ulnar, the proximal row consists of the scaphoid, lunate, triquetrum, and pisiform bones. In the same direction, the distal row consists of the trapezium, trapezoid, capitate, and hamate bones.
All carpal bones participate in wrist function except for the pisiform, which is a sesamoid bone through which the flexor carpi ulnaris tendon passes. The scaphoid serves as a link between each row; therefore, it is vulnerable to fractures. The distal row of carpal bones is strongly attached to the base of the second and third metacarpals, forming a fixed unit. All other structures (mobile units) move in relation to this stable unit. The flexor retinaculum, which attaches to the pisiform and hook of hamate ulnarly and to the scaphoid and trapezium radially, forms the roof of the carpal tunnel. The carpal tunnel houses the median nerve and flexor tendons, which are critical for hand function. [8, 9]
The hand contains five metacarpal bones numbered in the radio-ulnar order. [8] Each metacarpal is characterized as having a base, shaft, neck, and head. The first metacarpal bone (thumb) is the shortest and most mobile. It articulates proximally with the trapezium. The other four metacarpals articulate with the trapezoid, capitate, and hamate at the base. Each metacarpal head has a rounded shape that forms the knuckles, with a convex articular surface that interfaces with proximal phalanges at the metacarpophalangeal joints. The bases of metacarpals 2-5 also articulate with each other, enhancing stability. [8, 9]
The hand contains 14 phalanges. Each digit contains three phalanges (proximal, middle, and distal), except for the thumb, which has only two phalanges. To avoid confusion, each digit is referred to by its name (thumb, index, long, ring, and small) rather than a number.
Skin
The skin that covers the dorsum of the hand is greatly different from the skin that covers the palm (see the image below). The skin of the dorsum of the hand is thin and pliable. It is attached to the hand's skeleton only by loose areolar tissue, where lymphatics and veins course. This fact explains why edema of the hand is manifested predominantly at the dorsum. In addition, this loose attachment of skin makes the dorsum of the hand more vulnerable to skin avulsion injuries and permits the creation of local flaps.
The dorsal skin of the hand generally bears hair over the proximal phalanges and the ulnar aspect. [8]
 Surface anatomy of the left hand. A is the dorsum of the left hand, and B is the palm of the left hand. Number 1 is the position of the extensor retinaculum, 2 is the position of the flexor retinaculum, 3 is the position of the head of the metacarpals, 4 is the ulnar artery, 5 is the radial artery, 6 is the level of the deep palmar arch, and 7 is the level of the superficial palmar arch.
Surface anatomy of the left hand. A is the dorsum of the left hand, and B is the palm of the left hand. Number 1 is the position of the extensor retinaculum, 2 is the position of the flexor retinaculum, 3 is the position of the head of the metacarpals, 4 is the ulnar artery, 5 is the radial artery, 6 is the level of the deep palmar arch, and 7 is the level of the superficial palmar arch.
The skin of the palmar surface of the hand is unique, with characteristics for special function. The palmar skin is thick and glabrous and not as pliable as the dorsal skin. It is strongly attached to the underlying fascia by numerous vertical fibers. These features enhance skin stability for proper grasping function.
The palmar skin is devoid of sebaceous glands, although it has numerous nerve endings and eccrine sweat glands. [8] The dense arrangement of collagen fibers in the palmar skin adds strength and limits skin movement, reducing the risk for trauma during repeated mechanical tasks. [10]
The palmar creases are particularly significant for hand function, acting as anchor points where the skin is tightly tethered to deeper tissues, which prevents excessive movement of the skin during flexion and extension of the fingers. [8]
The skin is most firmly anchored to the deep structures at the palmar creases; this is of clinical importance when planning surgical incisions to minimize skin contractures. In contrast to the dorsal skin, the blood supply to the palmar skin is through numerous small, vertical branches from the common digital vessels. Therefore, the elevation of palmar skin flaps is limited. Finally, the skin of the palmar surface of the hand contains a high concentration of sensory nerve organs essential to the hand's normal function.
Nails
The nails are specialized skin appendages derived from the epidermis, primarily composed of keratin-filled squames arranged in 2-3 layers. [8]
The nail consists of:
Nail plate: It is the visible hard part of the nail, which is typically about half a millimeter thick. It is primarily formed by the nail matrix, which produces keratin that makes up approximately 90% of the nail plate's volume. [11] Ninety percent of the nail plate is produced by the germinal matrix, which approximately corresponds to the lunula (pale semicircle in proximal nail bed).
Nail bed: It is the skin beneath the nail plate, which supports it and contains blood vessels that contribute to its pink coloration. [8, 11] The nail bed has a germinal matrix, sterile matrix, and hyponychium.
This germinal matrix starts proximally at the base of the distal phalanx just distal to the insertion of the extensor tendon. The germinal matrix plays a central role in the nail's regenerative capabilities. The cells of this matrix undergo rapid mitosis, which contributes to nail growth. [12]
The sterile matrix is distal to the lunula; it is very vascular, which accounts for the pink color. The sterile matrix produces 10% of the nail plate volume and adds squamous components, which make the nail stronger and adherent to the nail bed.
The hyponychium, located beneath the free edge of the nail plate, serves as a crucial barrier against infections. It is the epidermal ridge forming the junction between the finger pulp and the subungual structures. It tightly adheres to the distal nail plate, reinforcing the nail's resistance to detachment and microbial invasion. Besides being rich in immune cells such as neutrophils and Langerhans cells, this adherence makes the hyponychium crucial for immune defense. [13, 14]
The entire nail matrix is in intimate contact with the periosteum of the distal phalanx; therefore, it is vulnerable to injury when the latter is fractured. Studies have demonstrated that the nail matrix, especially the germinal matrix, contains stem cell populations that are crucial for nail regrowth and repair after injury. Additionally, the Want signaling pathway has been implicated in regulating nail growth and regeneration, offering potential therapeutic avenues for nail disorders. [15]
Nail growth occurs at an average rate of about 3 millimeters per month for fingernails, with toenails growing slightly slower. The matrix continuously produces new keratin, pushing older cells forward to form the nail plate. [11]
Palmar Fascia and Deep Compartments
The palmar fascia consists of a resistant fibrous tissue arranged in longitudinal, transverse, oblique, and vertical fibers. This arrangement plays a crucial role in the function and stability of the hand. [8]
The longitudinal fibers originate at the wrist from the palmaris longus tendon when present or the flexor retinaculum of the wrist when the palmaris longus is absent. [8] These fibers spread out to the base of each digit, where minor fibers extend distally and attach to tissues. This arrangement of fibers forms the fibrous flexor sheath and pulley system of each digit (see the image below).
Studies highlight the importance of these fibers in maintaining the integrity of the flexor tendons during movement and in pathologic conditions such as Dupuytren's contracture. Research has shown that alterations in the collagen composition and inflammatory markers within these fibers can significantly affect hand function and disease progression. [16]
 Subcutaneous structures of the left hand. A is the dorsum of the left hand, and B is the palm of the left hand. Number 1 is the deep antebrachial fascia, 2 is the superficial fascia and dorsal venous network of the hand, 3 is the palmar aponeurosis, 4 is the thenar muscles, 5 is the hypothenar muscles, 6 is the palmaris brevis, 7 is the cephalic vein, and 8 is the basilic vein.
Subcutaneous structures of the left hand. A is the dorsum of the left hand, and B is the palm of the left hand. Number 1 is the deep antebrachial fascia, 2 is the superficial fascia and dorsal venous network of the hand, 3 is the palmar aponeurosis, 4 is the thenar muscles, 5 is the hypothenar muscles, 6 is the palmaris brevis, 7 is the cephalic vein, and 8 is the basilic vein.
The transverse fibers are concentrated in the mid palm and web spaces. They are closely associated with the longitudinal fibers and serve as pulleys for the flexor tendons proximal to the digital pulleys. These fibers, along with the superficial transverse metacarpal (natatory) ligament, and the deep transverse metacarpal ligament form the transverse fiber system. [8] The transverse fibers play a crucial role in stabilizing the flexor tendons and contribute to the formation of the palmar pulley system. This pulley mechanism prevents the "bowstringing" of the tendons, ensuring that a proper flexion force is transmitted through the digits. This organization is vital for coordinated finger movements and grip strength. [17, 18]
The vertical fibers (of Grapow) of the palmar fascia are comparatively delicate. [8] They attach to the dermis of the palmar skin. Deep to the longitudinal and transverse fibers, the vertical fibers coalesce into septa and attach to the metacarpals, forming eight different compartments for the flexor tendons and neurovascular bundles of each digit. These compartments protect and compartmentalize important structures such as the flexor tendons, lumbrical muscles, and digital nerves, allowing for independent and controlled motion of each digit. [8, 17, 18]
A common central compartment is located proximal in the palm. The digits contain two fascial bands of clinical importance. These are the Grayson ligament and the Cleland ligament, which are located volar and dorsal to the neurovascular bundle of each digit, respectively.
Knowledge of the anatomy of the palmar fascial fibers and deep compartments is crucial for the identification of structures during procedures such as palmar fasciectomy for Dupuytren disease.
Nerves
As previously mentioned, the hand is innervated by three nerves: the median, ulnar, and radial. Each has sensory and motor components. Variations from the classic nerve distribution are so common that they are the rule rather than the exception. [19] The skin of the forearm is innervated medially by the medial antebrachial cutaneous nerve and laterally by the lateral antebrachial cutaneous nerve (see the image below).
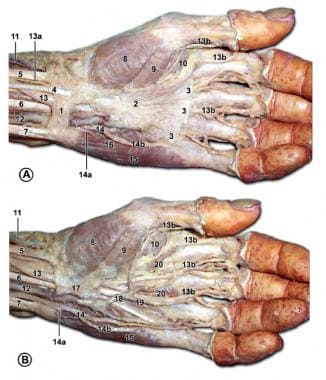
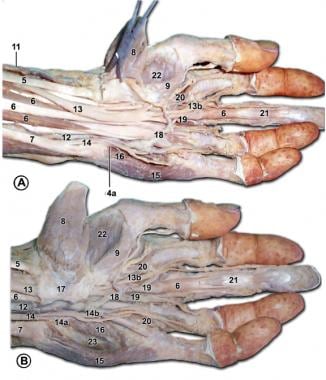 Palmar structures of the left hand. In A, the flexor retinaculum is removed. In B, the flexor retinaculum is intact. Number 5 is the flexor carpi radialis, 6 is the flexor digitorum superficialis, 7 is the flexor carpi ulnaris, 8 is the abductor pollicis brevis, 9 is the flexor pollicis brevis, 11 is the radial artery, 12 is the ulnar artery, 13 is the median nerve, 13B is the digital branches of median nerve, 14 is the ulnar nerve, 14A is the deep branch of the ulnar nerve, 14B is the digital branch of the ulnar nerve, 15 is the abductor digiti minimi, 16 is the flexor digiti minimi, 17 is the flexor retinaculum, 18 is the superficial palmar arch, 19 is the common palmar digital artery, 20 is the lumbricals, 21 is the flexor digitorum profundus, 22 is the opponens pollicis, and 23 is the opponens digiti minimi.
Palmar structures of the left hand. In A, the flexor retinaculum is removed. In B, the flexor retinaculum is intact. Number 5 is the flexor carpi radialis, 6 is the flexor digitorum superficialis, 7 is the flexor carpi ulnaris, 8 is the abductor pollicis brevis, 9 is the flexor pollicis brevis, 11 is the radial artery, 12 is the ulnar artery, 13 is the median nerve, 13B is the digital branches of median nerve, 14 is the ulnar nerve, 14A is the deep branch of the ulnar nerve, 14B is the digital branch of the ulnar nerve, 15 is the abductor digiti minimi, 16 is the flexor digiti minimi, 17 is the flexor retinaculum, 18 is the superficial palmar arch, 19 is the common palmar digital artery, 20 is the lumbricals, 21 is the flexor digitorum profundus, 22 is the opponens pollicis, and 23 is the opponens digiti minimi.
Median nerve
The median nerve is responsible for innervating the muscles involved in the fine precision and pinch function of the hand. It originates from the lateral and medial cords of the brachial plexus (C5-T1). In the forearm, the motor branches supply the pronator teres, flexor carpi radialis, palmaris longus, and flexor digitorum superficialis muscles. The anterior interosseus branch innervates the flexor pollicis longus, flexor digitorum profundus (index and long finger), and pronator quadratus muscles.
Proximal to the wrist, the palmar cutaneous branch provides sensation at the thenar eminence. As the median nerve passes through the carpal tunnel, the recurrent motor branch innervates the thenar muscles (abductor pollicis brevis, opponens pollicis, and superficial head of flexor pollicis brevis). It also innervates the index and long finger lumbrical muscles. Sensory digital branches provide sensation to the thumb, index finger, long finger, and radial side of the ring finger.
Studies have highlighted anatomical variations in the branching patters of the median nerve. For instance, division of the median nerve proximal to the carpal tunnel is called a bifid median nerve. It may be associated with carpal tunnel syndrome and persistent median vessels. [20]
Ulnar nerve
The ulnar nerve is responsible for innervating the muscles involved in the power grasp function of the hand. Studies also highlight its role in fine motor control in addition to the power grasp function. [8] It originates at the medial cord of the brachial plexus (C8-T1). Motor branches innervate the flexor carpi ulnaris and flexor digitorum profundus muscles to the ring and small fingers. Proximal to the wrist, the palmar cutaneous branch provides sensation at the hypothenar eminence. The dorsal branch, which branches from the main trunk at the distal forearm, provides sensation to the ulnar portion of the dorsum of the hand and small finger and part of the ring finger.
In the hand, the superficial branch forms the digital nerves, which provide sensation at the small finger and ulnar aspect of the ring finger. The deep motor branch passes through the Guyon canal in company with the ulnar artery. It innervates the hypothenar muscles (abductor digiti minimi, opponens digiti minimi, flexor digiti minimi, and palmaris brevis), all interossei, the two ulnar lumbricals, the adductor pollicis, and the deep head of the flexor pollicis brevis.
Findings indicate the prevalence of variations in the ulnar nerve anatomy. A study reported that 10% of the examined limbs displayed significant variations in the ulnar nerve structure that could complicate surgical interventions. [20]
Radial nerve
The radial nerve is responsible for innervating the wrist extensors, which control the position of the hand and stabilize the fixed unit. It originates from the posterior cord of the brachial plexus (C6-8). At the elbow, motor branches innervate the brachioradialis and extensor carpi radialis longus muscles.
At the proximal forearm, the radial nerve divides into the superficial and deep branches. The deep posterior interosseous branch innervates all the muscles in the extensor compartment: supinator, extensor carpi radialis brevis, extensor digitorum communis, extensor digiti minimi, extensor carpi ulnaris, extensor indicis proprius, extensor pollicis longus, extensor pollicis brevis, and abductor pollicis longus.
The superficial branch provides sensation at the radial aspect of the dorsum of the hand; the dorsum of the thumb; and the dorsum of the index finger, long finger, and radial half of the ring finger proximal to the distal interphalangeal joints.
Muscles and Tendons
The muscles of the hand are divided into intrinsic and extrinsic groups. The intrinsic muscles are located within the hand itself, whereas the extrinsic muscles are located proximally in the forearm and insert to the hand skeleton by long tendons. [21]
Extrinsic extensors
The extensor muscles are all extrinsic, except for the interosseous-lumbrical complex, which is involved in interphalangeal joint extension. All the extrinsic extensor muscles are innervated by the radial nerve. This group of muscles consists of three wrist extensors and a larger group of thumb and digit extensors (see the image below). [22]
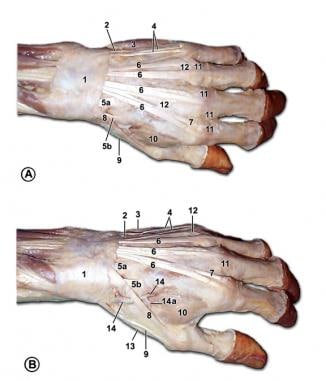 Muscles and tendons of the dorsum of the left hand. Number 1 is the extensor retinaculum, 2 is the extensor carpi ulnaris, 3 is the abductor digiti minimi, 4 is the extensor digiti minimi, 5A is the extensor carpi radialis brevis, 5B is the extensor carpi radialis longus, 6 is the extensor digitorum, 7 is the extensor indicis, 8 is the extensor pollicis longus, 9 is the extensor pollicis brevis, 10 is the first dorsal interosseus, 11 is the extensor expansion, 12 is the intertendinous connections, 13 is the abductor pollicis longus, 14 is the radial artery, and 14A is the princeps pollicis artery.
Muscles and tendons of the dorsum of the left hand. Number 1 is the extensor retinaculum, 2 is the extensor carpi ulnaris, 3 is the abductor digiti minimi, 4 is the extensor digiti minimi, 5A is the extensor carpi radialis brevis, 5B is the extensor carpi radialis longus, 6 is the extensor digitorum, 7 is the extensor indicis, 8 is the extensor pollicis longus, 9 is the extensor pollicis brevis, 10 is the first dorsal interosseus, 11 is the extensor expansion, 12 is the intertendinous connections, 13 is the abductor pollicis longus, 14 is the radial artery, and 14A is the princeps pollicis artery.
The extensor carpi radialis brevis (ECRB) is the main extensor of the wrist, along with the extensor carpi radialis longus (ECRL) and extensor carpi ulnaris (ECU), which also deviate the wrist radially and ulnarly, respectively. The ECRB inserts at the base of the third metacarpal, while the ECRL and ECU insert at the base of the second and fifth metacarpal, respectively.
The extensor digitorum communis, extensor indicis proprius, and extensor digiti minimi extend the digits. They insert to the base of the middle phalanges as central slips and to the base of the distal phalanges as lateral bands. The abductor pollicis longus, extensor pollicis brevis, and extensor pollicis longus extend the thumb. They insert at the base of the thumb metacarpal, proximal phalanx, and distal phalanx, respectively.
The extensor retinaculum prevents the bowstringing of tendons at the wrist level and separates the tendons into six compartments. The extensor digitorum communis is a series of tendons to each digit with a common muscle belly and with intertendinous bridges between them. The index and small finger each have an independent extension function through the extensor indicis proprius and extensor digiti minimi.
Extrinsic flexors
The extrinsic flexors consist of three wrist flexors and a larger group of thumb and digit flexors. They are innervated by the median nerve, except for the flexor carpi ulnaris (FCU) and the flexor digitorum profundus to the small and ring finger, which are innervated by the ulnar nerve (see the image below).
 Palmar structures of the left hand. In A, the palmar aponeurosis is intact. In B, the palmar aponeurosis is removed. Number 1 is the deep antebrachial fascia, 2 is the palmar aponeurosis, 3 is the superficial transverse metacarpal ligaments, 4 is the palmaris longus, 5 is the flexor carpi radialis, 6 is the flexor digitorum superficialis, 7 is the flexor carpi ulnaris, 8 is the abductor pollicis brevis, 9 is the flexor pollicis brevis, 10 is the adductor pollicis, 11 is the radial artery, 12 is the ulnar artery, 13 is the median nerve, 13B is the digital branches of the median nerve, 14 is the ulnar nerve, 14A is the deep branch of the ulnar nerve, 14B is the digital branch of the ulnar nerve, 15 is the abductor digiti minimi, 16 is the flexor digiti minimi, 17 is the flexor retinaculum, 18 is the superficial palmar arch, 19 is the common palmar digital artery, and 20 is the lumbricals.
Palmar structures of the left hand. In A, the palmar aponeurosis is intact. In B, the palmar aponeurosis is removed. Number 1 is the deep antebrachial fascia, 2 is the palmar aponeurosis, 3 is the superficial transverse metacarpal ligaments, 4 is the palmaris longus, 5 is the flexor carpi radialis, 6 is the flexor digitorum superficialis, 7 is the flexor carpi ulnaris, 8 is the abductor pollicis brevis, 9 is the flexor pollicis brevis, 10 is the adductor pollicis, 11 is the radial artery, 12 is the ulnar artery, 13 is the median nerve, 13B is the digital branches of the median nerve, 14 is the ulnar nerve, 14A is the deep branch of the ulnar nerve, 14B is the digital branch of the ulnar nerve, 15 is the abductor digiti minimi, 16 is the flexor digiti minimi, 17 is the flexor retinaculum, 18 is the superficial palmar arch, 19 is the common palmar digital artery, and 20 is the lumbricals.
The flexor carpi radialis is the main flexor of the wrist, along with the flexor carpi ulnaris and the palmaris longus, which is absent in 15% of the population. They insert at the base of the third metacarpal, the base of the fifth metacarpal, and the palmar fascia, respectively. The FCU is primarily an ulnar deviator. The eight digital flexors are divided into superficial and deep groups. Along with the flexor pollicis longus, which inserts at the thumb distal phalanx, they pass through the carpal tunnel to provide flexion at the interphalangeal joints.
In the palm, the flexor digitorum superficialis tendon lies volar to the profundus tendon. It then splits at the level of the proximal phalanx and reunites dorsal to the profundus tendon to insert in the middle phalanx. The flexor digitorum profundus perforates the superficialis tendon to insert at the distal phalanx. The relationship of flexor tendons with the wrist joint, metacarpophalangeal joint, and interphalangeal joint is maintained by a retinacular or pulley system that prevents the bowstringing effect.
Intrinsics
The intrinsic muscles are situated totally within the hand. They are divided into four groups: the thenar, hypothenar, lumbrical, and interossei muscles.
The thenar group consists of the abductor pollicis brevis, flexor pollicis brevis, opponens pollicis, and adductor pollicis muscles. All are innervated by the median nerve, except for the adductor pollicis and deep head of the flexor pollicis brevis, which are innervated by the ulnar nerve. They originate from the flexor retinaculum and carpal bones and insert at the thumb's proximal phalanx.
The hypothenar group consists of the palmaris brevis, abductor digiti minimi, flexor digiti minimi, and opponens digiti minimi. They are all innervated by the ulnar nerve. This group of muscles originates at the flexor retinaculum and carpal bones and inserts at the base of the proximal phalanx of the small finger.
The lumbrical muscles contribute to the flexion of the metacarpophalangeal joints and to the extension of the interphalangeal joints. They originate from the flexor digitorum profundus tendons at the palm and insert on the radial aspect of the extensor tendons at the digits. The index and long finger lumbricals are innervated by the median nerve, and the small and ring finger lumbricals are innervated by the ulnar nerve. [23]
The interossei group consists of three volar and four dorsal muscles, which are all innervated by the ulnar nerve. They originate at the metacarpals and form lateral bands with the lumbricals. The dorsal interossei abduct the fingers, whereas the volar interossei adduct the fingers to the hand axis.
Joints
The wrist joint is a complex, multiarticulated joint that allows a wide range of motion in flexion, extension, circumduction, radial deviation, and ulnar deviation.
The distal radioulnar joint allows pronation and supination of the hand as the radius rotates around the ulna. Studies emphasize the importance of the triangular fibrocartilage complex (TFCC) in stabilizing the distal radioulnar joint, particularly during rotational movements. Injuries to the TFCC may result in instability or loss of motion of this joint. [24]
The radiocarpal joint includes the proximal carpal bones and the distal radius. The proximal row of carpals articulates with the radius and ulna to provide extension, flexion, ulnar deviation, and radial deviation. This joint is supported by an extrinsic set of strong palmar ligaments that arise from the radius and ulna. Dorsally, it is supported by the dorsal intercarpal ligament between the scaphoid and triquetrum and by the dorsal radiocarpal ligament.
At the intercarpal joints, motion between carpal bones is very restricted. These joints are supported by strong intrinsic ligaments. The two most important ones are the scapholunate ligament and the lunotriquetral ligament. Disruption of either one can result in wrist instability.
The three Gilula lines have been described to represent the smooth contour of a greater arc formed by the proximal carpal bones and a lesser arc formed by the distal carpal bones in normal anatomy.
All four distal carpal bones articulate with the metacarpals at the carpometacarpal (CMC) joints. The second and third CMC joints form a fixed unit, while the first CMC forms the most mobile joint.
At the metacarpophalangeal joints, lateral motion is limited by the collateral ligaments, which are actually lateral oblique in position rather than true lateral. This arrangement and the shape of the metacarpal head allow the ligaments to be tight when the joint is flexed and loose when extended (i.e., cam effect). The volar plate is part of the joint capsule that attaches only to the proximal phalanx, allowing for hyperextension. The volar plate is the site of insertion for the intermetacarpal ligaments. These ligaments restrict the separation of the metacarpal heads.
At the interphalangeal joints, extension is limited by the volar plate, which attaches to the phalanges at each side of the joint. Radial and ulnar motion is restricted by collateral ligaments, which remain tight through their whole range of motion. Knowledge of these configurations is of critical when splinting a hand to avoid joint contractures.
Blood Supply
The hand has a complex and rich vascular network. The radial and ulnar arteries, which are branches of the brachial artery, supply blood to the hand. Supplemental arteries in the forearm include the anterior interosseous artery, the posterior interosseus artery, and (occasionally) the median artery, all of which are branches of the ulnar artery. [21]
The radial artery runs distally in the forearm between the brachioradialis and flexor carpi radialis muscles. At the wrist, it crosses dorsally deep to the tendons of the "anatomic snuffbox" to enter the palm and form the deep palmar arch. A superficial branch arises at the level of the wrist and contributes to the superficial palmar arch. [25]
The radial artery supplies blood to: [26]
-
The thumb via the princeps pollicis artery
-
The radial aspect of the index finger through the radialis indicis artery
The ulnar artery runs distally in the forearm under the flexor carpi ulnaris muscle. In the wrist, it travels into the hand through the Guyon canal, where it divides into the deep palmar branch and the superficial palmar branch. The superficial branch forms the superficial palmar arch and the deep branch contributes to the deep palmar arch. [27]
The superficial palmar arch lies directly deep to the palmar fascia. It gives rise to the volar common digital arteries and multiple branches to intrinsic muscles and skin. Distal in the palm, the common digital arteries bifurcate into the proper digital arteries. In the palm, the arteries lie volar to the corresponding nerves, a relation that is reversed in the digits. At the digits, the neurovascular bundle always lies volar to the ligament of Cleland. This pattern protects the bundle and can serve as a guide for their surgical dissection.
The deep palmar arch lies at the base of the metacarpals deep to the flexor tendons. It is the major blood supply to the thumb and radial half of the index finger by the first metacarpal artery. After giving its branch to the index finger, it is called the princeps pollicis.
The dorsal arteries originate proximally from the posterior interosseous artery and a dorsal perforating branch of the anterior interosseous artery. Dorsal metacarpal arteries arise from a dorsal carpal arch formed by the previously mentioned arteries and are the source of multiple local hand flaps (dorsal metacarpal artery flaps). These dorsal metacarpal arteries are found more reliably for the first and second metacarpals and then for the third and fourth.
Common digital arteries arise from the superficial palmar arch to form proper digital arteries at the webs. The palmar aspect of the digits receives arterial flow through these proper digital arteries. The dorsum of each digit, distal to the proximal interphalangeal joint, is vascularized by dorsal branches of the proper digital arteries.
Veins generally follow the deep arterial system as venae comitantes. A superficial venous system also exists at the dorsum of the hand and contributes to the cephalic and basilic veins in the upper extremity.
Pulley
The pulley system is critical to flexion of the finger. The retinacular system for each of the fingers contains five annular pulleys and four cruciate pulleys. [28] The thumb has two annular pulleys and one oblique pulley. In the finger, the second and fourth annular pulleys (A2, A4) are critical pulleys. The oblique pulley is the critical pulley in the thumb.
The retinacular system ensures that the flexor tendons glide smoothly during finger movements, preventing bowstringing — where tendons pull away from their intended path, reducing mechanical efficiency and strength during flexion. [29]
Deficiency of the pulley system can result in less active flexion of the digits for a certain tendon excursion. If the critical pulleys are missing as a result of injury, the moment arm of the flexor tendon-to-bone relationship is increased, resulting in the need for more tendon excursion to flex the finger.
Studies indicate that while complete ruptures of critical pulleys necessitate surgical intervention, partial injuries may be managed conservatively without a significant loss of function. [30]
-
Surface anatomy of the left hand. A is the dorsum of the left hand, and B is the palm of the left hand. Number 1 is the position of the extensor retinaculum, 2 is the position of the flexor retinaculum, 3 is the position of the head of the metacarpals, 4 is the ulnar artery, 5 is the radial artery, 6 is the level of the deep palmar arch, and 7 is the level of the superficial palmar arch.
-
Bones of the left hand. A is the dorsal view, and B is the palmar view. Number 1 is the radius, 2 is the ulna, 3 is the scaphoid, 4 is the lunate, 5 is the triquetral, 6 is the pisiform, 7 is the trapezium, 8 is the trapezoid, 9 is the capitate, 10 is the hamate, 11 is the metacarpal bones, 12 is the proximal phalanx, 13 is the middle phalanx, and 14 is the distal phalanx.
-
Subcutaneous structures of the left hand. A is the dorsum of the left hand, and B is the palm of the left hand. Number 1 is the deep antebrachial fascia, 2 is the superficial fascia and dorsal venous network of the hand, 3 is the palmar aponeurosis, 4 is the thenar muscles, 5 is the hypothenar muscles, 6 is the palmaris brevis, 7 is the cephalic vein, and 8 is the basilic vein.
-
Muscles and tendons of the dorsum of the left hand. Number 1 is the extensor retinaculum, 2 is the extensor carpi ulnaris, 3 is the abductor digiti minimi, 4 is the extensor digiti minimi, 5A is the extensor carpi radialis brevis, 5B is the extensor carpi radialis longus, 6 is the extensor digitorum, 7 is the extensor indicis, 8 is the extensor pollicis longus, 9 is the extensor pollicis brevis, 10 is the first dorsal interosseus, 11 is the extensor expansion, 12 is the intertendinous connections, 13 is the abductor pollicis longus, 14 is the radial artery, and 14A is the princeps pollicis artery.
-
Palmar structures of the left hand. In A, the palmar aponeurosis is intact. In B, the palmar aponeurosis is removed. Number 1 is the deep antebrachial fascia, 2 is the palmar aponeurosis, 3 is the superficial transverse metacarpal ligaments, 4 is the palmaris longus, 5 is the flexor carpi radialis, 6 is the flexor digitorum superficialis, 7 is the flexor carpi ulnaris, 8 is the abductor pollicis brevis, 9 is the flexor pollicis brevis, 10 is the adductor pollicis, 11 is the radial artery, 12 is the ulnar artery, 13 is the median nerve, 13B is the digital branches of the median nerve, 14 is the ulnar nerve, 14A is the deep branch of the ulnar nerve, 14B is the digital branch of the ulnar nerve, 15 is the abductor digiti minimi, 16 is the flexor digiti minimi, 17 is the flexor retinaculum, 18 is the superficial palmar arch, 19 is the common palmar digital artery, and 20 is the lumbricals.
-
Palmar structures of the left hand. In A, the flexor retinaculum is removed. In B, the flexor retinaculum is intact. Number 5 is the flexor carpi radialis, 6 is the flexor digitorum superficialis, 7 is the flexor carpi ulnaris, 8 is the abductor pollicis brevis, 9 is the flexor pollicis brevis, 11 is the radial artery, 12 is the ulnar artery, 13 is the median nerve, 13B is the digital branches of median nerve, 14 is the ulnar nerve, 14A is the deep branch of the ulnar nerve, 14B is the digital branch of the ulnar nerve, 15 is the abductor digiti minimi, 16 is the flexor digiti minimi, 17 is the flexor retinaculum, 18 is the superficial palmar arch, 19 is the common palmar digital artery, 20 is the lumbricals, 21 is the flexor digitorum profundus, 22 is the opponens pollicis, and 23 is the opponens digiti minimi.