Rectus capitis posterior minor muscle
| Rectus capitis posterior minor muscle | |
|---|---|
 Human skull seen from back (rectus capitis posterior minor shown in red.) | |
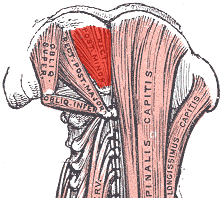 Deep muscles of the back. (rectus capitis posterior minor labeled at top center.) | |
| Details | |
| Origin | Tubercle on the posterior arch of the atlas |
| Insertion | Medial part of the inferior nuchal line of the occipital bone and the surface between it and the foramen magnum |
| Nerve | Branch of the dorsal primary division of the suboccipital nerve |
| Actions | Extends the head at the neck, but is now considered to be more of a sensory organ than a muscle |
| Identifiers | |
| Latin | musculus rectus capitis posterior minor |
| TA98 | A04.2.02.005 |
| TA2 | 2250 |
| FMA | 32526 |
| Anatomical terms of muscle | |
The rectus capitis posterior minor (or rectus capitis posticus minor[citation needed]) is a muscle in the upper back part of the neck. It is one of the suboccipital muscles. Its inferior attachment is at the posterior arch of atlas; its superior attachment is onto the occipital bone at and below the inferior nuchal line. The muscle is innervated by the suboccipital nerve (the posterior ramus of first cervical spinal nerve). The muscle acts as a weak extensor of the head.
Anatomy
The rectus capitis posterior major muscle is one of the suboccipital muscles.[1]
The muscle extends vertically superior-ward from its inferiro attachment to its superior attachment.[2] The muscle becomes broader superiorly.[1]
Attachments
The inferior attachment is (by a narrow tendon) onto the posterior tubercle[1] of the posterior arch of atlas.[2]
Its superior attachment is onto the medial portion of the inferior nuchal line[1] and the external surface of the occipital bone inferior to it[2][1] (between this line superiorly and the foramen magnum inferiorly[1]).
The muscle usually also additionally attaches onto the posterior atlantooccipital membrane (which is in turn attached onto adjacent dura mater of the spinal canal).[1]
Innervation
The muscle receives motor innervation from the suboccipital nerve (the posterior ramus of cervical spinal nerve C1).[2][1]
Variation
The muscle of either side may be doubled (along its length).[1]
Actions/movements
The muscle is a weak[2] extensor of the head.[2][1]
The synergists are the rectus capitis posterior major and the obliquus capitis superior.[citation needed]
Research
Role in headache
Connective tissue bridges were noted at the atlanto-occipital joint between the rectus capitis posterior minor (RCPm) muscle and the dorsal spinal dura.[3] Similar connective tissue connections of the rectus capitis posterior major have been reported recently as well.[4] The perpendicular arrangement of these fibers appears to restrict dural movement toward the spinal cord. The ligamentum nuchae was found to be continuous with the posterior cervical spinal dura and the lateral portion of the occipital bone. Anatomic structures innervated by cervical nerves C1-C3 have the potential to cause headache pain. Included are the joint complexes of the upper three cervical segments, the dura mater, and spinal cord.[citation needed]
The dura-muscular (myodural) and dura-ligamentous connections in the upper cervical spine and occipital areas may provide anatomic and physiologic answers to the cause of the cervicogenic headache.[5] The level of strain at which RCPm muscle fibers began to tear as a result of overstretching has been estimated to be 30%.[6] This would be expected to put them at risk of injury during whiplash-type distortions when the occipitoatlantal (OA) joint is flexed upon impact.[7] Tearing of the muscle fibers would result in fatty infiltration (FI) that would be expected to impact the functional relationship between the RCPm muscles and the pain sensitive spinal dura.[8] While FI and/or a reduction in the cross sectional area (CSA) of active muscle would not be expected to be the direct cause of chronic headache, it is known that muscle pathology will result in functional deficits. Pathologies in RCPm muscles in conjunction with the myodural bridge can compromise the normal functional relationship between the RCPm and the pain sensitive dura mater[9] and result in referred head and neck pain. This could help to explain manipulation's efficacy in the treatment of cervicogenic headache.[citation needed]
Additional images
-
Position of rectus capitis posterior minor muscle (shown in red). Animation.
-
Lateral view of human skull (rectus capitis posterior minor shown in red.)
-
Occipital bone. Outer surface.
See also
- Atlanto-occipital joint
- Rectus capitis lateralis
- Rectus capitis posterior major muscle
- Rectus capitis anterior muscle
References
![]() This article incorporates text in the public domain from page 401 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 401 of the 20th edition of Gray's Anatomy (1918)
- ^ a b c d e f g h i j Standring, Susan (2020). Gray's Anatomy: The Anatomical Basis of Clinical Practice (42th ed.). New York. pp. 848–849. ISBN 978-0-7020-7707-4. OCLC 1201341621.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ a b c d e f Sinnatamby, Chummy S. (2011). Last's Anatomy (12th ed.). Elsevier Australia. p. 430. ISBN 978-0-7295-3752-0.
- ^ Hack, Gary D.; Koritzer, Richard T.; Robinson, Walker L.; Hallgren, Richard C.; Greenman, Philip E. "Anatomic Relation between the Rectus Capitis Posterior Minor Muscle and the Dura Mater". Spine. 20 (23): 2484. ISSN 0362-2436.
- ^ Scali, Frank; Marsili, Eric S.; Pontell, Matthew E. (2011-12-01). "Anatomical Connection Between the Rectus Capitis Posterior Major and the Dura Mater". Spine. 36 (25): E1612. doi:10.1097/BRS.0b013e31821129df. ISSN 0362-2436.
- ^ Gary D. Hack; Peter Ratiu; John P. Kerr; Gwendolyn F. Dunn; Mi Young Toh. "Visualization of the Muscle-Dural Bridge in the Visible Human Female Data Set". The Visible Human Project, National Library of Medicine.
- ^ Hallgren, Richard C. (2017-02-01). "Injury Threshold of Rectus Capitis Muscles at the Atlanto-occipital Joint". Journal of Manipulative and Physiological Therapeutics. 40 (2): 71–76. doi:10.1016/j.jmpt.2016.11.001. ISSN 0161-4754.
- ^ Grauer, Jonathan N.; Panjabi, Manohar M.; Cholewicki, Jacek; Nibu, Kimio; Dvorak, Jiri (1997-11-01). "Whiplash Produces an S-Shaped Curvature of the Neck With Hyperextension at Lower Levels". Spine. 22 (21): 2489. ISSN 0362-2436.
- ^ Kong, Andrew; Van der Vliet, Andrew; Zadow, Steven (2007-07-01). "MRI and US of gluteal tendinopathy in greater trochanteric pain syndrome". European Radiology. 17 (7): 1772–1783. doi:10.1007/s00330-006-0485-x. ISSN 1432-1084.
- ^ Enix, Dennis E.; Scali, Frank; Pontell, Matthew E. (June 2014). "The cervical myodural bridge, a review of literature and clinical implications". The Journal of the Canadian Chiropractic Association. 58 (2): 184–192. ISSN 0008-3194. PMC 4025088. PMID 24932022.
External links
- Anatomy figure: 01:07-01 at Human Anatomy Online, SUNY Downstate Medical Center
- Anatomy photo:01:10-0101 at the SUNY Downstate Medical Center
- PTCentral
- CS1 maint: location missing publisher
- Articles with short description
- Short description with empty Wikidata description
- All articles with unsourced statements
- Articles with unsourced statements from August 2023
- Wikipedia articles incorporating text from the 20th edition of Gray's Anatomy (1918)
- Commons category link is on Wikidata
- Muscles of the head and neck



