Adenoid cystic carcinoma
| Adenoid cystic carcinoma | |
|---|---|
| Other names | Adenocyst, Malignant cylindroma, Adenocystic, Adenoidcystic |
 | |
| Micrograph of an adenoid cystic carcinoma of a salivary gland (right of image): Normal serous glands, typical of the parotid gland, are also seen (left of image), H&E stain. | |
| Specialty | Oncology |
Adenoid cystic carcinoma is a rare type of cancer that can exist in many different body sites. This tumor most often occurs in the salivary glands, but it can also be found in many anatomic sites, including the breast,[1][2] lacrimal gland, lung, brain, Bartholin gland, trachea, and the paranasal sinuses.
It is the third-most common malignant salivary gland tumor overall (after mucoepidermoid carcinoma and polymorphous adenocarcinoma). It represents 28% of malignant submandibular gland tumors, making it the single most common malignant salivary gland tumor in this region. Patients may survive for years with metastases because this tumor is generally well-differentiated and slow growing. In a 1999 study[3] of a cohort of 160 ACC patients, disease-specific survival was 89% at 5 years, but only 40% at 15 years,[citation needed] reflecting deaths from late-occurring metastatic disease.
Cause
Activation of the oncogenic transcription factor gene MYB is the key genomic event of ACC and seen in the vast majority of cases.[4][5] Most commonly, MYB is activated through gene fusion with the transcription factor encoding NFIB gene as a result of a t(6;9) translocation.[4] Alternatively, MYB is activated by copy number gain or by juxtaposition of enhancer elements in the vicinity of the MYB gene.[6] In a subset of ACCs, the closely related MYBL1 gene is fused to NFIB or to other fusion partners.[7][8]
MYB drives proliferation of ACC cells and regulates genes involved in cell cycle control, DNA replication and repair, and RNA processing.[9] Thus, the MYB oncogene is a potential diagnostic and therapeutic target in ACC.
ACC has a relatively quiet genome with few recurrent copy number alterations or point mutations,[6][10][11][12] consistent with the view that MYB and MYBL1 are the main oncogenic drivers of the disease.
Treatment
Primary treatment for this cancer, regardless of body site, is surgical removal with clean margins. This surgery can prove challenging in the head and neck region due to this tumor's tendency to show a perineural discontinuous growth, meaning that it follows nerves and different "nests" of the tumor can exist without a connection to the original tumor. Therefore, MRI-images should be analysed following nerve tracts up to the brainstem. Adjuvant or palliative radiotherapy is commonly given following surgery. For advanced major and minor salivary gland tumors that are inoperable, recurrent, or exhibit gross residual disease after surgery, fast neutron therapy is widely regarded as the most effective form of treatment.[13][14][15][16] Chemotherapy is used for metastatic disease. Chemotherapy is considered on a case-by-case basis, as data on the positive effects of chemotherapy are limited. Clinical studies are ongoing, however.[citation needed]
Images
-
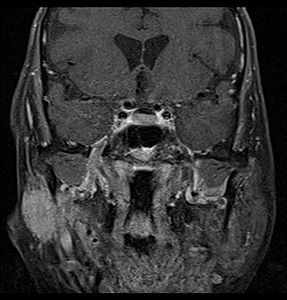
Coronal MRI showing right parotid adenoid cystic carcinoma with perineural spread of tumor: The tumor originates in the right parotid gland and spreads along the trigeminal nerve via the auricuotemporal branch extending intracranially through the foramen ovale at the skull base towards Meckel's cave.
-
Coronal MRI showing right parotid adenoid cystic carcinoma with perineural spread of tumor along the facial nerve extending to the stylomastoid foramen
-
Histopathological image of adenoid cystic carcinoma of the salivary gland infiltrating a nerve (center), H&E stain
-
Histopathological image of adenoid cystic carcinoma of the salivary gland, immunostain for S-100 protein
-
Micrograph of adenoid cystic carcinoma, fine needle aspiration specimen, Pap stain
-
Adenoid cystic carcinoma with comedonecrosis
-
Relative incidence of submandibular tumors, with adenoid cystic carcinoma being the second most common.[17]
-
Relative incidence of parotid tumors, with adenoid cystic carcinoma being relatively rare.[17]
See also
References
- ^ Marchiò C, Weigelt B, Reis-Filho JS (Mar 2010). "Adenoid cystic carcinomas of the breast and salivary glands (or 'The strange case of Dr Jekyll and Mr Hyde' of exocrine gland carcinomas)". J Clin Pathol. 63 (3): 220–8. doi:10.1136/jcp.2009.073908. PMID 20203221.
- ^ Fusco N, Guerini-Rocco E, Schultheis AM, Badve SS, Reis-Filho JS, Weigelt B (Feb 2015). "The birth of an adenoid cystic carcinoma" (PDF). Int J Surg Pathol. 23 (1): 26–7. doi:10.1177/1066896914548795. hdl:1805/7652. PMID 25185745. S2CID 5935648.
- ^ Fordice, Jim; Kershaw, Corey; El-Naggar, Adel; Goepfert, Helmuth (February 1999). "Adenoid Cystic Carcinoma of the Head and Neck: Predictors of Morbidity and Mortality". Archives of Otolaryngology–Head & Neck Surgery. 125 (2): 149–52. doi:10.1001/archotol.125.2.149. PMID 10037280.
- ^ a b Persson M, Andrén Y, Mark J, Horlings HM, Persson F, Stenman G (2009). "Recurrent fusion of MYB and NFIB transcription factor genes in carcinomas of the breast and head and neck". Proc Natl Acad Sci U S A. 106 (44): 18740–4. Bibcode:2009PNAS..10618740P. doi:10.1073/pnas.0909114106. PMC 2773970. PMID 19841262.
- ^ Andersson MK, Stenman G (2016). "The landscape of gene fusions and somatic mutations in salivary gland neoplasms - Implications for diagnosis and therapy". Oral Oncol. 57: 63–9. doi:10.1016/j.oraloncology.2016.04.002. PMID 27101980.
- ^ a b Persson M, Andrén Y, Moskaluk CA, Frierson HF Jr, Cooke SL, Futreal PA, Kling T, Nelander S, Nordkvist A, Persson F, Stenman G (2012). "Clinically significant copy number alterations and complex rearrangements of MYB and NFIB in head and neck adenoid cystic carcinoma". Genes Chromosomes Cancer. 51 (8): 805–17. doi:10.1002/gcc.21965. PMID 22505352. S2CID 25742114.
- ^ Brayer KJ, Frerich CA, Kang H, Ness SA (2016). "Recurrent Fusions in MYB and MYBL1 Define a Common, Transcription Factor-Driven Oncogenic Pathway in Salivary Gland Adenoid Cystic Carcinoma". Cancer Discov. 622 (2): 176–87. doi:10.1158/2159-8290.CD-15-0859. PMC 4744535. PMID 26631070.
- ^ Mitani Y, Liu B, Rao PH, Borra VJ, Zafereo M, Weber RS, Kies M, Lozano G, Futreal PA, Caulin C, El-Naggar AK (2016). "Novel MYBL1 Gene Rearrangements with Recurrent MYBL1-NFIB Fusions in Salivary Adenoid Cystic Carcinomas Lacking t(6;9) Translocations". Clin Cancer Res. 22 (3): 725–33. doi:10.1158/1078-0432.CCR-15-2867-T. PMC 4807116. PMID 26631609.
- ^ Andersson MK, Afshari MK, Andrén Y, Wick MJ, Stenman G (2017). "Targeting the Oncogenic Transcriptional Regulator MYB in Adenoid Cystic Carcinoma by Inhibition of IGF1R/AKT Signaling". J Natl Cancer Inst. 109 (9). doi:10.1093/jnci/djx017. PMID 28954282.
- ^ Ho AS, Kannan K, Roy DM, Morris LG, Ganly I, Katabi N, Ramaswami D, Walsh LA, Eng S, Huse JT, Zhang J, Dolgalev I, Huberman K, Heguy A, Viale A, Drobnjak M, Leversha MA, Rice CE, Singh B, Iyer NG, Leemans CR, Bloemena E, Ferris RL, Seethala RR, Gross BE, Liang Y, Sinha R, Peng L, Raphael BJ, Turcan S, Gong Y, Schultz N, Kim S, Chiosea S, Shah JP, Sander C, Lee W, Chan TA (2013). "The mutational landscape of adenoid cystic carcinoma". Nat Genet. 45 (7): 791–8. doi:10.1038/ng.2643. PMC 3708595. PMID 23685749.
- ^ Stephens PJ, Davies HR, Mitani Y, Van Loo P, Shlien A, Tarpey PS, Papaemmanuil E, Cheverton A, Bignell GR, Butler AP, Gamble J, Gamble S, Hardy C, Hinton J, Jia M, Jayakumar A, Jones D, Latimer C, McLaren S, McBride DJ, Menzies A, Mudie L, Maddison M, Raine K, Nik-Zainal S, O'Meara S, Teague JW, Varela I, Wedge DC, Whitmore I, Lippman SM, McDermott U, Stratton MR, Campbell PJ, El-Naggar AK, Futreal PA (2013). "Whole exome sequencing of adenoid cystic carcinoma". J Clin Invest. 123 (7): 2965–8. doi:10.1172/JCI67201. PMC 3999050. PMID 23778141.
- ^ Rettig EM, Talbot CC Jr, Sausen M, Jones S, Bishop JA, Wood LD, Tokheim C, Niknafs N, Karchin R, Fertig EJ, Wheelan SJ, Marchionni L, Considine M, Fakhry C, Papadopoulos N, Kinzler KW, Vogelstein B, Ha PK, Agrawal N (2013). "Whole-Genome Sequencing of Salivary Gland Adenoid Cystic Carcinoma". Cancer Prev Res (Phila). 9 (4): 265–74. doi:10.1158/1940-6207.CAPR-15-0316. PMC 4818686. PMID 26862087.
- ^ Laramore, GE (September 1987). "Fast neutron radiotherapy for inoperable salivary gland tumors: is it the treatment of choice?". International Journal of Radiation Oncology, Biology, Physics. 13 (9): 1421–3. doi:10.1016/0360-3016(87)90240-9. PMID 3114190.
- ^ Prott FJ, Haverkamp U, Willich N, Wagner W, Micke O, Pötter R (1996). "Ten years of fast neutron therapy in Münster". Bulletin du Cancer. Radiothérapie. 83 (Suppl): 115s–21s. doi:10.1016/0924-4212(96)84895-x. PMID 8949762.
- ^ Douglas, James G; Laramore, George E; Austin-Seymour, Mary; Koh, Wui-jin; Stelzer, Keith; Griffin, Thomas W (February 2000). "Treatment of locally advanced adenoid cystic carcinoma of the head and neck with neutron radiotherapy". International Journal of Radiation Oncology, Biology, Physics. 46 (3): 551–7. doi:10.1016/S0360-3016(99)00445-9. PMID 10701733.
- ^ Breteau N, Wachter T, Kerdraon R, et al. (2000). "Utilisation des neutrons rapides dans le traitement des tumeurs des glandes salivaires : rationnel, revue de la littérature et expérience d'Orléans" [Use of fast neutrons in the treatment of tumors of the salivary glands: rationale, review of the literature and experience in Orleans]. Cancer/Radiothérapie (in French). 4 (3): 181–90. doi:10.1016/S1278-3218(00)89092-7. PMID 10897760.
- ^ a b Lee SC (23 December 2021). "Salivary Gland Neoplasms". Medscape. Updated: Jan 13, 2021
Diagrams by Mikael Häggström, MD
Further reading
- Neville, Damm, Allen, Bouquot. Oral and Maxillofacial Pathology. 2nd edition.






![Relative incidence of submandibular tumors, with adenoid cystic carcinoma being the second most common.[17]](http://upload.wikimedia.org/wikipedia/commons/thumb/a/a7/Relative_incidence_of_submandibular_tumors.png/519px-Relative_incidence_of_submandibular_tumors.png)
![Relative incidence of parotid tumors, with adenoid cystic carcinoma being relatively rare.[17]](http://upload.wikimedia.org/wikipedia/commons/thumb/b/b1/Relative_incidence_of_parotid_tumors.png/517px-Relative_incidence_of_parotid_tumors.png)