Vigabatrin
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /vaɪˈɡæbətrɪn/ vy-GAB-ə-trin |
| Trade names | Sabril, others |
| Other names | γ-Vinyl-GABA |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a610016 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 80–90% |
| Protein binding | 0% |
| Metabolism | not metabolized |
| Elimination half-life | 5–8 hours in young adults, 12–13 hours in the elderly. |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.165.122 |
| Chemical and physical data | |
| Formula | C6H11NO2 |
| Molar mass | 129.159 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 171 to 177 °C (340 to 351 °F) |
| |
| |
| (verify) | |
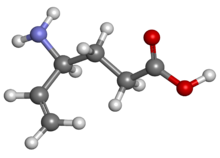
Vigabatrin, sold under the brand name Sabril among others, is a medication used in the management and treatment of infantile spasms and refractory complex partial seizures.
It works by inhibiting the breakdown of γ-aminobutyric acid (GABA). It is also known as γ-vinyl-GABA, and is a structural analogue of GABA, but does not bind to GABA receptors.[7]
Vigabatrin is generally used only in cases of treatment-resistant epilepsy due to the risk of permanent vision loss.[8] Although estimates of visual field loss vary substantially, risk appears to be lower among infants with treatment duration less than 12 months and the risk of clinically meaningful vision loss is very low among children treated for infantile spasms.[9][10]
Medical uses
[edit]Epilepsy
[edit]In Canada, vigabatrin is approved for use as an adjunctive treatment (with other drugs) in treatment resistant epilepsy, complex partial seizures, secondary generalized seizures, and for monotherapy use in infantile spasms in West syndrome.[7]
As of 2003, vigabatrin is approved in Mexico for the treatment of epilepsy that is not satisfactorily controlled by conventional therapy (adjunctive or monotherapy) or in recently diagnosed patients who have not tried other agents (monotherapy).[11]
Vigabatrin is also indicated for monotherapy use in secondarily generalized tonic-clonic seizures, partial seizures, and in infantile spasms due to West syndrome.[11]
Others
[edit]Vigabatrin reduced cholecystokinin tetrapeptide-induced symptoms of panic disorder, in addition to elevated cortisol and ACTH levels, in healthy volunteers.[12]
Vigabatrin is also used to treat seizures in succinic semialdehyde dehydrogenase deficiency (SSADHD), which is an inborn GABA metabolism defect that causes intellectual disability, hypotonia, seizures, speech disturbance, and ataxia through the accumulation of γ-Hydroxybutyric acid (GHB). Vigabatrin helps lower GHB levels through GABA transaminase inhibition. However, this is in the brain only; it has no effect on peripheral GABA transaminase, so the GHB keeps building up and eventually reaches the brain.[13]
Adverse effects
[edit]Central nervous system
[edit]Sleepiness (12.5%), headache (3.8%), dizziness (3.8%), nervousness (2.7%), depression (2.5%), memory disturbances (2.3%), diplopia (2.2%), aggression (2.0%), ataxia (1.9%), vertigo (1.9%), hyperactivity (1.8%), vision loss (1.6%) (See below), confusion (1.4%), insomnia (1.3%), impaired concentration (1.2%), personality issues (1.1%).[7] Out of 299 children, 33 (11%) became hyperactive.[7]
Some patients develop psychosis during the course of vigabatrin therapy,[14] which is more common in adults than in children.[15] This can happen even in patients with no prior history of psychosis.[16] Other rare CNS side effects include anxiety, emotional lability, irritability, tremor, abnormal gait, and speech disorder.[7]
Gastrointestinal
[edit]Abdominal pain (1.6%), constipation (1.4%), vomiting (1.4%), and nausea (1.4%). Dyspepsia and increased appetite occurred in less than 1% of subjects in clinical trials.[7]
Body as a whole
[edit]Fatigue (9.2%), weight gain (5.0%), asthenia (1.1%).[7]
Teratogenicity
[edit]A teratology study conducted in rabbits found that a dose of 150 mg/kg/day caused cleft palate in 2% of pups and a dose of 200 mg/kg/day caused it in 9%.[7] This may be due to a decrease in methionine levels, according to a study published in March 2001.[17] In 2005, a study conducted at the University of Catania was published stating that rats whose mothers had consumed 250–1000 mg/kg/day had poorer performance in the water maze and open-field tasks, rats in the 750 mg group were underweight at birth and did not catch up to the control group, and rats in the 1000 mg group did not survive pregnancy.[18]
There is no controlled teratology data in humans to date.
Sensory
[edit]In 2003, vigabatrin was shown by Frisén and Malmgren to cause irreversible diffuse atrophy of the retinal nerve fiber layer in a retrospective study of 25 patients.[19] This has the most effect on the outer area (as opposed to the macular, or central area) of the retina.[20] Visual field defects had been reported as early as 1997 by Tom Eke and others, in the UK. Some authors, including Comaish et al. believe that visual field loss and electrophysiological changes may be demonstrable in up to 50% of Vigabatrin users.
The retinal toxicity of vigabatrin can be attributed to a taurine depletion.[21]
Due to safety issues, the Vigabatrin REMS Program is required by the FDA to ensure informed decisions before initiating and to ensure appropriate use of this drug.[22]
Interactions
[edit]A study published in 2002 found that vigabatrin causes a statistically significant increase in plasma clearance of carbamazepine.[23]
In 1984, Drs Rimmer and Richens at the University of Wales reported that administering vigabatrin with phenytoin lowered the serum phenytoin concentration in patients with treatment-resistant epilepsy.[24] Five years later, the same two scientists reported a fall in concentration of phenytoin of 23% within five weeks in a paper describing their failed attempt at elucidating the mechanism behind this interaction.[25]
Pharmacology
[edit]Vigabatrin is an irreversible mechanism-based inhibitor of gamma-aminobutyric acid aminotransferase (GABA-AT), the enzyme responsible for the catabolism of GABA. Inhibition of GABA-AT results in increased levels of GABA in the brain.[7][26] Vigabatrin is a racemic compound, and its [S]-enantiomer is pharmacologically active.[27],[28]

Pharmacokinetics
[edit]With most drugs, elimination half-life is a useful predictor of dosing schedules and the time needed to reach steady state concentrations. In the case of vigabatrin, however, it has been found that the half-life of biologic activity is far longer than the elimination half-life.[30]
For vigabatrin, there is no range of target concentrations because researchers found no difference between the serum concentration levels of responders and those of non-responders.[31] Instead, the duration of action is believed to be more a function of the GABA-T resynthesis rate; levels of GABA-T do not usually return to their normal state until six days after stopping the medication.[28]
History
[edit]Vigabatrin was developed in the 1980s with the specific goal of increasing GABA concentrations in the brain in order to stop an epileptic seizure. To do this, the drug was designed to irreversibly inhibit the GABA transaminase, which degrades the GABA substrate. Although the drug was approved for treatment in the United Kingdom in 1989, the authorized use of Vigabatrin by US Food and Drug Administration was delayed twice in the United States before 2009. It was delayed in 1983 because animal trials produced intramyelinic edema, however, the effects were not apparent in human trials so the drug design continued. In 1997, the trials were temporarily suspended because it was linked to peripheral visual field defects in humans.[32]
Society and culture
[edit]Legal status
[edit]Vigabatrin (Sabril) was approved for medical use in the United States in August 2009.[33][34]
In April 2017, the US Food and Drug Administration (FDA) approved the first generic powder packets for the oral solution version of vigabatrin.[35] In January 2019, the FDA approved the first generic tablet version of vigabatrin.[36]
Vigpoder was approved in the United States in June 2022.[6]
Vigafyde was approved in the United States in June 2024.[4][37][38]
Brand Names
[edit]Vigabatrin is sold under the brand names Sabril, Vigafyde,[4] and Vigpoder.[6]
Vigabatrin is sold as Sabril in Canada,[39] Mexico,[11] and the United Kingdom.[40] The brand name in Denmark is Sabrilex.
Research
[edit]The PREVeNT Trial
[edit]The PREVeNT study found that early vigabatrin treatment delayed the onset and reduced the overall prevalence of infantile spasms in TSC infants. However, the seizure prevention was not seen for other seizure types, including focal seizures, that are highly prevalent in this population. PREVeNT, similarly to EPISTOP, reported a reduced incidence of infantile spasms up to 24 months of age.[36]
EPISTOP Trial
[edit]Infantile spasms are seen in 50 to 70% of children with TSC, and are associated with both drug-resistance and intellectual disability. Importantly, in EPISTOP, none of the children who received preventive treatment developed infantile spasms throughout the 2-year course of the study, in contrast to 10 of 25 (40%) receiving conventional treatment.[36]
References
[edit]- ^ Anvisa (March 31, 2023). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published April 4, 2023). Archived from the original on August 3, 2023. Retrieved August 16, 2023.
- ^ "Sabril- vigabatrin tablet, film coated". DailyMed. October 20, 2021. Retrieved September 5, 2024.
- ^ "Sabril- vigabatrin powder, for solution". DailyMed. October 20, 2021. Retrieved September 5, 2024.
- ^ a b c "Vigafyde- vigabatrin solution". DailyMed. August 23, 2024. Retrieved September 5, 2024.
- ^ "Vigadrone- vigabatrin tablet". DailyMed. July 14, 2023. Retrieved September 5, 2024.
- ^ a b c "Vigpoder- vigabatrin powder, for solution". DailyMed. March 20, 2024. Retrieved September 5, 2024.
- ^ a b c d e f g h i Long PW (2003). "Vigabatrin". Drug Monograph. Internet Mental Health. Archived from the original on April 23, 2006.
- ^ "Sabril (vigabatrin) Tablets for Oral Use, Powder for Oral Solution. Full Prescribing Information" (PDF). Lundbeck.
- ^ Hussain SA, Schmid E, Peters JM, Goyal M, Bebin EM, Northrup H, et al. (Tuberous Sclerosis Complex Autism Center of Excellence Network) (2018). "High vigabatrin dosage is associated with lower risk of infantile spasms relapse among children with tuberous sclerosis complex". Epilepsy Research. 148: 1–7. doi:10.1016/j.eplepsyres.2018.09.016. PMC 6347124. PMID 30296632.
- ^ Schwarz MD, Li M, Tsao J, Zhou R, Wu YW, Sankar R, et al. (2016). "A lack of clinically apparent vision loss among patients treated with vigabatrin with infantile spasms: The UCLA experience". Epilepsy & Behavior. 57 (Pt A): 29–33. doi:10.1016/j.yebeh.2016.01.012. PMID 26921595.
- ^ a b c "DEF Mexico: Sabril". Diccionario de Especialdades Farmaceuticas. (49 ed.). 2003. Archived from the original on September 14, 2005.
- ^ Zwanzger P, Baghai TC, Schuele C, Strohle A, Padberg F, Kathmann N, et al. (2001). "Vigabatrin decreases cholecystokinin-tetrapeptide (CCK-4) induced panic in healthy volunteers". Neuropsychopharmacology. 25 (5): 699–703. doi:10.1016/S0893-133X(01)00266-4. PMID 11682253.
- ^ Pearl PL, Wiwattanadittakul N, Roullet JB, Gibson KM (May 5, 2004). "Succinic Semialdehyde Dehydrogenase Deficiency". In dam MP, Mirzaa GM, Pagon RA, Wallace SE, Bean LJ, Gripp KW, Amemiya A (eds.). GeneReviews. University of Washington. PMID 20301374. Archived from the original on July 28, 2020. Retrieved September 6, 2010.
- ^ Sander JW, Hart YM (1990). "Vigabatrin and behaviour disturbance". Lancet. 335 (8680): 57. doi:10.1016/0140-6736(90)90190-G. PMID 1967367. S2CID 34456538.
- ^ Chiaretti A, Castorina M, Tortorolo L, Piastra M, Polidori G (1994). "[Acute psychosis and vigabatrin in childhood]". La Pediatria Medica e Chirurgica: Medical and Surgical Pediatrics (in Italian). 16 (5): 489–90. PMID 7885961.
- ^ Sander JW, Hart YM, Trimble MR, Shorvon SD (1991). "Vigabatrin and psychosis". Journal of Neurology, Neurosurgery, and Psychiatry. 54 (5): 435–9. doi:10.1136/jnnp.54.5.435. PMC 488544. PMID 1865207.
- ^ Abdulrazzaq YM, Padmanabhan R, Bastaki SM, Ibrahim A, Bener A (2001). "Placental transfer of vigabatrin (gamma-vinyl GABA) and its effect on concentration of amino acids in the embryo of TO mice". Teratology. 63 (3): 127–33. doi:10.1002/tera.1023. PMID 11283969.
- ^ Lombardo SA, Leanza G, Meli C, Lombardo ME, Mazzone L, Vincenti I, et al. (2005). "Maternal exposure to the antiepileptic drug vigabatrin affects postnatal development in the rat" (PDF). Neurological Sciences. 26 (2): 89–94. doi:10.1007/s10072-005-0441-6. hdl:2108/194069. PMID 15995825. S2CID 25257244. Archived (PDF) from the original on August 27, 2021. Retrieved September 3, 2019.
- ^ Frisén L, Malmgren K (2003). "Characterization of vigabatrin-associated optic atrophy". Acta Ophthalmologica Scandinavica. 81 (5): 466–73. doi:10.1034/j.1600-0420.2003.00125.x. PMID 14510793.
- ^ Buncic JR, Westall CA, Panton CM, Munn JR, MacKeen LD, Logan WJ (2004). "Characteristic retinal atrophy with secondary "inverse" optic atrophy identifies vigabatrin toxicity in children". Ophthalmology. 111 (10): 1935–42. doi:10.1016/j.ophtha.2004.03.036. PMC 3880364. PMID 15465561.
- ^ Gaucher D, Arnault E, Husson Z, Froger N, Dubus E, Gondouin P, et al. (November 2012). "Taurine deficiency damages retinal neurones: cone photoreceptors and retinal ganglion cells". Amino Acids. 43 (5): 1979–1993. doi:10.1007/s00726-012-1273-3. PMC 3472058. PMID 22476345.
- ^ "Sabril (vigabatrin) tablets, for oral use Sabril (vigabatrin) powder for oral..." Sabril.net. Retrieved May 31, 2019.[permanent dead link]
- ^ Sánchez-Alcaraz A, Quintana MB, López E, Rodríguez I, Llopis P (December 2002). "Effect of vigabatrin on the pharmacokinetics of carbamazepine". Journal of Clinical Pharmacy and Therapeutics. 27 (6): 427–430. doi:10.1046/j.1365-2710.2002.00441.x. PMID 12472982. S2CID 29986581.
- ^ Rimmer EM, Richens A (1984). "Double-blind study of gamma-vinyl GABA in patients with refractory epilepsy". Lancet. 1 (8370): 189–90. doi:10.1016/S0140-6736(84)92112-3. PMID 6141335. S2CID 54336689.
- ^ Rimmer EM, Richens A (1989). "Interaction between vigabatrin and phenytoin". British Journal of Clinical Pharmacology. 27 (Suppl 1): 27S–33S. doi:10.1111/j.1365-2125.1989.tb03458.x. PMC 1379676. PMID 2757906.
- ^ Rogawski MA, Löscher W (July 2004). "The neurobiology of antiepileptic drugs". Nature Reviews. Neuroscience. 5 (7): 553–564. doi:10.1038/nrn1430. PMID 15208697. S2CID 2201038. Archived from the original on December 16, 2020. Retrieved June 5, 2020.
- ^ Sheean G, Schramm T, Anderson DS, Eadie MJ (1992). "Vigabatrin--plasma enantiomer concentrations and clinical effects". Clinical and Experimental Neurology. 29: 107–116. PMID 1343855.
- ^ a b Gram L, Larsson OM, Johnsen A, Schousboe A (1989). "Experimental studies of the influence of vigabatrin on the GABA system". British Journal of Clinical Pharmacology. 27 (Suppl 1): 13S–17S. doi:10.1111/j.1365-2125.1989.tb03455.x. PMC 1379673. PMID 2757904.
- ^ Storici P, De Biase D, Bossa F, Bruno S, Mozzarelli A, Peneff C, et al. (January 2004). "Structures of gamma-aminobutyric acid (GABA) aminotransferase, a pyridoxal 5'-phosphate, and [2Fe-2S] cluster-containing enzyme, complexed with gamma-ethynyl-GABA and with the antiepilepsy drug vigabatrin" (PDF). The Journal of Biological Chemistry. 279 (1): 363–373. doi:10.1074/jbc.M305884200. PMID 14534310.
- ^ Browne TR (November 1998). "Pharmacokinetics of antiepileptic drugs". Neurology. 51 (5 Suppl 4): S2–S7. doi:10.1212/wnl.51.5_suppl_4.s2. PMID 9818917. S2CID 39231047.
- ^ Lindberger M, Luhr O, Johannessen SI, Larsson S, Tomson T (2003). "Serum concentrations and effects of gabapentin and vigabatrin: observations from a dose titration study". Therapeutic Drug Monitoring. 25 (4): 457–62. doi:10.1097/00007691-200308000-00007. PMID 12883229. S2CID 35834401.
- ^ Ben-Menachem E (2011). "Mechanism of action of vigabatrin: correcting misperceptions". Acta Neurologica Scandinavica. Supplementum. 124 (192): 5–15. doi:10.1111/j.1600-0404.2011.01596.x. PMID 22061176. S2CID 25347559.
- ^ "Drug Approval Package: Sabril (Vigabatrin) Tablets NDA #020427". U.S. Food and Drug Administration. November 23, 2009. Retrieved September 8, 2024.
- ^ Bresnahan R, Gianatsi M, Maguire MJ, Tudur Smith C, Marson AG (July 2020). "Vigabatrin add-on therapy for drug-resistant focal epilepsy". The Cochrane Database of Systematic Reviews. 2020 (7): CD007302. doi:10.1002/14651858.CD007302.pub3. PMC 8211760. PMID 32730657.
- ^ "Sabril (vigabatrin) – First-time generic" (PDF). OptumRx.
- ^ a b c Kotulska K, Kwiatkowski DJ, Curatolo P, Weschke B, Riney K, Jansen F, et al. (February 2021). "Prevention of Epilepsy in Infants with Tuberous Sclerosis Complex in the EPISTOP Trial". Annals of Neurology. 89 (2): 304–314. doi:10.1002/ana.25956. PMC 7898885. PMID 33180985.
- ^ PharmD BP (June 18, 2024). "Ready-to-Use Vigabatrin Oral Solution Approved for Infantile Spasms". MPR. Retrieved June 18, 2024.
- ^ "Pyros Pharmaceuticals Announces FDA Approval of Vigafyde (vigabatrin) as the First and Only Ready-to-Use Vigabatrin Oral Solution" (Press release). Pyros Pharmaceuticals. June 17, 2024. Retrieved June 18, 2024 – via Businesswire.
- ^ "Vigabatrin Drug Information". Drugs.com. Archived from the original on July 28, 2020. Retrieved January 23, 2018.
- ^ "Treatments for Epilepsy - Vigabatrin". Norfolk and Waveney Mental Health Partnership NHS Trust. Archived from the original on February 11, 2002. Retrieved March 26, 2017.

