Health system
A health system, health care system or healthcare system is an organization of people, institutions, and resources that delivers health care services to meet the health needs of target populations.
There is a wide variety of health systems around the world, with as many histories and organizational structures as there are nations. Implicitly, nations must design and develop health systems in accordance with their needs and resources, although common elements in virtually all health systems are primary healthcare and public health measures.[1]
In certain nations, the orchestration of health system planning is decentralized, with various stakeholders in the market assuming responsibilities. In contrast, in other regions, a collaborative endeavor exists among governmental entities, labor unions, philanthropic organizations, religious institutions, or other organized bodies, aimed at the meticulous provision of healthcare services tailored to the specific needs of their respective populations. Nevertheless, it is noteworthy that the process of healthcare planning is frequently characterized as an evolutionary progression rather than a revolutionary transformation.[2][3]
As with other social institutional structures, health systems are likely to reflect the history, culture and economics of the states in which they evolve. These peculiarities bedevil and complicate international comparisons and preclude any universal standard of performance.
Goals
[edit]According to the World Health Organization (WHO), the directing and coordinating authority for health within the United Nations system, healthcare systems' goals are good health for the citizens, responsiveness to the expectations of the population, and fair means of funding operations. Progress towards them depends on how systems carry out four vital functions: provision of health care services, resource generation, financing, and stewardship.[4] Other dimensions for the evaluation of health systems include quality, efficiency, acceptability, and equity.[2] They have also been described in the United States as "the five C's": Cost, Coverage, Consistency, Complexity, and Chronic Illness.[5] Also, continuity of health care is a major goal.[6]
Definitions
[edit]Often health system has been defined with a reductionist perspective. Some authors[7] have developed arguments to expand the concept of health systems, indicating additional dimensions that should be considered:
- Health systems should not be expressed in terms of their components only, but also of their interrelationships;
- Health systems should include not only the institutional or supply side of the health system but also the population;
- Health systems must be seen in terms of their goals, which include not only health improvement, but also equity, responsiveness to legitimate expectations, respect of dignity, and fair financing, among others;
- Health systems must also be defined in terms of their functions, including the direct provision of services, whether they are medical or public health services, but also "other enabling functions, such as stewardship, financing, and resource generation, including what is probably the most complex of all challenges, the health workforce."[7]
World Health Organization definition
[edit]The World Health Organization defines health systems as follows:
A health system consists of all organizations, people and actions whose primary intent is to promote, restore or maintain health. This includes efforts to influence determinants of health as well as more direct health-improving activities. A health system is, therefore, more than the pyramid of publicly owned facilities that deliver personal health services. It includes, for example, a mother caring for a sick child at home; private providers; behaviour change programmes; vector-control campaigns; health insurance organizations; occupational health and safety legislation. It includes inter-sectoral action by health staff, for example, encouraging the ministry of education to promote female education, a well-known determinant of better health.[8]
Financial resources
[edit]
There are generally five primary methods of funding health systems:[9]
- general taxation to the state, county or municipality
- national health insurance
- voluntary or private health insurance
- out-of-pocket payments
- donations to charities
| Universal | Non-universal | |||
|---|---|---|---|---|
| Single payer | Multi-payer | Multi-payer | No insurance | |
| Single provider | Beveridge Model, Semashko model | |||
| Multiple Providers | National Health Insurance | Bismarck model | Private health insurance | Out-of-pocket |
Most countries' systems feature a mix of all five models. One study[10] based on data from the OECD concluded that all types of health care finance "are compatible with" an efficient health system. The study also found no relationship between financing and cost control.[citation needed] Another study examining single payer and multi payer systems in OECD countries found that single payer systems have significantly less hospital beds per 100,000 people than in multi payer systems.[11]
The term health insurance is generally used to describe a form of insurance that pays for medical expenses. It is sometimes used more broadly to include insurance covering disability or long-term nursing or custodial care needs. It may be provided through a social insurance program, or from private insurance companies. It may be obtained on a group basis (e.g., by a firm to cover its employees) or purchased by individual consumers. In each case premiums or taxes protect the insured from high or unexpected health care expenses.[citation needed]
Through the calculation of the comprehensive cost of healthcare expenditures, it becomes feasible to construct a standard financial framework, which may involve mechanisms like monthly premiums or annual taxes. This ensures the availability of funds to cover the healthcare benefits delineated in the insurance agreement. Typically, the administration of these benefits is overseen by a government agency, a nonprofit health fund, or a commercial corporation.[12]
Many commercial health insurers control their costs by restricting the benefits provided, by such means as deductibles, copayments, co-insurance, policy exclusions, and total coverage limits. They will also severely restrict or refuse coverage of pre-existing conditions. Many government systems also have co-payment arrangements but express exclusions are rare or limited because of political pressure. The larger insurance systems may also negotiate fees with providers.[citation needed]
Many forms of social insurance systems control their costs by using the bargaining power of the community they are intended to serve to control costs in the health care delivery system. They may attempt to do so by, for example, negotiating drug prices directly with pharmaceutical companies, negotiating standard fees with the medical profession, or reducing unnecessary health care costs. Social systems sometimes feature contributions related to earnings as part of a system to deliver universal health care, which may or may not also involve the use of commercial and non-commercial insurers. Essentially the wealthier users pay proportionately more into the system to cover the needs of the poorer users who therefore contribute proportionately less. There are usually caps on the contributions of the wealthy and minimum payments that must be made by the insured (often in the form of a minimum contribution, similar to a deductible in commercial insurance models).[citation needed]
In addition to these traditional health care financing methods, some lower income countries and development partners are also implementing non-traditional or innovative financing mechanisms for scaling up delivery and sustainability of health care,[13] such as micro-contributions, public-private partnerships, and market-based financial transaction taxes. For example, as of June 2011, Unitaid had collected more than one billion dollars from 29 member countries, including several from Africa, through an air ticket solidarity levy to expand access to care and treatment for HIV/AIDS, tuberculosis and malaria in 94 countries.[14]
Payment models
[edit]In most countries, wage costs for healthcare practitioners are estimated to represent between 65% and 80% of renewable health system expenditures.[15][16] There are three ways to pay medical practitioners: fee for service, capitation, and salary. There has been growing interest in blending elements of these systems.[17]
Fee-for-service
[edit]Fee-for-service arrangements pay general practitioners (GPs) based on the service.[17] They are even more widely used for specialists working in ambulatory care.[17]
There are two ways to set fee levels:[17]
- By individual practitioners.
- Central negotiations (as in Japan, Germany, Canada and in France) or hybrid model (such as in Australia, France's sector 2, and New Zealand) where GPs can charge extra fees on top of standardized patient reimbursement rates.
Capitation
[edit]In capitation payment systems, GPs are paid for each patient on their "list", usually with adjustments for factors such as age and gender.[17] According to OECD (Organization for Economic Co-operation and Development), "these systems are used in Italy (with some fees), in all four countries of the United Kingdom (with some fees and allowances for specific services), Austria (with fees for specific services), Denmark (one third of income with remainder fee for service), Ireland (since 1989), the Netherlands (fee-for-service for privately insured patients and public employees) and Sweden (from 1994). Capitation payments have become more frequent in "managed care" environments in the United States."[17]
According to OECD, "capitation systems allow funders to control the overall level of primary health expenditures, and the allocation of funding among GPs is determined by patient registrations". However, under this approach, GPs may register too many patients and under-serve them, select the better risks and refer on patients who could have been treated by the GP directly. Freedom of consumer choice over doctors, coupled with the principle of "money following the patient" may moderate some of these risks. Aside from selection, these problems are likely to be less marked than under salary-type arrangements.'[citation needed]
Salary arrangements
[edit]In several OECD countries, general practitioners (GPs) are employed on salaries for the government.[17] According to OECD, "Salary arrangements allow funders to control primary care costs directly; however, they may lead to under-provision of services (to ease workloads), excessive referrals to secondary providers and lack of attention to the preferences of patients."[17] There has been movement away from this system.[17]
Value-based care
[edit]In recent years, providers have been switching from fee-for-service payment models to a value-based care payment system, where they are compensated for providing value to patients. In this system, providers are given incentives to close gaps in care and provide better quality care for patients. [18]
Spending
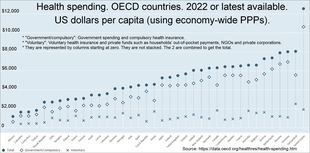
[edit]Expand the OECD charts below to see the breakdown:
- "Government/compulsory": Government spending and compulsory health insurance.
- "Voluntary": Voluntary health insurance and private funds such as households' out-of-pocket payments, NGOs and private corporations.
- They are represented by columns starting at zero. They are not stacked. The 2 are combined to get the total.
- At the source you can run your cursor over the columns to get the year and the total for that country.[19]
- Click the table tab at the source to get 3 lists (one after another) of amounts by country: "Total", "Government/compulsory", and "Voluntary".[19]

Information resources
[edit]Sound information plays an increasingly critical role in the delivery of modern health care and efficiency of health systems. Health informatics – the intersection of information science, medicine and healthcare – deals with the resources, devices, and methods required to optimize the acquisition and use of information in health and biomedicine. Necessary tools for proper health information coding and management include clinical guidelines, formal medical terminologies, and computers and other information and communication technologies. The kinds of health data processed may include patients' medical records, hospital administration and clinical functions, and human resources information.[20]
The use of health information lies at the root of evidence-based policy and evidence-based management in health care. Increasingly, information and communication technologies are being utilised to improve health systems in developing countries through: the standardisation of health information; computer-aided diagnosis and treatment monitoring; informing population groups on health and treatment.[21]
Management
[edit]The management of any health system is typically directed through a set of policies and plans adopted by government, private sector business and other groups in areas such as personal healthcare delivery and financing, pharmaceuticals, health human resources, and public health.[citation needed]
Public health is concerned with threats to the overall health of a community based on population health analysis. The population in question can be as small as a handful of people, or as large as all the inhabitants of several continents (for instance, in the case of a pandemic). Public health is typically divided into epidemiology, biostatistics and health services. Environmental, social, behavioral, and occupational health are also important subfields.[citation needed]

Today, most governments recognize the importance of public health programs in reducing the incidence of disease, disability, the effects of ageing and health inequities, although public health generally receives significantly less government funding compared with medicine. For example, most countries have a vaccination policy, supporting public health programs in providing vaccinations to promote health. Vaccinations are voluntary in some countries and mandatory in some countries. Some governments pay all or part of the costs for vaccines in a national vaccination schedule.[citation needed]
The rapid emergence of many chronic diseases, which require costly long-term care and treatment, is making many health managers and policy makers re-examine their healthcare delivery practices. An important health issue facing the world currently is HIV/AIDS.[22] Another major public health concern is diabetes.[23] In 2006, according to the World Health Organization, at least 171 million people worldwide had diabetes. Its incidence is increasing rapidly, and it is estimated that by 2030, this number will double. A controversial aspect of public health is the control of tobacco smoking, linked to cancer and other chronic illnesses.[24]
Antibiotic resistance is another major concern, leading to the reemergence of diseases such as tuberculosis. The World Health Organization, for its World Health Day 2011 campaign, called for intensified global commitment to safeguard antibiotics and other antimicrobial medicines for future generations.[citation needed]
Health systems performance
[edit]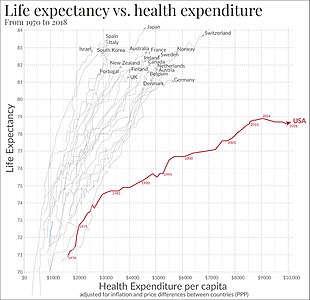
Since 2000, more and more initiatives have been taken at the international and national levels in order to strengthen national health systems as the core components of the global health system. Having this scope in mind, it is essential to have a clear, and unrestricted, vision of national health systems that might generate further progress in global health. The elaboration and the selection of performance indicators are indeed both highly dependent on the conceptual framework adopted for the evaluation of the health systems performance.[26] Like most social systems, health systems are complex adaptive systems where change does not necessarily follow rigid management models.[27] In complex systems path dependency, emergent properties and other non-linear patterns are seen,[28] which can lead to the development of inappropriate guidelines for developing responsive health systems.[29]
Quality frameworks are essential tools for understanding and improving health systems. They help define, prioritize, and implement health system goals and functions. Among the key frameworks is the World Health Organization's building blocks model, which enhances health quality by focusing on elements like financing, workforce, information, medical products, governance, and service delivery. This model influences global health evaluation and contributes to indicator development and research.[30]
The Lancet Global Health Commission's 2018 framework builds upon earlier models by emphasizing system foundations, processes, and outcomes, guided by principles of efficiency, resilience, equity, and people-centeredness. This comprehensive approach addresses challenges associated with chronic and complex conditions and is particularly influential in health services research in developing countries.[31] Importantly, recent developments also highlight the need to integrate environmental sustainability into these frameworks, suggesting its inclusion as a guiding principle to enhance the environmental responsiveness of health systems.[32]
An increasing number of tools and guidelines are being published by international agencies and development partners to assist health system decision-makers to monitor and assess health systems strengthening[33] including human resources development[34] using standard definitions, indicators and measures. In response to a series of papers published in 2012 by members of the World Health Organization's Task Force on Developing Health Systems Guidance, researchers from the Future Health Systems consortium argue that there is insufficient focus on the 'policy implementation gap'. Recognizing the diversity of stakeholders and complexity of health systems is crucial to ensure that evidence-based guidelines are tested with requisite humility and without a rigid adherence to models dominated by a limited number of disciplines.[29][35] Healthcare services often implement Quality Improvement Initiatives to overcome this policy implementation gap. Although many of these initiatives deliver improved healthcare, a large proportion fail to be sustained. Numerous tools and frameworks have been created to respond to this challenge and increase improvement longevity. One tool highlighted the need for these tools to respond to user preferences and settings to optimize impact.[36]
Health Policy and Systems Research (HPSR) is an emerging multidisciplinary field that challenges 'disciplinary capture' by dominant health research traditions, arguing that these traditions generate premature and inappropriately narrow definitions that impede rather than enhance health systems strengthening.[37] HPSR focuses on low- and middle-income countries and draws on the relativist social science paradigm which recognises that all phenomena are constructed through human behaviour and interpretation. In using this approach, HPSR offers insight into health systems by generating a complex understanding of context in order to enhance health policy learning.[38] HPSR calls for greater involvement of local actors, including policy makers, civil society and researchers, in decisions that are made around funding health policy research and health systems strengthening.[39]


International comparisons
[edit]
Health systems can vary substantially from country to country, and in the last few years, comparisons have been made on an international basis. The World Health Organization, in its World Health Report 2000, provided a ranking of health systems around the world according to criteria of the overall level and distribution of health in the populations, and the responsiveness and fair financing of health care services.[4] The goals for health systems, according to the WHO's World Health Report 2000 – Health systems: improving performance (WHO, 2000),[42] are good health, responsiveness to the expectations of the population, and fair financial contribution. There have been several debates around the results of this WHO exercise,[43] and especially based on the country ranking linked to it,[44] insofar as it appeared to depend mostly on the choice of the retained indicators.
Direct comparisons of health statistics across nations are complex. The Commonwealth Fund, in its annual survey, "Mirror, Mirror on the Wall", compares the performance of the health systems in Australia, New Zealand, the United Kingdom, Germany, Canada and the United States. Its 2007 study found that, although the United States system is the most expensive, it consistently underperforms compared to the other countries.[45] A major difference between the United States and the other countries in the study is that the United States is the only country without universal health care. The OECD also collects comparative statistics, and has published brief country profiles.[46][47][48] Health Consumer Powerhouse makes comparisons between both national health care systems in the Euro health consumer index and specific areas of health care such as diabetes[49] or hepatitis.[50]
Ipsos MORI produces an annual study of public perceptions of healthcare services across 30 countries.[51]
| Country | Life expectancy[52] | Infant mortality rate[53] | Preventable deaths per 100,000 people in 2007[54] | Physicians per 1000 people | Nurses per 1000 people | Per capita expenditure on health (USD PPP) | Healthcare costs as a percent of GDP | % of government revenue spent on health | % of health costs paid by government |
|---|---|---|---|---|---|---|---|---|---|
| Australia | 83.0 | 4.49 | 57 | 2.8 | 10.1 | 3,353 | 8.5 | 17.7 | 67.5 |
| Canada | 82.0 | 4.78 | 77[55] | 2.2 | 9.0 | 3,844 | 10.0 | 16.7 | 70.2 |
| Finland | 79.5 | 2.6 | 2.7 | 15.5 | 3,008 | 8.4 | |||
| France | 82.0 | 3.34 | 55 | 3.3 | 7.7 | 3,679 | 11.6 | 14.2 | 78.3 |
| Germany | 81.0 | 3.48 | 76 | 3.5 | 10.5 | 3,724 | 10.4 | 17.6 | 76.4 |
| Italy | 83.0 | 3.33 | 60 | 4.2 | 6.1 | 2,771 | 8.7 | 14.1 | 76.6 |
| Japan | 84.0 | 2.17 | 61 | 2.1 | 9.4 | 2,750 | 8.2 | 16.8 | 80.4 |
| Norway | 83.0 | 3.47 | 64 | 3.8 | 16.2 | 4,885 | 8.9 | 17.9 | 84.1 |
| Spain | 83.0 | 3.30 | 74 | 3.8 | 5.3 | 3,248 | 8.9 | 15.1 | 73.6 |
| Sweden | 82.0 | 2.73 | 61 | 3.6 | 10.8 | 3,432 | 8.9 | 13.6 | 81.4 |
| UK | 81.6 | 4.5 | 83 | 2.5 | 9.5 | 3,051 | 8.4 | 15.8 | 81.3 |
| US | 78.74 | 5.9 | 96 | 2.4 | 10.6 | 7,437 | 16.0 | 18.5 | 45.1 |
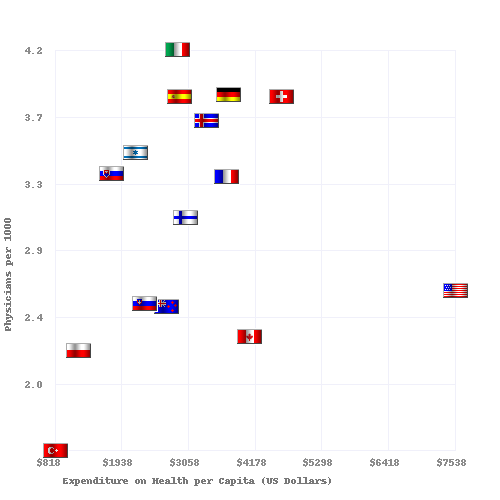
Physicians and hospital beds per 1000 inhabitants vs Health Care Spending in 2008 for OECD Countries. The data source is OECD.org - OECD.[47][48]
See also
[edit]- Acronyms in healthcare
- Catholic Church and health care
- Clinical Health Promotion
- Community health
- Comparison of the health care systems in Canada and the United States
- Consumer-driven health care
- Cultural competence in health care
- Global health
- Genetic testing
- List of countries by health insurance coverage
- Health administration
- Health care
- Health care provider
- Health care reform
- Health crisis
- Health economics
- Health equity
- Health human resources
- Health insurance
- Health policy
- Health promotion
- Health services research
- Healthy city
- Hospital network
- Medicine
- National health insurance
- Occupational safety and health
- Philosophy of healthcare
- Primary care
- Primary health care
- Public health
- Publicly funded health care
- Single-payer health care
- Social determinants of health
- Socialized medicine
- Timeline of global health
- Two-tier health care
- Universal health care
References
[edit]- ^ White F (2015). "Primary health care and public health: foundations of universal health systems". Med Princ Pract. 24 (2): 103–116. doi:10.1159/000370197. PMC 5588212. PMID 25591411.
- ^ a b "Health care system". Liverpool-ha.org.uk. Archived from the original on 25 January 2021. Retrieved 6 August 2011.
- ^ New Yorker magazine article: "Getting there from here." Archived 28 May 2014 at the Wayback Machine 26 January 2009
- ^ a b World Health Organization. (2000). World Health Report 2000 – Health systems: improving performance. Geneva, WHO [1]
- ^ Remarks by Johns Hopkins University President William Brody: "Health Care '08: What's Promised/What's Possible?" Archived 11 February 2009 at the Wayback Machine 7 September 2007
- ^ Cook, R. I.; Render, M.; Woods, D. (2000). "Gaps in the continuity of care and progress on patient safety". BMJ. 320 (7237): 791–794. doi:10.1136/bmj.320.7237.791. PMC 1117777. PMID 10720370.
- ^ a b Frenk J (2010). "The global health system: strengthening national health systems as the next step for global progress". PLOS Med. 7 (1): e1000089. doi:10.1371/journal.pmed.1000089. PMC 2797599. PMID 20069038.
- ^ "Everybody's business. Strengthening health systems to improve health outcomes : WHO's framework for action" (PDF). WHO. 2007. Archived (PDF) from the original on 28 December 2021. Retrieved 4 October 2020.
- ^ "Regional Overview of Social Health Insurance in South-East Asia Archived 24 February 2007 at the Wayback Machine, World Health Organization. And [2] Archived 3 September 2012 at the Wayback Machine. Retrieved 18 August 2006.
- ^ Glied, Sherry A. "Health Care Financing, Efficiency, and Equity." Archived 24 February 2012 at the Wayback Machine National Bureau of Economic Research, March 2008. Accessed 20 March 2008.
- ^ Bengali, Shawn M (13 April 2021). "A COMPARISON OF HOSPITAL CAPACITIES BETWEEN SINGLE-PAYER AND MULTIPAYER HEALTHCARE SYSTEMS AMONG OECD NATIONS" (PDF). Washington, D.C. Retrieved 5 July 2024.
- ^ How Private Insurance Works: A Primer Archived 21 December 2008 at the Wayback Machine by Gary Claxton, Institution for Health Care Research and Policy, Georgetown University, on behalf of the Henry J. Kaiser Family Foundation
- ^ Bloom, G; et al. (2008). "Markets, Information Asymmetry And Health Care: Towards New Social Contracts". Social Science and Medicine. 66 (10): 2076–2087. doi:10.1016/j.socscimed.2008.01.034. PMID 18316147. Archived from the original on 27 April 2021. Retrieved 26 May 2012.
- ^ UNITAID. Republic of Guinea Introduces Air Solidarity Levy to Fight AIDS, TB and Malaria. Archived 12 November 2011 at the Wayback Machine Geneva, 30 June 2011. Accessed 5 July 2011.
- ^ Saltman RB, Von Otter C. Implementing Planned Markets in Health Care: Balancing Social and Economic Responsibility. Buckingham: Open University Press 1995.
- ^ Kolehamainen-Aiken RL (1997). "Decentralization and human resources: implications and impact". Human Resources for Health Development. 2 (1): 1–14.
- ^ a b c d e f g h i Elizabeth Docteur; Howard Oxley (2003). "Health-Care Systems: Lessons from the Reform Experience" (PDF). OECD. Archived (PDF) from the original on 22 December 2015. Retrieved 22 January 2009.
- ^ "What is Value-Based Care and How to Make the Transition - Measures Manager". Archived from the original on 13 May 2019. Retrieved 13 May 2019.
- ^ a b c d OECD Data. Health resources - Health spending Archived 12 April 2020 at the Wayback Machine. doi:10.1787/8643de7e-en. 2 bar charts: For both: From bottom menus: Countries menu > choose OECD. Check box for "latest data available". Perspectives menu > Check box to "compare variables". Then check the boxes for government/compulsory, voluntary, and total. Click top tab for chart (bar chart). For GDP chart choose "% of GDP" from bottom menu. For per capita chart choose "US dollars/per capita". Click fullscreen button above chart. Click "print screen" key. Click top tab for table, to see data.
- ^ "Records Management Code of Practice". NHS England. 2023. Retrieved 29 June 2023.
- ^ Lucas, H (2008). "Information And Communications Technology For Future Health Systems In Developing Countries". Social Science and Medicine. 66 (10): 2122–2132. doi:10.1016/j.socscimed.2008.01.033. PMID 18343005. Archived from the original on 27 April 2021. Retrieved 26 May 2012.
- ^ "European Union Public Health Information System – HIV/Aides page". Euphix.org. Archived from the original on 26 July 2011. Retrieved 6 August 2011.
- ^ "European Union Public Health Information System – Diabetes page". Euphix.org. Archived from the original on 26 July 2011. Retrieved 6 August 2011.
- ^ "European Union Public Health Information System – Smoking Behaviors page". Euphix.org. Archived from the original on 1 August 2011. Retrieved 6 August 2011.
- ^ Link between health spending and life expectancy: US is an outlier Archived 11 March 2022 at the Wayback Machine. May 26, 2017. By Max Roser at Our World in Data. Click the sources tab under the chart for info on the countries, healthcare expenditures, and data sources. See the later version of the chart here Archived 5 March 2022 at the Wayback Machine.
- ^ Handler A, Issel M, Turnock B. A conceptual framework to measure performance of the public health system. American Journal of Public Health, 2001, 91(8): 1235–39.
- ^ Wilson, Tim; Plsek, Paul E. (29 September 2001). "Complexity, leadership, and management in healthcare organisations". BMJ. 323 (7315): 746–749. doi:10.1136/bmj.323.7315.746. ISSN 0959-8138. PMC 1121291. PMID 11576986.
- ^ Paina, Ligia; David Peters (5 August 2011). "Understanding pathways for scaling up health services through the lens of complex adaptive systems". Health Policy and Planning. 26 (5): 365–373. doi:10.1093/heapol/czr054. PMID 21821667. Archived from the original on 30 May 2013. Retrieved 18 May 2012.
- ^ a b Peters, David; Sara Bennet (2012). "Better Guidance Is Welcome, but without Blinders". PLOS Med. 9 (3): e1001188. doi:10.1371/journal.pmed.1001188. PMC 3308928. PMID 22448148. Archived from the original on 30 May 2013. Retrieved 18 May 2012.
- ^ Organization, World Health (2010). Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. World Health Organization. ISBN 978-92-4-156405-2. Archived from the original on 3 May 2024. Retrieved 15 May 2024.
- ^ Kruk, Margaret E.; Gage, Anna D.; Arsenault, Catherine; Jordan, Keely; Leslie, Hannah H.; Roder-DeWan, Sanam; Adeyi, Olusoji; Barker, Pierre; Daelmans, Bernadette; Doubova, Svetlana V.; English, Mike; García-Elorrio, Ezequiel; Guanais, Frederico; Gureje, Oye; Hirschhorn, Lisa R. (2018). "High-quality health systems in the Sustainable Development Goals era: time for a revolution". The Lancet. Global Health. 6 (11): e1196–e1252. doi:10.1016/S2214-109X(18)30386-3. ISSN 2214-109X. PMC 7734391. PMID 30196093. Archived from the original on 3 May 2024. Retrieved 15 May 2024.
- ^ Padget, Michael; Peters, Michael A.; Brunn, Matthias; Kringos, Dionne; Kruk, Margaret E. (30 April 2024). "Health systems and environmental sustainability: updating frameworks for a new era". BMJ. 385: e076957. doi:10.1136/bmj-2023-076957. ISSN 1756-1833. PMID 38688557. Archived from the original on 3 May 2024. Retrieved 15 May 2024.
- ^ World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva, WHO Press, 2010.
- ^ Dal Poz MR et al. Handbook on monitoring and evaluation of human resources for health. Geneva, WHO Press, 2009
- ^ Hyder, A; et al. (2007). "Exploring health systems research and its influence on policy processes in low income countries". BMC Public Health. 7: 309. doi:10.1186/1471-2458-7-309. PMC 2213669. PMID 17974000. Archived from the original on 30 May 2013. Retrieved 26 May 2012.
- ^ Lennox, Laura; Doyle, Cathal; Reed, Julie E.; Bell, Derek (1 September 2017). "What makes a sustainability tool valuable, practical and useful in real-world healthcare practice? A mixed-methods study on the development of the Long Term Success Tool in Northwest London". BMJ Open. 7 (9): e014417. doi:10.1136/bmjopen-2016-014417. ISSN 2044-6055. PMC 5623390. PMID 28947436.
- ^ Sheikh, Kabir; Lucy Gilson; Irene Akua Agyepong; Kara Hanson; Freddie Ssengooba; Sara Bennett (2011). "Building the Field of Health Policy and Systems Research: Framing the Questions". PLOS Medicine. 8 (8): e1001073. doi:10.1371/journal.pmed.1001073. PMC 3156683. PMID 21857809.

- ^ Gilson, Lucy; Kara Hanson; Kabir Sheikh; Irene Akua Agyepong; Freddie Ssengooba; Sara Bennet (2011). "Building the Field of Health Policy and Systems Research: Social Science Matters". PLOS Medicine. 8 (8): e1001079. doi:10.1371/journal.pmed.1001079. PMC 3160340. PMID 21886488.

- ^ Bennet, Sara; Irene Akua Agyepong; Kabir Sheikh; Kara Hanson; Freddie Ssengooba; Lucy Gilson (2011). "Building the Field of Health Policy and Systems Research: An Agenda for Action". PLOS Medicine. 8 (8): e1001081. doi:10.1371/journal.pmed.1001081. PMC 3168867. PMID 21918641.

- ^ "OECD.StatExtracts, Health, Non-Medical Determinants of Health, Body weight, Overweight or obese population, self-reported and measured, Total population" (Online Statistics). stats.oecd.org. OECD's iLibrary. 2013. Archived from the original on 2 April 2019. Retrieved 24 April 2014.
- ^ "OECD.StatExtracts, Health, Non-Medical Determinants of Health, Body weight, Obese population, self-reported and measured, Total population" (Online Statistics). stats.oecd.org. OECD's iLibrary. 2013. Archived from the original on 2 April 2019. Retrieved 24 April 2014.
- ^ World Health Organization. (2000) World Health Report 2000 – Health systems: improving performance. Geneva, WHO Press.
- ^ World Health Organization. Health Systems Performance: Overall Framework. Archived 17 June 2012 at the Wayback Machine Accessed 15 March 2011.
- ^ Navarro V (2000). "Assessment of the World Health Report 2000". Lancet. 356 (9241): 1598–601. doi:10.1016/s0140-6736(00)03139-1. PMID 11075789. S2CID 18001992.
- ^ "Mirror, Mirror on the Wall: An International Update on the Comparative Performance of American Health Care". The Commonwealth Fund. 15 May 2007. Archived from the original on 29 March 2009. Retrieved 7 March 2009.
- ^ Organisation for Economic Co-operation and Development. "OECD Health Data 2008: How Does Canada Compare" (PDF). Archived from the original (PDF) on 31 May 2013. Retrieved 9 January 2009.
- ^ a b "Updated statistics from a 2009 report". Oecd.org. Archived from the original on 5 March 2010. Retrieved 6 August 2011.
- ^ a b "OECD Health Data 2009 – Frequently Requested Data". Oecd.org. Archived from the original on 24 September 2015. Retrieved 6 August 2011.
- ^ "The Euro Consumer Diabetes Index 2008". Health Consumer Powerhouse. Archived from the original on 22 April 2016. Retrieved 29 April 2013.
- ^ "Euro Hepatitis Care Index 2012". Health Consumer Powerhouse. Archived from the original on 12 April 2016. Retrieved 29 April 2013.
- ^ "Mental health replaces Covid as the top health concern among Americans". ITIJ. 5 October 2022. Archived from the original on 14 October 2022. Retrieved 14 October 2022.
- ^ "Life expectancy at birth, total (years) | Data". data.worldbank.org. Archived from the original on 2 February 2021. Retrieved 3 August 2018.
- ^ CIA – The World Factbook: Infant Mortality Rate. Archived from the original on 18 December 2012 (Older data). Retrieved 15 May 2013.
- ^ "Mortality amenable to health care" Nolte, Ellen (2011). "Variations in Amenable Mortality—Trends in 16 High-Income Nations". Health Policy (Amsterdam, Netherlands). 103 (1). Commonwealth Fund: 47–52. doi:10.1016/j.healthpol.2011.08.002. PMID 21917350. Archived from the original on 5 February 2012. Retrieved 10 February 2012.
- ^ data for 2003
Nolte, Ellen (2008). "Measuring the Health of Nations: Updating an Earlier Analysis". Health Affairs. 27 (1). Commonwealth Fund: 58–71. doi:10.1377/hlthaff.27.1.58. PMID 18180480. Archived from the original on 11 January 2012. Retrieved 8 January 2012.
External links
[edit]- World Health Organization: Health Systems
- HRC/Eldis Health Systems Resource Guide Archived 2 August 2005 at the Wayback Machine research and other resources on health systems in developing countries
- OECD: Health policies, a list of latest publications by OECD