Key Points
-
Women generally have lower age-adjusted incidence and prevalence of atrial fibrillation (AF) than men; however, given the greater longevity of women, the absolute number of men and women with AF is similar
-
The prevalence of major risk factors differ by sex; women have higher prevalence of hypertension and valvular heart disease, and lower prevalence of coronary heart disease, than men
-
Women are more likely to present with atypical symptoms, such as weakness and fatigue, have longer duration of symptoms, and report worse quality of life and more-frequent depression than men
-
Female sex has been shown to be a risk factor for AF-related stroke or thromboembolism, myocardial infarction, and mortality, but has not been associated with incident heart failure or dementia
-
Future research is needed to address the knowledge gaps in sex-specific differences in AF
Abstract
Atrial fibrillation (AF) is the most common sustained arrhythmia in women and men worldwide. During the past century, a range of risk factors has been associated with AF, severe complications from the arrhythmia have been identified, and its prevalence has been increasing steadily. Whereas evidence has accumulated regarding sex-specific differences in coronary heart disease and stroke, the differences between women and men with AF has received less attention. We review the current literature on sex-specific differences in the epidemiology of AF, including incidence, prevalence, risk factors, and genetics, and in the pathophysiology and the clinical presentation and prognosis of patients with this arrhythmia. We highlight current knowledge gaps and areas that warrant future research, which might advance understanding of variation in the risk factors and complications of AF, and ultimately aid more-tailored management of the arrhythmia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Chugh, S. S. et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 129, 837–847 (2014).
Friberg, L. et al. Population screening of 75- and 76-year-old men and women for silent atrial fibrillation (STROKESTOP). Europace 15, 135–140 (2013).
Tedrow, U. B. et al. The long- and short-term impact of elevated body mass index on the risk of new atrial fibrillation the WHS (women's health study). J. Am. Coll. Cardiol. 55, 2319–2327 (2010).
Benjamin, E. J. et al. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 271, 840–844 (1994).
Schnabel, R. B. et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet 386, 154–162 (2015).
Christophersen, I. E. & Ellinor, P. T. Genetics of atrial fibrillation: from families to genomes. J. Hum. Genet. 61, 61–70 (2015).
Chen, Y. C. et al. Heterogeneous expression of potassium currents and pacemaker currents potentially regulates arrhythmogenesis of pulmonary vein cardiomyocytes. J. Cardiovasc. Electrophysiol. 20, 1039–1045 (2009).
Oyen, N. et al. Familial aggregation of lone atrial fibrillation in young persons. J. Am. Coll. Cardiol. 60, 917–921 (2012).
Zoller, B., Ohlsson, H., Sundquist, J. & Sundquist, K. High familial risk of atrial fibrillation/atrial flutter in multiplex families: a nationwide family study in Sweden. J. Am. Heart Assoc. 2, e003384 (2013).
Ball, J., Carrington, M. J., Wood, K. A., Stewart, S. & Investigators, S. Women versus men with chronic atrial fibrillation: insights from the Standard versus Atrial Fibrillation spEcific managemenT studY (SAFETY). PLoS ONE 8, e65795 (2013).
Scheuermeyer, F. X. et al. There are sex differences in the demographics and risk profiles of emergency department (ED) patients with atrial fibrillation and flutter, but no apparent differences in ED management or outcomes. Acad. Emerg. Med. 22, 1067–1075 (2015).
Xiong, Q., Proietti, M., Senoo, K. & Lip, G. Y. Asymptomatic versus symptomatic atrial fibrillation: a systematic review of age/gender differences and cardiovascular outcomes. Int. J. Cardiol. 191, 172–177 (2015).
Humphries, K. H. et al. New-onset atrial fibrillation: sex differences in presentation, treatment, and outcome. Circulation 103, 2365–2370 (2001).
Bushnell, C. et al. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45, 1545–1588 (2014).
Benjamin, E. J. et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 98, 946–952 (1998).
Miyasaka, Y. et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation 114, 119–125 (2006).
Chien, K. L. et al. Atrial fibrillation prevalence, incidence and risk of stroke and all-cause death among Chinese. Int. J. Cardiol. 139, 173–180 (2010).
Wilke, T. et al. Incidence and prevalence of atrial fibrillation: an analysis based on 8.3 million patients. Europace 15, 486–493 (2013).
Piccini, J. P. et al. Incidence and prevalence of atrial fibrillation and associated mortality among Medicare beneficiaries, 1993–2007. Circ. Cardiovasc. Qual. Outcomes 5, 85–93 (2012).
Svennberg, E. et al. Mass screening for untreated atrial fibrillation: the STROKESTOP Study. Circulation 131, 2176–2184 (2015).
Li, Y. et al. Prevalence of atrial fibrillation in China and its risk factors. Biomed. Environ. Sci. 26, 709–716 (2013).
Zhou, Z. & Hu, D. An epidemiological study on the prevalence of atrial fibrillation in the Chinese population of mainland China. J. Epidemiol. 18, 209–216 (2008).
Yap, K. B., Ng, T. P. & Ong, H. Y. Low prevalence of atrial fibrillation in community-dwelling Chinese aged 55 years or older in Singapore: a population-based study. J. Electrocardiol. 41, 94–98 (2008).
Jeong, J. H. Prevalence of and risk factors for atrial fibrillation in Korean adults older than 40 years. J. Korean Med. Sci. 20, 26–30 (2005).
Inoue, H. et al. Prevalence of atrial fibrillation in the general population of Japan: an analysis based on periodic health examination. Int. J. Cardiol. 137, 102–107 (2009).
Iguchi, Y. et al. Prevalence of atrial fibrillation in community-dwelling Japanese aged 40 years or older in Japan: analysis of 41,436 non-employee residents in Kurashiki-city. Circ. J. 72, 909–913 (2008).
Ohsawa, M. et al. Rapid increase in estimated number of persons with atrial fibrillation in Japan: an analysis from national surveys on cardiovascular diseases in 1980, 1990 and 2000. J. Epidemiol. 15, 194–196 (2005).
Stefansdottir, H., Aspelund, T., Gudnason, V. & Arnar, D. O. Trends in the incidence and prevalence of atrial fibrillation in Iceland and future projections. Europace 13, 1110–1117 (2011).
Majeed, A., Moser, K. & Carroll, K. Trends in the prevalence and management of atrial fibrillation in general practice in England and Wales, 1994–1998: analysis of data from the general practice research database. Heart 86, 284–288 (2001).
Lloyd-Jones, D. M. et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation 110, 1042–1046 (2004).
Heeringa, J. et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur. Heart J. 27, 949–953 (2006).
Guo, Y. et al. Prevalence, incidence, and lifetime risk of atrial fibrillation in China: new insights into the global burden of atrial fibrillation. Chest 147, 109–119 (2015).
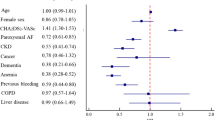
Alonso, A. et al. Simple risk model predicts incidence of atrial fibrillation in a racially and geographically diverse population: the CHARGE-AF consortium. J. Am. Heart Assoc. 2, e000102 (2013).
Wang, T. J. et al. Obesity and the risk of new-onset atrial fibrillation. JAMA 292, 2471–2477 (2004).
Potpara, T. S. et al. Gender-related differences in presentation, treatment and long-term outcome in patients with first-diagnosed atrial fibrillation and structurally normal heart: the Belgrade atrial fibrillation study. Int. J. Cardiol. 161, 39–44 (2012).
Dagres, N. et al. Gender-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: a report from the Euro Heart Survey on Atrial Fibrillation. J. Am. Coll. Cardiol. 49, 572–577 (2007).
Conen, D. et al. Influence of systolic and diastolic blood pressure on the risk of incident atrial fibrillation in women. Circulation 119, 2146–2152 (2009).
Huxley, R. R. et al. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: the Atherosclerosis Risk in Communities (ARIC) study. Circulation 123, 1501–1508 (2011).
Chiang, C. E. et al. Distribution and risk profile of paroxysmal, persistent, and permanent atrial fibrillation in routine clinical practice: insight from the real-life global survey evaluating patients with atrial fibrillation international registry. Circ. Arrhythm. Electrophysiol. 5, 632–639 (2012).
Murin, J. et al. Clinical characteristics, management, and control of permanent versus nonpermanent atrial fibrillation: insights from the RealiseAF survey. PLoS ONE 9, e86443 (2014).
Larsson, S. C., Drca, N. & Wolk, A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response meta-analysis. J. Am. Coll. Cardiol. 64, 281–289 (2014).
Ofman, P. et al. Regular physical activity and risk of atrial fibrillation: a systematic review and meta-analysis. Circ. Arrhythm. Electrophysiol. 6, 252–256 (2013).
Selmer, C. et al. The spectrum of thyroid disease and risk of new onset atrial fibrillation: a large population cohort study. BMJ 345, e7895 (2012).
Aviles, R. J. et al. Inflammation as a risk factor for atrial fibrillation. Circulation 108, 3006–3010 (2003).
Aizer, A. et al. Relation of vigorous exercise to risk of atrial fibrillation. Am. J. Cardiol. 103, 1572–1577 (2009).
Myrstad, M. et al. Effect of years of endurance exercise on risk of atrial fibrillation and atrial flutter. Am. J. Cardiol. 114, 1229–1233 (2014).
Mozaffarian, D., Furberg, C. D., Psaty, B. M. & Siscovick, D. Physical activity and incidence of atrial fibrillation in older adults: the cardiovascular health study. Circulation 118, 800–807 (2008).
Everett, B. M. et al. Physical activity and the risk of incident atrial fibrillation in women. Circ. Cardiovasc. Qual. Outcomes 4, 321–327 (2011).
Azarbal, F. et al. Obesity, physical activity, and their interaction in incident atrial fibrillation in postmenopausal women. J. Am. Heart Assoc. 3, e001127 (2014).
Drca, N., Wolk, A., Jensen-Urstad, M. & Larsson, S. C. Physical activity is associated with a reduced risk of atrial fibrillation in middle-aged and elderly women. Heart 101, 1627–1630 (2015).
Arnar, D. O. et al. Familial aggregation of atrial fibrillation in Iceland. Eur. Heart J. 27, 708–712 (2006).
Chen, L. Y., Herron, K. J., Tai, B. C. & Olson, T. M. Lone atrial fibrillation: influence of familial disease on gender predilection. J. Cardiovasc. Electrophysiol. 19, 802–806 (2008).
Christophersen, I. E. et al. Familial aggregation of atrial fibrillation: a study in Danish twins. Circ. Arrhythm. Electrophysiol. 2, 378–383 (2009).
Ellinor, P. T., Yoerger, D. M., Ruskin, J. N. & MacRae, C. A. Familial aggregation in lone atrial fibrillation. Hum. Genet. 118, 179–184 (2005).
Fox, C. S. et al. Parental atrial fibrillation as a risk factor for atrial fibrillation in offspring. JAMA 291, 2851–2855 (2004).
Yang, Y. Q. et al. Familial aggregation of lone atrial fibrillation in the Chinese population. Intern. Med. 49, 2385–2391 (2010).
Lubitz, S. A. et al. Association between familial atrial fibrillation and risk of new-onset atrial fibrillation. JAMA 304, 2263–2269 (2010).
Ravn, L. S. et al. Relation of 97T polymorphism in KCNE5 to risk of atrial fibrillation. Am. J. Cardiol. 96, 405–407 (2005).
Karst, M. L., Herron, K. J. & Olson, T. M. X-linked nonsyndromic sinus node dysfunction and atrial fibrillation caused by emerin mutation. J. Cardiovasc. Electrophysiol. 19, 510–515 (2008).
January, C. T. et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation 130, e199–e267 (2014).
Haissaguerre, M. et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N. Engl. J. Med. 339, 659–666 (1998).
Hocini, M. et al. Electrical conduction in canine pulmonary veins: electrophysiological and anatomic correlation. Circulation 105, 2442–2448 (2002).
Kamalvand, K. et al. Alterations in atrial electrophysiology associated with chronic atrial fibrillation in man. Eur. Heart J. 20, 888–895 (1999).
Raitt, M. H., Kusumoto, W., Giraud, G. & McAnulty, J. H. Reversal of electrical remodeling after cardioversion of persistent atrial fibrillation. J. Cardiovasc. Electrophysiol. 15, 507–512 (2004).
Franz, M. R., Karasik, P. L., Li, C., Moubarak, J. & Chavez, M. Electrical remodeling of the human atrium: similar effects in patients with chronic atrial fibrillation and atrial flutter. J. Am. Coll. Cardiol. 30, 1785–1792 (1997).
Wijffels, M. C., Kirchhof, C. J., Dorland, R. & Allessie, M. A. Atrial fibrillation begets atrial fibrillation. A study in awake chronically instrumented goats. Circulation 92, 1954–1968 (1995).
Ehrlich, J. R. et al. Cellular electrophysiology of canine pulmonary vein cardiomyocytes: action potential and ionic current properties. J. Physiol. 551, 801–813 (2003).
Platonov, P. G., Mitrofanova, L. B., Orshanskaya, V. & Ho, S. Y. Structural abnormalities in atrial walls are associated with presence and persistency of atrial fibrillation but not with age. J. Am. Coll. Cardiol. 58, 2225–2232 (2011).
Henry, W. L. et al. Relation between echocardiographically determined left atrial size and atrial fibrillation. Circulation 53, 273–279 (1976).
Vasan, R. S., Larson, M. G., Levy, D., Evans, J. C. & Benjamin, E. J. Distribution and categorization of echocardiographic measurements in relation to reference limits: the Framingham Heart Study: formulation of a height- and sex-specific classification and its prospective validation. Circulation 96, 1863–1873 (1997).
Vaziri, S. M., Larson, M. G., Benjamin, E. J. & Levy, D. Echocardiographic predictors of nonrheumatic atrial fibrillation. The Framingham Heart Study. Circulation 89, 724–730 (1994).
Nattel, S., Burstein, B. & Dobrev, D. Atrial remodeling and atrial fibrillation: mechanisms and implications. Circ. Arrhythm. Electrophysiol. 1, 62–73 (2008).
Anne, W. et al. Self-terminating AF depends on electrical remodeling while persistent AF depends on additional structural changes in a rapid atrially paced sheep model. J. Mol. Cell. Cardiol. 43, 148–158 (2007).
Filgueiras-Rama, D. et al. Long-term frequency gradients during persistent atrial fibrillation in sheep are associated with stable sources in the left atrium. Circ. Arrhythm. Electrophysiol. 5, 1160–1167 (2012).
Remes, J. et al. Persistent atrial fibrillation in a goat model of chronic left atrial overload. J. Thorac. Cardiovasc. Surg. 136, 1005–1011 (2008).
Ravens, U. Antiarrhythmic therapy in atrial fibrillation. Pharmacol. Ther. 128, 129–145 (2010).
Sanfilippo, A. J. et al. Atrial enlargement as a consequence of atrial fibrillation. A prospective echocardiographic study. Circulation 82, 792–797 (1990).
Kishi, S. et al. Race-ethnic and sex differences in left ventricular structure and function: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. J. Am. Heart Assoc. 4, e001264 (2015).
Tsang, T. S. et al. Left atrial volume: important risk marker of incident atrial fibrillation in 1655 older men and women. Mayo Clin. Proc. 76, 467–475 (2001).
Hudsmith, L. E., Petersen, S. E., Francis, J. M., Robson, M. D. & Neubauer, S. Normal human left and right ventricular and left atrial dimensions using steady state free precession magnetic resonance imaging. J. Cardiovasc. Magn. Reson. 7, 775–782 (2005).
McManus, D. D. et al. Longitudinal tracking of left atrial diameter over the adult life course: clinical correlates in the community. Circulation 121, 667–674 (2010).
Cochet, H. et al. Age, atrial fibrillation, and structural heart disease are the main determinants of left atrial fibrosis detected by delayed-enhanced magnetic resonance imaging in a general cardiology population. J. Cardiovasc. Electrophysiol. 26, 484–492 (2015).
Khera, A. et al. Race and gender differences in C-reactive protein levels. J. Am. Coll. Cardiol. 46, 464–469 (2005).
Mathew, J. S. et al. Fibroblast growth factor-23 and incident atrial fibrillation: the Multi-Ethnic Study of Atherosclerosis (MESA) and the Cardiovascular Health Study (CHS). Circulation 130, 298–307 (2014).
Patel, P., Dokainish, H., Tsai, P. & Lakkis, N. Update on the association of inflammation and atrial fibrillation. J. Cardiovasc. Electrophysiol. 21, 1064–1070 (2010).
Panwar, B. et al. Fibroblast growth factor 23 and risk of incident stroke in community-living adults. Stroke 46, 322–328 (2015).
Tsai, W. C., Chen, Y. C., Lin, Y. K., Chen, S. A. & Chen, Y. J. Sex differences in the electrophysiological characteristics of pulmonary veins and left atrium and their clinical implication in atrial fibrillation. Circ. Arrhythm. Electrophysiol. 4, 550–559 (2011).
Takigawa, M. et al. Differences in catheter ablation of paroxysmal atrial fibrillation between males and females. Int. J. Cardiol. 168, 1984–1991 (2013).
Yang, P. C., Kurokawa, J., Furukawa, T. & Clancy, C. E. Acute effects of sex steroid hormones on susceptibility to cardiac arrhythmias: a simulation study. PLoS Comput. Biol. 6, e1000658 (2010).
Nakamura, H. et al. Progesterone regulates cardiac repolarization through a nongenomic pathway: an in vitro patch-clamp and computational modeling study. Circulation 116, 2913–2922 (2007).
Nakagawa, M. et al. Influence of menstrual cycle on QT interval dynamics. Pacing Clin. Electrophysiol. 29, 607–613 (2006).
Rosano, G. M. et al. Cyclical variation in paroxysmal supraventricular tachycardia in women. Lancet 347, 786–788 (1996).
Rosano, G. M. et al. Acute electrophysiologic effect of estradiol 17β in menopausal women. Am. J. Cardiol. 86, 1385–1387 (2000).
Saba, S. et al. Effects of estrogen on cardiac electrophysiology in female mice. J. Cardiovasc. Electrophysiol. 13, 276–280 (2002).
Perez, M. V. et al. Effects of postmenopausal hormone therapy on incident atrial fibrillation: the Women's Health Initiative randomized controlled trials. Circ. Arrhythm. Electrophysiol. 5, 1108–1116 (2012).
Drici, M. D., Burklow, T. R., Haridasse, V., Glazer, R. I. & Woosley, R. L. Sex hormones prolong the QT interval and downregulate potassium channel expression in the rabbit heart. Circulation 94, 1471–1474 (1996).
Liu, X. K. et al. Gender difference in the cycle length-dependent QT and potassium currents in rabbits. J. Pharmacol. Exp. Ther. 285, 672–679 (1998).
Stramba-Badiale, M., Locati, E. H., Martinelli, A., Courville, J. & Schwartz, P. J. Gender and the relationship between ventricular repolarization and cardiac cycle length during 24-h Holter recordings. Eur. Heart J. 18, 1000–1006 (1997).
Nielsen, J. B. et al. Risk of atrial fibrillation as a function of the electrocardiographic PR interval: results from the Copenhagen ECG Study. Heart Rhythm 10, 1249–1256 (2013).
Cheng, S. et al. Long-term outcomes in individuals with prolonged PR interval or first-degree atrioventricular block. JAMA 301, 2571–2577 (2009).
Buitrago, C., Massheimer, V. & de Boland, A. R. Acute modulation of Ca2+ influx on rat heart by 17β-estradiol. Cell. Signal. 12, 47–52 (2000).
Jovanovic, S., Jovanovic, A., Shen, W. K. & Terzic, A. Low concentrations of 17β-estradiol protect single cardiac cells against metabolic stress-induced Ca2+ loading. J. Am. Coll. Cardiol. 36, 948–952 (2000).
Magnani, J. W. et al. Association of sex hormones, aging, and atrial fibrillation in men: the Framingham Heart Study. Circ. Arrhythm. Electrophysiol. 7, 307–312 (2014).
Tsuneda, T. et al. Deficiency of testosterone associates with the substrate of atrial fibrillation in the rat model. J. Cardiovasc. Electrophysiol. 20, 1055–1060 (2009).
Cove, C. L. et al. Female sex as an independent risk factor for stroke in atrial fibrillation: possible mechanisms. Thromb. Haemost. 111, 385–391 (2014).
Soliman, E. Z. et al. Atrial fibrillation and risk of ST-segment-elevation versus non-ST-segment-elevation myocardial infarction: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation 131, 1843–1850 (2015).
Udelson, J. E. Heart failure with preserved ejection fraction. Circulation 124, e540–e543 (2011).
Clayton, J. A. & Collins, F. S. Policy: NIH to balance sex in cell and animal studies. Nature 509, 282–283 (2014).
Lip, G. Y. et al. Prognosis and treatment of atrial fibrillation patients by European cardiologists: one year follow-up of the EURObservational Research Programme-Atrial Fibrillation General Registry Pilot Phase (EORP-AF Pilot registry). Eur. Heart J. 35, 3365–3376 (2014).
Paquette, M. et al. Role of gender and personality on quality-of-life impairment in intermittent atrial fibrillation. Am. J. Cardiol. 86, 764–768 (2000).
Sanna, T. et al. Cryptogenic stroke and underlying atrial fibrillation. N. Engl. J. Med. 370, 2478–2486 (2014).
Bekwelem, W. et al. Extracranial systemic embolic events in patients with nonvalvular atrial fibrillation: incidence, risk factors, and outcomes. Circulation 132, 796–803 (2015).
Frost, L. et al. Incident thromboembolism in the aorta and the renal, mesenteric, pelvic, and extremity arteries after discharge from the hospital with a diagnosis of atrial fibrillation. Arch. Intern. Med. 161, 272–276 (2001).
Andersen, L. V. et al. Atrial fibrillation and upper limb thromboembolectomy: a national cohort study. J. Thromb. Haemost. 9, 1738–1743 (2011).
Camm, A. J. et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation. Eur. Heart J. 33, 2719–2747 (2012).
Wang, T. J. et al. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA 290, 1049–1056 (2003).
Mikkelsen, A. P. et al. Female sex as a risk factor for stroke in atrial fibrillation: a nationwide cohort study. J. Thromb. Haemost. 10, 1745–1751 (2012).
Friberg, L., Benson, L., Rosenqvist, M. & Lip, G. Y. Assessment of female sex as a risk factor in atrial fibrillation in Sweden: nationwide retrospective cohort study. BMJ 344, e3522 (2012).
Fang, M. C. et al. Gender differences in the risk of ischemic stroke and peripheral embolism in atrial fibrillation: the AnTicoagulation and Risk factors In Atrial fibrillation (ATRIA) study. Circulation 112, 1687–1691 (2005).
Friberg, J., Scharling, H., Gadsboll, N., Truelsen, T. & Jensen, G. B. Comparison of the impact of atrial fibrillation on the risk of stroke and cardiovascular death in women versus men (The Copenhagen City Heart Study). Am. J. Cardiol. 94, 889–894 (2004).
Inoue, H. & Atarashi, H. Risk factors for thromboembolism in patients with paroxysmal atrial fibrillation. Am. J. Cardiol. 86, 852–855 (2000).
Avgil Tsadok, M. et al. Sex differences in stroke risk among older patients with recently diagnosed atrial fibrillation. JAMA 307, 1952–1958 (2012).
Aronow, W. S., Ahn, C., Kronzon, I. & Gutstein, H. Risk factors for new thromboembolic stroke in patients ≥62 years of age with chronic atrial fibrillation. Am. J. Cardiol. 82, 119–121 (1998).
Stollberger, C. et al. Transesophageal echocardiography to assess embolic risk in patients with atrial fibrillation. Ann. Intern. Med. 128, 630–638 (1998).
Van Staa, T. P., Setakis, E., Di Tanna, G. L., Lane, D. A. & Lip, G. Y. A comparison of risk stratification schemes for stroke in 79,884 atrial fibrillation patients in general practice. J. Thromb. Haemost. 9, 39–48 (2011).
Olesen, J. B., Fauchier, L., Lane, D. A., Taillandier, S. & Lip, G. Y. Risk factors for stroke and thromboembolism in relation to age among patients with atrial fibrillation: the Loire Valley Atrial Fibrillation Project. Chest 141, 147–153 (2012).
Poli, D., Antonucci, E., Testa, S., Ageno, W. & Palareti, G. Gender differences of bleeding and stroke risk in very old atrial fibrillation patients on VKA treatment: results of the EPICA study on the behalf of FCSA (Italian Federation of Anticoagulation Clinics). Thromb. Res. 131, 12–16 (2013).
Overvad, T. F. et al. Female sex as a risk factor for thromboembolism and death in patients with incident atrial fibrillation. Thromb. Haemost. 112, 789–795 (2014).
Cha, M.-J., Oh, G.-C., Hahn, S., Choi, E.-K. & Oh, S. Thromboembolic risk evaluation in patients with atrial fibrillation using a modified CHADS2 scoring system. J. Cardiovasc. Electrophysiol. 23, 155–162 (2012).
Nakagami, H. et al. Mitral regurgitation reduces the risk of stroke in patients with nonrheumatic atrial fibrillation. Am. Heart J. 136, 528–532 (1998).
Inoue, H. et al. Impact of gender on the prognosis of patients with nonvalvular atrial fibrillation. Am. J. Cardiol. 113, 957–962 (2014).
Siu, C.-W., Lip, G. Y. H., Lam, K.-F. & Tse, H.-F. Risk of stroke and intracranial hemorrhage in 9727 Chinese with atrial fibrillation in Hong Kong. Heart Rhythm 11, 1401–1408 (2014).
Friberg, L., Skeppholm, M. & Terént, A. Benefit of anticoagulation unlikely in patients with atrial fibrillation and a CHA2DS2-VASc score of 1. J. Am. Coll. Cardiol. 65, 225–232 (2015).
Olesen, J. B. et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ 342, d124 (2011).
de Bruijn, R. F. et al. Association between atrial fibrillation and dementia in the general population. JAMA Neurol. 72, 1288–1294 (2015).
Miyasaka, Y. et al. Risk of dementia in stroke-free patients diagnosed with atrial fibrillation: data from a community-based cohort. Eur. Heart J. 28, 1962–1967 (2007).
Liao, J. N. et al. Risk and prediction of dementia in patients with atrial fibrillation — a nationwide population-based cohort study. Int. J. Cardiol. 199, 25–30 (2015).
Horstmann, S. et al. Atrial fibrillation and prestroke cognitive impairment in stroke. J. Neurol. 261, 546–553 (2014).
Bunch, T. J. et al. Atrial fibrillation is independently associated with senile, vascular, and Alzheimer's dementia. Heart Rhythm 7, 433–437 (2010).
Dublin, S. et al. Atrial fibrillation and risk of dementia: a prospective cohort study. J. Am. Geriatr. Soc. 59, 1369–1375 (2011).
Forti, P. et al. Atrial fibrillation and risk of dementia in non-demented elderly subjects with and without mild cognitive impairment (MCI). Arch. Gerontol. Geriatr. 44 (Suppl. 1), 155–165 (2007).
Rusanen, M. et al. Heart diseases and long-term risk of dementia and Alzheimer's disease: a population-based CAIDE study. J. Alzheimers Dis. 42, 183–191 (2014).
Wang, T. J. et al. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation 107, 2920–2925 (2003).
Miyasaka, Y. et al. Incidence and mortality risk of congestive heart failure in atrial fibrillation patients: a community-based study over two decades. Eur. Heart J. 27, 936–941 (2006).
Schnabel, R. B. et al. Risk assessment for incident heart failure in individuals with atrial fibrillation. Eur. J. Heart Fail. 15, 843–849 (2013).
Meyer, S. et al. Sex differences in new-onset heart failure. Clin. Res. Cardiol. 104, 342–350 (2015).
Stewart, S., Hart, C. L., Hole, D. J. & McMurray, J. J. V. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am. J. Med. 113, 359–364 (2002).
Fukuda, T. et al. Development of congestive heart failure in Japanese patients with atrial fibrillation. Circ. J. 71, 308–312 (2007).
Goyal, A. et al. Predictors of incident heart failure in a large insured population: a one million person-year follow-up study. Circ. Heart Fail. 3, 698–705 (2010).
Andersson, T. et al. Gender-related differences in risk of cardiovascular morbidity and all-cause mortality in patients hospitalized with incident atrial fibrillation without concomitant diseases: a nationwide cohort study of 9519 patients. Int. J. Cardiol. 177, 91–99 (2014).
Potpara, T. S. et al. A 12-year follow-up study of patients with newly diagnosed lone atrial fibrillation: implications of arrhythmia progression on prognosis: the Belgrade Atrial Fibrillation study. Chest 141, 339–347 (2012).
Soliman, E. Z. et al. Atrial fibrillation and the risk of myocardial infarction. JAMA Intern. Med. 174, 107–114 (2014).
O'Neal, W. T., Sangal, K., Zhang, Z. M. & Soliman, E. Z. Atrial fibrillation and incident myocardial infarction in the elderly. Clin. Cardiol. 37, 750–755 (2014).
Chao, T. F. et al. Acute myocardial infarction in patients with atrial fibrillation with a CHA2DS2-VASc score of 0 or 1: a nationwide cohort study. Heart Rhythm 11, 1941–1947 (2014).
Miyasaka, Y. et al. Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based study. J. Am. Coll. Cardiol. 49, 986–992 (2007).
Chen, L. Y. et al. Atrial fibrillation and the risk of sudden cardiac death: the Atherosclerosis Risk In Communities study and Cardiovascular Health Study. JAMA Intern. Med. 173, 29–35 (2013).
Conen, D. et al. Risk of death and cardiovascular events in initially healthy women with new-onset atrial fibrillation. JAMA 305, 2080–2087 (2011).
Stollberger, C., Winkler-Dworak, M., Finsterer, J., Hartl, E. & Chnupa, P. Factors influencing mortality in atrial fibrillation. Post hoc analysis of an observational study in outpatients. Int. J. Cardiol. 103, 140–144 (2005).
Marijon, E. et al. Causes of death and influencing factors in patients with atrial fibrillation: a competing-risk analysis from the randomized evaluation of long-term anticoagulant therapy study. Circulation 128, 2192–2201 (2013).
Olsson, L. G., Swedberg, K., Lappas, G., Stewart, S. & Rosengren, A. Trends in mortality after first hospitalization with atrial fibrillation diagnosis in Sweden 1987 to 2006. Int. J. Cardiol. 170, 75–80 (2013).
Stollberger, C. et al. Mortality and rate of stroke or embolism in atrial fibrillation during long-term follow-up in the embolism in left atrial thrombi (ELAT) study. Clin. Cardiol. 27, 40–46 (2004).
Nieuwlaat, R. et al. Prognosis, disease progression, and treatment of atrial fibrillation patients during 1 year: follow-up of the Euro Heart Survey on atrial fibrillation. Eur. Heart J. 29, 1181–1189 (2008).
Gallego, P. et al. Cessation of oral anticoagulation in relation to mortality and the risk of thrombotic events in patients with atrial fibrillation. Thromb. Haemost. 110, 1189–1198 (2013).
Banerjee, A. et al. Pattern of atrial fibrillation and risk of outcomes: the Loire Valley Atrial Fibrillation Project. Int. J. Cardiol. 167, 2682–2687 (2013).
Zubaid, M. et al. Management and 1-year outcomes of patients with atrial fibrillation in the Middle East: Gulf survey of atrial fibrillation events. Angiology 66, 464–471 (2015).
Badheka, A. O. et al. Influence of obesity on outcomes in atrial fibrillation: yet another obesity paradox. Am. J. Med. 123, 646–651 (2010).
Emdin, C. A. et al. Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: systematic review and meta-analysis of cohort studies. BMJ 532, h7013 (2016).
Mosca, L., Barrett-Connor, E. & Kass Wenger, N. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation 124, 2145–2154 (2011).
Rahman, F., Kwan, G. F. & Benjamin, E. J. Global epidemiology of atrial fibrillation. Nat. Rev. Cardiol. 11, 639–654 (2014).
Nattel, S. New ideas about atrial fibrillation 50 years on. Nature 415, 219–226 (2002).
Gowd, B. M. & Thompson, P. D. Effect of female sex on cardiac arrhythmias. Cardiol. Rev. 20, 297–303 (2012).
Apostolakis, S., Sullivan, R. M., Olshansky, B. & Lip, G. Y. Hormone replacement therapy and adverse outcomes in women with atrial fibrillation: an analysis from the atrial fibrillation follow-up investigation of rhythm management trial. Stroke 45, 3076–3079 (2014).
Schnabel, R. B. et al. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort study. Lancet 373, 739–745 (2009).
Schnabel, R. B. et al. Relations of biomarkers of distinct pathophysiological pathways and atrial fibrillation incidence in the community. Circulation 121, 200–207 (2010).
Acknowledgements
D.K. is supported by the National Heart, Lung, and Blood Institute award 5T32HL007224-38 and the National Institutes of Health Clinical and Translational Science Award programme award UL1-TR000157. R.B.S. is supported by European Research Council under the European Union's Horizon 2020 research and innovation programme (agreement No 648131), and Junior Research Alliance symAtrial project funded by the German Ministry of Research and Education (BMBF 01ZX1408A) e:Med – Systems Medicine programme and by Deutsche Forschungsgemeinschaft (German Research Foundation) Emmy Noether Program SCHN 1149/3-1. E.J.B. is supported in part through NIH/NHLBI HHSN268201500001I; N01-HC25195, 2R01HL092577, 1R01 HL102214, 1R01HL128914, and 1RC1HL101056. I.E.C. is supported by a mobility grant from the Research Council of Norway (240149/F20).
Author information
Authors and Affiliations
Contributions
D.K., F.R., E.J.B., and I.E.C. researched data for the article, discussed its content, and wrote, reviewed and edited the manuscript before submission. X.Y. researched data for the article. R.B.S. discussed the content of the article, and wrote, reviewed, and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary information S1 (table)
Incidence of AF in women and men, age-pooled (PDF 71 kb)
Supplementary information S2 (table)
Incidence of AF in women and men, age-specific (PDF 117 kb)
Supplementary information S3 (table)
Prevalence of AF in women and men, age-pooled (PDF 82 kb)
Supplementary information S4 (table)
Prevalence of AF in women and men, age-specific (PDF 204 kb)
Supplementary information S5 (table)
Genetics (PDF 82 kb)
Supplementary information S6 (table)
Stroke and thromboembolism (PDF 188 kb)
Supplementary information S7 (table)
Dementia (PDF 58 kb)
Supplementary information S8 (table)
Heart failure (PDF 85 kb)
Supplementary information S9 (table)
Myocardial infarction (PDF 67 kb)
Supplementary information S10 (table)
Mortality (PDF 119 kb)
Supplementary information S11 (table)
Search strategies (PDF 76 kb)
Rights and permissions
About this article
Cite this article
Ko, D., Rahman, F., Schnabel, R. et al. Atrial fibrillation in women: epidemiology, pathophysiology, presentation, and prognosis. Nat Rev Cardiol 13, 321–332 (2016). https://doi.org/10.1038/nrcardio.2016.45
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2016.45
This article is cited by
-
Atrial fibrillation patterns and their cardiovascular risk profiles in the general population: the Rotterdam study
Clinical Research in Cardiology (2023)
-
Heart rate variability and atrial fibrillation in the general population: a longitudinal and Mendelian randomization study
Clinical Research in Cardiology (2023)
-
Efficacy of mobile health-technology integrated care based on the ‘Atrial fibrillation Better Care’ (ABC) pathway in relation to sex: a report from the mAFA-II randomized clinical trial
Internal and Emergency Medicine (2023)
-
Atrial fibrillation prediction by combining ECG markers and CMR radiomics
Scientific Reports (2022)
-
Atrial Fibrillation in Women: from Epidemiology to Treatment
Current Cardiovascular Risk Reports (2022)